Abstract
Background
Recent data regarding the clinical epidemiologic characteristics of Mycoplasma pneumoniae pneumonia in Korean adults are insufficient. This study was conducted in order to compare epidemics in different ages and to identify the clinical characteristics in adults.
Material and Methods
We investigated patients who visited Korea University Guro Hospital from January to December 2011 due to community acquired pneumonia and underwent mycoplasma antibody tests. M. pneumoniae pneumonia was diagnosed if mycoplasma antibody titer was ≥1:320 at any time, seroconversion or 4-fold rise was seen at convalescent phase. Patients under the age of 19 were classified as child and adolescent, otherwise adult. We investigated the number of monthly cases in all patients and reviewed the medical records of adult patients.
Results
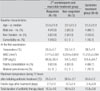
A total of 249 young patients aged ≤18 years and 29 adults were diagnosed with M. pneumoniae pneumonia. Among young patients, 75.5% were concentrated in the 0-6 years age group and 58.6% of adults belonged to the 26-40 years age group. The number of young patients began to increase in July and continued to increase in December, while the number of adult patients began to increase in August and occurred continuously until December. The correlation coefficient of the epidemic trend between the two groups was 0.682 (P=0.015). Median age of adult patients was 33.3 years. Fever was observed in all patients and 25 patients (86.2%) complained of purulent sputum. The average white blood cell count was 7,066/mm3. The average values for aspartate aminotransferase, alanine aminotransferase, creatinine, and sodium were within the normal range. In chest X-ray study, ipsilateral lower patchy consolidation was found in 24 patients (82.8%). Twenty one adult patients (72.4%) were hospitalized. The mean duration of hospitalization was 7.3 days. Twenty three patients (79.3%) were initially treated with combinations of third generation cephalosporin and macrolide. Among them, five patients (17.2%) showed poor responses. Six cases (20.7%) were initially treated with quinolone, and treatment was maintained until the end without changing antibiotics. Development of cryptogenic organizing pneumonia occurred in one case and there was no occurrence of death.
Conclusions
When M. pneumoniae pneumonia is epidemic among children and adolescents, it should also be suspected in adult patients with community-acquired pneumonia. Some patients showed poor responses to macrolide. Overall, it appears that additional studies are needed for evaluation of the effectiveness of macrolide in treatment of M. pneumoniae pneumonia in adults.
Figures and Tables
Figure 1
Number of Mycoplasma pneumoniae pneumonia patients according to the age distribution during the study period (January 2011-Deccember 2011).

Figure 2
Monthly distribution of number of Mycoplasma pneumoniae pneumonia patients according to age group during the study period (January 2011-December 2011).

References
1. Denny FW, Clyde WA Jr, Glezen WP. Mycoplasma pneumoniae disease: clinical spectrum, pathophysiology, epidemiology, and control. J Infect Dis. 1971. 123:74–92.

2. Kim JW, Seo HK, Yoo EG, Park SJ, Yoon SH, Jung HY, Han MY. Mycoplasma pneumoniae pneumonia in Korean children, from 1979 to 2006-a meta-analysis. Korean J Pediatr. 2009. 52:315–323.

3. Chong YP, Jung KS, Lee KH, Kim MN, Moon SM, Park S, Hur J, Kim DM, Jeon MH, Woo JH. The bacterial etiology of community-acquired pneumonia in Korea: a nationwide prospective multicenter study. Infect Chemother. 2010. 42:397–403.

4. Foy HM, Kenny GE, Cooney MK, Allan ID. Long-term epidemiology of infections with Mycoplasma pneumoniae. J Infect Dis. 1979. 139:681–687.

5. Mansel JK, Rosenow EC 3rd, Smith TF, Martin JW Jr. Mycoplasma pneumoniae pneumonia. Chest. 1989. 95:639–646.

7. Clyde WA Jr. Clinical overview of typical Mycoplasma pneumoniae infections. Clin Infect Dis. 1993. 17:Suppl 1. S32–S36.
8. Marrie TJ. Mycoplasma pneumoniae pneumonia requiring hospitalization, with emphasis on infection in the elderly. Arch Intern Med. 1993. 153:488–494.

9. Isozumi R, Yoshimine H, Morozumi M, Ubukata K, Ariyoshi K. Adult community-acquired pneumonia caused by macrolide resistant Mycoplasma pneumoniae. Respirology. 2009. 14:1206–1208.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download