Abstract
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome is a disorder which can be caused by treatment with a diverse collection of drugs, and it is characterized by fever, rash, lymphadenopathy, and internal organ involvement with eosinophilia. Although ethambutol and rifampin are popularly used to treat tuberculosis, there has been only one reported case of DRESS syndrome associated with ethambutol. DRESS syndrome associated with administration of rifampin have not been reported. In this report and discussion, we present the case of a patient suffering from DRESS syndrome induced by both ethambutol and rifampin.
Ethambutol (EMB) and rifampin (RFP) are commonly used with other drugs in the treatment of tuberculosis and are generally well-tolerated. A well known serious adverse reaction caused by EMB occurring in 1% or fewer patients is retrobulbar neuritis [1]. Common RFP-related adverse effects include fever, hepatitis, hypersensitivity and thrombocytopenia with purpura. Rare adverse skin disorders related to EMB or RFP treatment include urticaria and Steven-Johnson syndrome, as well as drug reactions with eosinophilia and systemic symptoms (DRESS) syndrome [2-4].
DRESS syndrome was first reported as exfoliative dermatitis following sulfanilamide treatment [5, 6]. This syndrome is characterized by fever, rash, lymphadenopathy, and internal organ involvement with eosinophilia [7]. Patients diagnosed with DRESS syndrome should fulfill at least three of four systemic features: a body temperature above 38℃, enlarged lymph nodes at a minimum of two sites, involvement of at least one internal organ, and clinical blood chemistry count abnormalities [8]. Commonly affected organs include the liver, lungs and kidneys. The mortality rate of this syndrome, associated with visceral involvement, is approximately 10% [9].
To our knowledge, there has been only one reported case of DRESS syndrome associated with EMB [2] and none associated with RFP. Herein, we present a rare case of DRESS syndrome induced by treatment with both EMB and RFP.
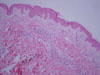
A 26-year-old female, who had been placed on anti-tuberculosis medications consisting of isoniazid (INH), RFP, pyrazinamide (PZA) and EMB for the treatment of pulmonary tuberculosis four weeks earlier, presented with a fever and rash which had persisted for a week. She had been healthy and had not suffered from any previous allergy. The skin lesion was erythematous generalized macule which involved the whole body including the palmoplantar and oral mucosa (Fig. 1). Upon admission, her temperature was 38.5℃, and cervical lymphadenopathy and hepatosplenomegaly were detected. At the time of admission, her initial laboratory results included hemoglobin of 11.6 g/dL, WBC of 22,410 cells/mm3 (differential count of eosinophil; 43% and atypical lymphocyte; 7%), platelet count of 243,000 cells/mm3, aspartate transaminase of 117 U/L, alanine transaminase of 171 U/L, total bilirubin of 1.0 mg/dL and serum creatinine of 0.6 mg/dL. Chest x-ray results showed localized infiltration on the right upper lobe with mild lobar atelectasis. A skin biopsy obtained from the abdomen revealed superficial perivascular lymphocyte infiltration (Fig. 2). All the original anti-tuberculous medications were stopped and high dose methylprednisolone (120 mg/d for 3 days) with human immunoglobulin were prescribed. As a substitute treatment for tuberculosis, levofloxacin was administered from 7 days after admission.
At her 4th week of hospitalization, 400 mg of EMB was reintroduced, as her clinical symptoms had almost completely improved. Unfortunately, immediately after taking the EMB she complained of severe dyspnea and pruritus. Erythematous macules, identical to those observed in the previous reaction, reappeared and covered her entire body. The EMB was believed to be the cause of her DRESS syndrome and it was discontinued. After 4 days, RFP was administered to the patient with an initial dose of 150 mg and gradually increased to 450 mg. However, clinical symptoms including hepatitis and eosinophilia gradually reappeared and the RFP administration was also discontinued.
When the patient's hepatitis and eosinophilia improved, one week after RFP administration had been discontinued, treatment by INH was resumed with increasing dosages from 50 to 200 mg. As no adverse drug reaction occurred after seven days of medication, PZA was added at a dose of 250 mg and increased up to 1,250 mg. Intramuscular streptomycin was also added to the regimen. The final course of anti-tuberculosis medications consisted of 200 mg of INH, 1,250 mg of PZA, 700 mg of levofloxacin, and 1 g of streptomycin, daily. This regimen was maintained for 9 months and her pulmonary tuberculosis was ultimately cured (Fig. 3).
In 1996, DRESS syndrome was named by Bocquet, et al., in an effort to decrease ambiguity in clinical practice [7]. This syndrome represents a group of severe cutaneous adverse reactions with multivisceral involvement. DRESS syndrome characteristically arises after a long latency period, typically 3 to 8 weeks after use of the offending drug [6]. In our case, symptoms developed at the 4th week after starting the anti-tuberculosis medications. Although the pathogenesis remains unclear, type IVb hypersensitivity reaction and a lack of effective drug metabolism, leading to an accumulation of harmful metabolites, are thought to play important roles in this condition [9-10]. It has also been suggested that human herpesvirus 6 infection is associated with DRESS syndrome [11].
The mortality rate with visceral involvement has been reported to be approximately 10%, with most patients dying as a result of liver failure. Typically, drugs responsible for DRESS syndrome are aromatic anticonvulsants (phenytoin, phenobarbital and carbamazepine), sulfonamide, allopurinol, etc. [2, 5, 7, 9]. Of note, EMB and RFP are not part of this list. An exhaustive review of the literature found only one case of DRESS syndrome associated with EMB, which had been confirmed by a patch test [2]. A cause-effect relationship is difficult to establish when multiple drugs are concomitantly administrated such as seen in an anti-tuberculosis regimen. We could have determined the cause-effect relationship between EMB, RFP and DRESS syndrome with our case by rechallenging. However, a provocation test such as rechallenging is not risk free. A safer alternative, the patch test may be useful in detecting the culprit from multiple drugs. If it is absolutely necessary to use a potentially causative drug, it should be administered cautiously starting with a small dose.
Prompt withdrawal of the causative agent is most important when it comes to treating DRESS syndrome because accumulation of reactive drug metabolites plays a key role in the disease pathogenesis [12]. Other treatment options include corticosteroid, human immunoglobulin and N-acetylcysteine. Systemic corticosteroid is indicated for cases with visceral involvement or life-threatening conditions, except in situations involving infection. Dramatic improvement has been reported with systemic corticosteroids [7, 9]. Human immunoglobulin and high dose N-acetylcysteine may also be used as therapies. While it is the opinion of some physicians that DRESS syndrome is associated with human herpesvirus 6 infection, the efficacy of human immunoglobulin, which results from anti-virus IgG mechanisms, is not yet fully understood [2, 11]. The effect of high dose N-acetylcysteine, a glutathione precursor, is associated with inhibition of hypersensitivity reactions [9].
In summary, this case revealed the cause-effect relationship between DRESS syndrome and EMB and RFP by rechallenging. The patient was successfully cured by prompt cessation of the culprit drugs, and the use of corticosteroid and human immunoglobulin without aggravation of the underlying tuberculosis. This paper represents the first and second report of DRESS syndrome caused by RFP and EMB, respectively. Although they are generally well-tolerated anti-tuberculosis drugs, EMB and RFP should be considered as possible causative agents of DRESS syndrome.
Figures and Tables
References
1. Takami A, Nakao S, Asakura H, Yamazaki H, Mizuhashi K, Matsuda T, Mizushima N. Pneumonitis and eosinophilia induced by ethambutol. J Allergy Clin Immunol. 1997. 100:712–713.

