Abstract
Background
Local epidemiologic data on prevalent pathogens are important to guide empirical antibiotic therapy. In this study, we observed annual changes in frequency of occurrence and in vitro antimicrobial susceptibility of blood isolates over a period of 13 years.
Materials and Methods
We reviewed blood isolates identified during the period from 1998 to 2010 at Seoul National University Hospital. Only first isolates for each patient were included in the analysis. We analyzed the frequency of isolates and their trend with regard to in vitro antimicrobial susceptibility. Data were presented according to guidelines of the Clinical and Laboratory Standards Institute (CLSI) (2009).
Results
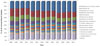
A total of 23,501 isolates were identified during the period from 1998 to 2010. Fifty-five percent of the isolates were gram-positive cocci, 38% were gram-negative rods, and 3% were fungi. Coagulase-negative Staphylococcus (CoNS) (24%), Escherichia coli (16%), Staphylococcus aureus (10%), and Klebsiella pneumoniae (8%) were the most commonly isolated bacteria, and Candida albicans (2%) was the most commonly isolated fungus. The frequency of CoNS increased from 18.0% to 26.8%, whereas the frequency of E. coli and K. pneumoniae decreased from 20.2% to 13.7% and from 11.7% to 6.7%, respectively. Overall, the proportion of methicillin-resistant S. aureus changed from 47.9% to 62.1%. In E. coli, the resistance rate of cefotaxime and ciprofloxacin increased over a period of 13 years. However, such an increase of resistance was not observed in K. pneumoniae. In P. aeruginosa, and particularly in A. baumannii, resistance to imipenem rose alarmingly (3% in 1998 to 27.8% in 2010, 5% in 1998 to 68.9% in 2010, respectively).
Conclusions
Over the last 13 years, the proportion of CoNS in blood isolates increased, which led to a relative decrease of isolated gram-negative rods. Proportions of MRSA showed no significant change, whereas cefotaxime resistant and ciprofloxacin resistant E. coli increased. Imipenem resistant P. aeruginosa and A. baumannii also increased during the study period.
Figures and Tables
 | Figure 213-year trend of S. aureus for % resistant to ciprofloxacin, oxacillin, rifampin, cotrimoxazole, vancomycin. CIP, ciprofloxacin; OXA, oxacillin; RIF, rifampin; SXT, cotrimoxazole; VAN, vancomycin; %R, %resistant. |
 | Figure 313-year trend of E. faecium and E. faecalis for % resistant to ampicillin and vancomycin. EFA, E. faecalis ; EFM, E. faecium; AMP, ampicillin; VAN, vancomycin; %R, %resistant. |
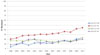 | Figure 413-year trend of E. coli and K. pneumoniae for % resistant to ceftriaxone and ciprofloxacin. ECO, E. coli; KPN, K. pneumoniae; CTX, cefotaxime; CIP, ciprofloxacin; %R, %resistant. |
References
1. Weinstein MP, Towns ML, Quartey SM, Mirrett S, Reimer LG, Parmigiani G, Reller LB. The clinical significance of positive blood cultures in the 1990s: a prospective comprehensive evaluation of the microbiology, epidemiology, and outcome of bacteremia and fungemia in adults. Clin Infect Dis. 1997. 24:584–602.

2. Leibovici L, Shraga I, Drucker M, Konigsberger H, Samra Z, Pitlik SD. The benefit of appropriate empirical antibiotic treatment in patients with bloodstream infection. J Intern Med. 1998. 244:379–386.

3. Kang CI, Kim SH, Kim HB, Park SW, Choe YJ, Oh MD, Kim EC, Choe KW. Pseudomonas aeruginosa bacteremia: risk factors for mortality and influence of delayed receipt of effective antimicrobial therapy on clinical outcome. Clin Infect Dis. 2003. 37:745–751.

4. Biedenbach DJ, Moet GJ, Jones RN. Occurrence and antimicrobial resistance pattern comparisons among bloodstream infection isolates from the SENTRY Antimicrobial Surveillance Program (1997-2002). Diagn Microbiol Infect Dis. 2004. 50:59–69.

5. Decousser JW, Lamy B, Pina P, Allouch PY. Collège de Bactériologie Virologie Hygiène Study Group (ColBVH). Trends in antibiotic susceptibility of bloodstream pathogens in hospitalized patients in France, 1996 to 2007. Diagn Microbiol Infect Dis. 2010. 66:292–300.

6. Raveh D, Rudensky B, Schlesinger Y, Benenson S, Yinnon AM. Susceptibility trends in bacteraemias: analyses of 7544 patient-unique bacteraemic episodes spanning 11 years (1990-2000). J Hosp Infect. 2003. 55:196–203.

7. Fluit AC, Jones ME, Schmitz FJ, Acar J, Gupta R, Verhoef J. Antimicrobial susceptibility and frequency of occurrence of clinical blood isolates in Europe from the SENTRY antimicrobial surveillance program, 1997 and 1998. Clin Infect Dis. 2000. 30:454–460.

8. Streit JM, Jones RN, Sader HS, Fritsche TR. Assessment of pathogen occurrences and resistance profiles among infected patients in the intensive care unit: report from the SENTRY Antimicrobial Surveillance Program (North America, 2001). Int J Antimicrob Agents. 2004. 24:111–118.

