Abstract
Invasive aspergillosis is a serious infectious complication, which can occur after hematopoietic stem cell transplantation (HSCT). In particular, despite antifungal treatment, invasive aspergillosis involving the central nervous system (CNS) shows very high mortality. In principle, a neurosurgical procedure with an antifungal agent is recommended for treatment of CNS invasive aspergillosis. We encountered a patient suffering from disseminated invasive aspergillosis involving the lung, brain, and soft tissues after allogeneic HSCT for treatment of relapsed acute myeloid leukemia who was cured with voriconazole and stereotactic drainage of the brain abscess.
Development of invasive aspergillosis (IA) often occurs in patients who are under immune-compromised conditions, such as hematologic disorders, organ transplantation, and prolonged use of steroids. Recently, due to the growing number of patients undergoing intensive chemotherapy and immunotherapy, the incidence of invasive aspergillosis has increased [1, 2]. Despite efforts towards an early diagnosis and use of powerful antifungal agents, IA involving the central nervous system (CNS) is known to be fatal, and its mortality is greater than 90 percent [3]. In general, in order to overcome the difficulty of drug penetration to the CNS, surgical intervention in addition to an antifungal agent is recommended [4-6]. However, in many cases, a surgical approach is often unavailable due to cytopenia or poor performance status.
We experienced a case of IA involving the lung, brain, and soft tissues after allogeneic hematopoietic stem cell transplantation (HSCT) in a patient with acute myeloid leukemia (AML) who was treated successfully with voriconazole and stereotactic aspiration of the brain abscess.
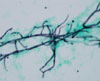
A 31-year-old female patient who received allogeneic hematopoietic stem cell transplantation (HSCT) for treatment of relapsed acute myeloid leukemia (AML) was admitted because of cough and fever on day 67 after transplantation. She was on cyclosporine for prophylaxis of graft-versus-host disease. Initially, her vital signs included blood pressure of 115/80 mmHg, heart rate of 120/min, respiratory rate of 18/min, and body temperature 37.5℃. Crackle was auscultated at the left lower lung field, and multiple ulcerative skin lesions and subcutaneous nodules were observed on the face, limb, breast, trunk, and extremities (Fig. 1). Findings on chest roentgenogram and computed tomogram showed multiple pneumonic consolidations in both lungs and a large cavitary lesion in the left lower lobe, suggesting disseminated IA (Fig. 2A). She presented with a white blood cell count of 2,420/mm3, platelets of 12,000/mm3, and hemoglobin of 9.4 g/dL. Results of chemistry examination showed total protein of 6.0 g/dL, albumin of 3.6 g/dL, aspartate transaminase of 21 IU/L, alanine transaminase of 63 IU/L, total billirubin of 1.6 mg/dL, lactated dehydrogenase of 582 IU/L, blood urea nitrogen of 38.8 mg/dL, creatinine of 0.9 mg/dL, C-reactive protein (CRP) of 32.5 mg/dL, and erythrocyte sedimentation rate of 103 mm/hr. Serum galactomannan test was positive, with an index value of 4.6. We performed biopsy of the skin nodule; however, the result showed non-specific inflammation with necrosis. Repeated biopsy was refused by the patient. We immediately started empiric antibiotics with amphotericin B of 1 mg/kg/day, however, her clinical symptoms and signs did not show improvement. After two weeks of antimicrobial treatment, she developed an abrupt headache, visual field defect, and septic shock; therefore, brain MRI was performed. Multifocal masses were observed in both cerebral hemispheres (Fig. 3A), and we changed the antifungal agent from amphotericin B to intravenous voriconazole. After intravenous administration of voriconazole, the septic shock, pneumonia, and subcutaneous nodules showed improvement. However, the brain lesions showed only a slight decrease, with formation of abscess cavities on follow up brain MRI. Using a stereotactic approach, we performed aspiration of the cerebral abscesses on day 50 of voriconazole treatment after recovery of thrombocytopenia. Necrotic tissue and hyphae consistent with aspergillus were observed in the aspiration material (Fig. 4). Tissue culture was performed; however, detail species of fungus was not identified eventually. After drainage of the cerebral abscesses and continuous administration of voriconazole, the patient's clinical symptoms and signs showed dramatic improvement, except for the visual field defect (Fig. 2B, 3B). Galatomanan test converted to negative after four weeks of use of voriconazole. We completed the antifungal treatment under near remission of lung and brain lesions after two weeks of use of intravenous voriconazole 200 mg every 12 hr and five months of oral voriconazole 200 mg bid. She has been followed up at an outpatient clinic without occurrence of any serious events for over one year.
The most common underlying conditions of IA include AML, malignant lymphoma, and chronic myeloid leukemia, and the most commonly involved organs are the lung, brain, heart, and alimentary tract [7, 8]. Primary CNS aspergillosis is very rare [9], and most CNS aspergillosis is disseminated by the blood stream from pulmonary aspergillosis. Uncommon fungi including Pseudallescheria Boydii, Scedosporium prolifican and dark-walled fungi should be considered in CNS fungal infection that is not confirmed by culture or biopsy [10].
Voriconazole is the treatment of choice for CNS aspergillosis, and itraconzole, posaconazole, and liposomal amphotericin are considered for intolerant or refractory cases. Few studies supporting the use of echinocandins as a single agent in salvage treatment of CNS aspergillosis have been reported. Combination therapy with voriconazole and caspofungin has been used anecdotally for treatment of CNS aspergillosis [11-13]. In terms of pharmacokinetics, due to their large molecular size of over 700 Dalton, amphotericin B, echinocandins, itraconazole, and posaconazole have the limitation of CNS penetration. Although fluconazole and 5-fluorocytosine penetrate the CNS, they have a narrow spectrum of antifungal activity. In contrast, due to its smaller size of 349 dalton and lipophilic characteristic, voriconazole has broad antifungal activity and is able to penetrate the CNSE. It has been repeatedly reported that the peak level of voriconazole in cerebrospinal fluid is over 1 lg/mL, and concentration in human brain tissue or brain abscess material exceeds over 1 lg/g [12]. The practice of intrathecal or intralesional antifungal chemotherapy is not recommended for treatment of CNS aspergillosis. In addition, corticosteroids can be deleterious and should be avoided whenever possible [11]. For these reasons, voriconazole is regarded as the optimal agent for treatment of CNS aspergillosis.
Surgical resection or intervention is also important in treatment of CNS aspergillosis. Surgical resection of lesions can be the definitive treatment and prevent serious neurological sequelae. Patients receiving those neurosurgical interventions showed significantly higher response rates compared to those without/unknown neurosurgery (60% vs. 42%) [14]. However, if surgical resection is impossible due to bleeding tendency or poor condition, a stereotactic neurosurgical procedure for drainage of the intracranial fungal abscess can contribute to improvement of infection [15]. In our case, we performed stereotactic aspiration for drainage of the intracranial fungal abscess instead of surgical resection because of thrombocytopenia and poor general condition.
In conclusion, we experienced a case of disseminated IA with multiple brain abscesses after allogeneic HSCT in a patient with AML who was cured by use of a multimodality approach. CNS IA after allogeneic HSCT is rare, and the treatment outcome is very poor. In this situation, intensive treatment with voriconazole and surgical resection or intervention should be considered.
Figures and Tables
 | Figure 2(A) Chest CT at diagnosis of invasive pulmonary aspergillosis; There was a cavitary lesion with abscess in left lower lung. (B) After treatment with voriconazole for 150 days, the lesion is much improved. |
References
1. Maschmeyer G, Haas A, Cornely OA. Invasive aspergillosis: epidemiology, diagnosis and management in immunocompromised patients. Drugs. 2007. 67:1567–1601.
2. Lass-Flörl C. The changing face of epidemiology of invasive fungal diseases in Europe. Mycoses. 2009. 52:197–205.
3. Denning DW, Stevens DA. Antifungal and surgical treatment of invasive aspergillosis: review of 2,121 published cases. Rev Infect Dis. 1990. 12:1147–1201.

