Abstract
While Raoultella planticola is a rare cause of human infection, we experienced a case of severe cholangitis caused by R. planticola. A 75-year-old male patient with cancer of the pancreatic head was admitted and found to have cholangitis. Following performance of percutaneous transhepatic biliary drainage for decompression and initiation of empirical antibiotics with cefotaxime and metronidazole. R. planticola, which was susceptible to cefotaxime, was isolated from both bile and blood. Despite administration of prompt and appropriate antibiotic therapy, the patient died 10 days after admission. We herein describe the first case of cholangitis caused by infection with R. planticola.
Raoultella planticola, a gram-negative non-motile bacillus, was formerly identified as a member of the Klebsiella genus and reclassified as the Raultella genus in 2001 [1]. Although R. planticola has been regarded as an environmental bacterium, five cases of human infection caused by this organism have been reported since 1984 [2-6]. However, no case of cholangitis due to infection with this organism has been reported. We recently experienced a case of fatal cholangitis caused by infection with R. planticola in a 75-year-old male patient with pancreatic cancer.
In November 2010, a 75-year-old male patient was admitted to Korea University Ansan Hospital with fever and jaundice. The patient had been diagnosed with cancer of the pancreatic head three months earlier. Chemotherapy or radiotherapy was recommended; however, the patient and his family refused curative treatment, and only conservative management was applied. On admission, his body temperature was 38.4℃ and systolic blood pressure was below 90 mmHg. Results of initial laboratory tests were as follows: white blood cell count, 13,110/µL; aspartate aminotransferase, 59 IU/L; alanine aminotransferase, 62 IU/L; alkaline phosphatase, 259 IU/L; gamma-glutamyltransferase, 160 IU/L; total bilirubin, 22.2 mg/dL; direct bilirubin, 15.8 mg/dL; C-reactive protein, 15.4 mg/dL; erythrocyte sedimentation rate 105 mm/hr; blood urea nitrogen, 132 mg/dL; and serum creatinine, 4.6 mg/dL. A low attenuation mass, measuring 3.6×3.2 cm, on the head portion of the pancreas, which grew larger, when compared with the previous image (3.1×2.8 cm), was observed on abdominal computed tomography scan. In an attempt to control his septic condition, the patient was transferred to the intensive care unit. Due to blockage of the bile duct, percutaneous transhepatic biliary drainage was performed for decompression. Blood and bile cultures taken at the time of admission yielded R. planticolla, which was identified with a 93% probability, using the VITEK-2 (bioMérieux Inc., Marcy lÉtoile, France) biochemical identification system. According to results of the antibiotic susceptibility test, R. planticolla showed resistance to ampicillin and piperacillin, but susceptibility to cephalothin, cefoxitin, cefotaxime, cefepime, aztreonam, imipenem, amikacin, levofloxacin, and trimethoprim/sulfamethoxazol. Despite administration of prompt and appropriate antibiotic therapy, fluid resuscitation, vasopressor, and inotropic agents, the patient's condition did not show improvement. Fever persisted with increasing leukocytosis up to 33,800/mm3, and he eventually demonstrated greater hemodynamic instability on day four of hospitalization. On day eight, a Gram-positive organism was isolated from the patient's blood, indicating suspicion of central catheter-related bloodstream infection (CR-BSI); therefore, vancomycin was added.
However, the patient's condition showed progressive deterioration and he died of multiple organ failure on day 10 of hospitalization.
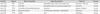
Since description of the first case of R. planticola septicemia by Freney in 1984 [2], four additional cases of human infection have been reported (Table 1); one case of post-operative infection [3], one case of pancreatitis with retroperitoneal abscess [4], one case involving surgical site infection [5], and, the most recent case, primary soft tissue infection [6]. However, cholangitis caused by infection with this organism has not yet been reported.
R. planticola was originally named Klebsiella planticola in 1981 [7]; however, its name was changed to K. trevisanii in 1983 [8]; it was then renamed K. planticola in 1986 [9]. Based on sequence analysis of the 16S rRNA and rpoB genes, a new genus, Raoultella, was proposed in 2001 [1]. R. planticola was originally regarded as an environmental bacterium, and, despite its isolation from various human specimens, the clinical significance of the organism remained uncharacterized [2, 3]. In our case, R. planticola was isolated from both blood and bile fluid, and the patient exhibited clinical features of severe sepsis due to cholangitis. While the organism was then identified with a 93% probability, using VITEK-2 (bioMérieux Inc.), evaluation of the VITEK-2 (bioMérieux Inc.) GN card for identification of Gram-negative bacilli revealed that the system had correctly identified 97.4% of the 426 isolates tested [10]. As a result, R. planticola isolated from the patient was determined to be a true pathogen of cholangitis. The patient's condition did not show any improvement from the initial throughout his entire hospital course; therefore, despite the presence of another infection, CR-BSI, the cause of his death was thought to be mainly related to cholangitis by infection with R. planticola. However, in the five previously reported cases of R. planticola infection, no case involving mortality was reported; thus, the R. planticola strain isolated from our patient could be more virulent than those of previously reported cases. Underlying malignancy and combined nosocomial infection observed in our case may also have contributed to the fatal outcome.
In conclusion, this is the first report of cholangitis caused by infection with R. planticola. This report demonstrates that, although rare, R. planticola can truly cause human infection, which can be fatal.
Figures and Tables
References
1. Drancourt M, Bollet C, Carta A, Rousselier P. Phylogenetic analyses of Klebsiella species delineate Klebsiella and Raoultella gen. nov., with description of Raoultella ornithinolytica comb. nov., Raoultella terrigena comb. nov. and Raoultella planticola comb. nov. Int J Syst Evol Microbiol. 2001. 51:925–932.

2. Freney J, Fleurette J, Gruer LD, Desmonceaux M, Gavini F, Leclerc H. Klebsiella trevisanii colonisation and septicaemia. Lancet. 1984. 1:909.
3. Freney J, Gavini F, Alexandre H, Madier S, Izard D, Leclerc H, Fleurette J. Nosocomial infection and colonization by Klebsiella trevisanii. J Clin Microbiol. 1986. 23:948–950.

4. Alves MS, Riley LW, Moreira BM. A case of severe pancreatitis complicated by Raoultella planticola infection. J Med Microbiol. 2007. 56:696–698.

5. Wolcott R, Dowd S. Molecular diagnosis of Raoultella planticola infection of a surgical site. J Wound Care. 2010. 19:329–332.

6. O'Connell K, Kelly J, Niriain U. A rare case of soft-tissue infection caused by Raoultella planticola. Case Report Med. 2010. 2010:134086.
7. Bagley ST, Seidler RJ, Brenner DJ. Klebsiella planticola sp. nov. : a new species of enterobacteriaceae found primarily in nonclinical environments. Curr Microbiol. 1981. 6:105–109.

8. Ferragut C, Izard D, Gavini F, Kersters K, Deley J, Leclerc H. Klebsiella trevisanii : a new species from water and soil. Int J Syst Bacteriol. 1983. 33:133–142.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download