2. Lee JH, Park HK, Heo J, Kim TO, Kim GH, Kang DH, Song GA, Cho M, Kim DS, Kim HW, Lee CH. Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) syndrome induced by celecoxib and anti-tuberculosis drugs. J Korean Med Sci. 2008. 23:521–525.

3. Pegram PS Jr, Mountz JD, O'Bar PR. Ethambutol-induced toxic epidermal necrolysis. Arch Intern Med. 1981. 141:1677–1678.

4. Surjapranata FJ, Rahaju NN. A case of Stevens-Johnson's syndrome caused by ethambutol. Paediatr Indones. 1979. 19:195–201.

5. Ben'mrad M, Leclerc-Mercier S, Blanche P, Franck N, Rozenberg F, Fulla Y, Guesmi M, Rollot F, Dehoux M, Guillevin L, Moachon L. Drug-induced hypersensitivity syndrome: clinical and biologic disease patterns in 24 patients. Medicine (Baltimore). 2009. 88:131–140.

6. Chen YC, Chiu HC, Chu CY. Drug reaction with eosinophilia and systemic symptoms: a retrospective study of 60 cases. Arch Dermatol. 2010. 146:1373–1379.

7. Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996. 15:250–257.

8. Walsh SA, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): a clinical update and review of current thinking. Clin Exp Dermatol. 2011. 36:6–11.

9. Tas S, Simonart T. Management of drug rash with eosinophilia and systemic symptoms (DRESS syndrome): an update. Dermatology. 2003. 206:353–356.
10. Wolf R, Matz H, Marcos B, Orion E. Drug rash with eosinophilia and systemic symptoms vs toxic epidermal necrolysis: the dilemma of classification. Clin Dermatol. 2005. 23:311–314.
11. Descamps V, Valance A, Edlinger C, Fillet AM, Grossin M, Lebrun-Vignes B, Belaich S, Crickx B. Association of human herpesvirus 6 infection with drug reaction with eosinophilia and systemic symptoms. Arch Dermatol. 2001. 137:301–304.
12. Sullivan JR, Shear NH. The drug hypersensitivity syndrome: what is the pathogenesis? Arch Dermatol. 2001. 137:357–364.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download