9. Asensio A, Alvarez-Espejo T, Fernandez-Crehuet J, Ramos A, Vaque-Rafart J, Bishopberger C, Hernandez Navarrete M, Calbo-Torrecillas F, Campayo J, Canton R. Estudio de Prevalencia de las Infecciones Nosocomiales en Espana (EPINE) Working Group. Trends in yearly prevalence of third-generation cephalosporin and fluoroquinolone resistant Enterobacteriaceae infections and antimicrobial use in Spanish hospitals, Spain, 1999 to 2010. Euro Surveill. 2011. 16:19983.

10. Ahn GY, Jang Sj, Lee SH, Jeong OY, Chaulagain BP, Moon DS, Park YJ. Trends of the species and antimicrobial susceptibility of microorganisms isolated from blood cultures of patients. Korean J Clin Microbiol. 2006. 9:42–50.
11. Kang BK, Lee HJ, Suh JT. The trends of the species and antimicrobial susceptibility of bacteria and fungi isolated from blood cultures (1986-1996). Korean J Clin Pathol. 1998. 18:57–64.
12. Kim HJ, Lee NY, Kim S, Shin JH, Kim MN, Kim EC, Koo SH, Ryoo NH, Kim JS, Cho JH. Characteristics of microorganisms isolated from blood cultures at nine university hospitals in Korea during 2009. Korean J Clin Microbiol. 2011. 14:48–54.

13. Kim SY, Lim G, Kim MJ, Suh JT, Lee HJ. Trends in five-year blood cultures of patients at a university hospital (2003~2007). Korean J Clin Microbiol. 2009. 12:163–168.

14. Koh EM, Lee SG, Kim CK, Kim M, Yong D, Lee K, Kim JM, Kim DS, Chong Y. Microorganisms isolated from blood cultures and their antimicrobial susceptibility patterns at a university hospital during 1994-2003. Korean J Lab Med. 2007. 27:265–275.

15. Park Y, Lee Y, Kim M, Choi JY, Yong D, Jeong SH, Kim JM, Lee K, Chong Y. Recent trends of anaerobic bacteria isolated from clinical specimens and clinical characteristics of anaerobic bacteremia. Infect Chemother. 2009. 41:216–223.

16. Kang CI, Kim DM, Yi JY, Park WB, Lee KD, Kim HB, Oh MD, Kim EC, Choe KW. Antimicrobial susceptibility of Escherichia coli and Klebsiella pneumoniae blood isolates over 5 years: Influence of extended-spectrum beta-lactamase-producing organisms. Infect Chemother. 2003. 35:365–369.
17. CLSI. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-First Informational Supplement M100-S21. 2011. 31.
18. CLSI. Analysis and Presentation of Cumulative Antimicrobial Susceptibility Test Data; Approved Guideline - Third Edition. M39-A3. 2009. 29.
19. Arpi M, Victor MA, Møller JK, Jønsson V, Hansen MM, Peterslund NA, Bruun B. Changing etiology of bacteremia in patients with hematological malignancies in Denmark. Scand J Infect Dis. 1994. 26:157–162.

20. Falagas ME, Kasiakou SK, Nikita D, Morfou P, Georgoulias G, Rafailidis PI. Secular trends of antimicrobial resistance of blood isolates in a newly founded Greek hospital. BMC Infect Dis. 2006. 6:99.

21. Worth LJ, Slavin MA. Bloodstream infections in haematology: risks and new challenges for prevention. Blood Rev. 2009. 23:113–122.

22. Weinstein MP. Blood culture contamination: persisting problems and partial progress. J Clin Microbiol. 2003. 41:2275–2278.

23. Mirrett S, Weinstein MP, Reimer LG, Wilson ML, Reller LB. Relevance of the number of positive bottles in determining clinical significance of coagulase-negative staphylococci in blood cultures. J Clin Microbiol. 2001. 39:3279–3281.

24. Weinstein MP, Mirrett S, Van Pelt L, McKinnon M, Zimmer BL, Kloos W, Reller LB. Clinical importance of identifying coagulase-negative staphylococci isolated from blood cultures: evaluation of MicroScan Rapid and Dried Overnight Gram-Positive panels versus a conventional reference method. J Clin Microbiol. 1998. 36:2089–2092.

25. Favre B, Hugonnet S, Correa L, Sax H, Rohner P, Pittet D. Nosocomial bacteremia: clinical significance of a single blood culture positive for coagulase-negative staphylococci. Infect Control Hosp Epidemiol. 2005. 26:697–702.

26. Chung G, Cha J, Han S, Jang H, Lee K, Yoo J, Yoo J, Kim H, Eun S, Kim B, Park O, Lee Y. Nationwide surveillance study of vancomycin intermediate Staphylococcus aureus strains in Korean hospitals from 2001 to 2006. J Microbiol Biotechnol. 2010. 20:637–642.
27. Kim MN. Multidrug-resistant Organisms and Healthcare-associated Infections. Hanyang Med Rev. 2011. 31:141–152.

28. Karlowsky JA, Jones ME, Thornsberry C, Friedland IR, Sahm DF. Trends in antimicrobial susceptibilities among Enterobacteriaceae isolated from hospitalized patients in the United States from 1998 to 2001. Antimicrob Agents Chemother. 2003. 47:1672–1680.

29. Peleg AY, Hooper DC. Hospital-acquired infections due to gram-negative bacteria. N Engl J Med. 2010. 362:1804–1813.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download