4. Kasper EM, Bartek J Jr, Johnson S, Kasper BS, Pavlakis M, Wong M. Posttransplant aspergillosis and the role of combined neurosurgical and antifungal therapies under belatacept immunosuppression. Surg Neurol Int. 2011. 2:75.
5. Coleman JM, Hogg GG, Rosenfeld JV, Waters KD. Invasive central nervous system aspergillosis: cure with liposomal amphotericin B, itraconazole, and radical surgery-case report and review of the literature. Neurosurgery. 1995. 36:858–863.
6. Henze G, Aldenhoff P, Stephani U, Grosse G, Kazner E, Staib F. Successful treatment of pulmonary and cerebral aspergillosis in an immunosuppressed child. Eur J Pediatr. 1982. 138:263–265.

7. Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Park SW, Choe YJ, Oh MD, Choe KW. Clinical manifestations and treatment outcome of invasive aspergillosis. Korean J Infect Dis. 2002. 34:160–166.
8. Meyer RD, Young LS, Armstrong D, Yu B. Aspergillosis complicating neoplastic disease. Am J Med. 1973. 54:6–15.

9. Chae KS, Eun JP. A case of multiple intracerebral aspergillus abscess in neonate. Infect Chemother. 2004. 36:122–126.
10. Mandell GL, Douglas RG, Bennett JE, editors. Principles and practice of infectious disease. 2009. 7th ed. Philadelphia: Churchill Livingstone;3365–3369.
11. Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, Morrison VA, Segal BH, Steinbach WJ, Stevens DA, van Burik JA, Wingard JR, Patterson TF. Infectious Diseases Society of America. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008. 46:327–360.

12. Schwartz S, Thiel E. Cerebral aspergillosis: tissue penetration is the key. Med Mycol. 2009. 47:Suppl 1. S387–S393.

13. Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, Kern WV, Marr KA, Ribaud P, Lortholary O, Sylvester R, Rubin RH, Wingard JR, Stark P, Durand C, Caillot D, Thiel E, Chandrasekar PH, Hodges MR, Schlamm HT, Troke PF, de Pauw B. Invasive Fungal Infections Group of the European Organisation for Research and Treatment of Cancer and the Global Aspergillus Study Group. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002. 347:408–415.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download