Introduction
Dermabacter hominis (D. hominis) has been identified as an asporogenous, non-motile, rod-shaped microorganism [1]. This agent is usually recognized as an opportunistic human pathogen. Cases of serious infections caused by this agent are extremely rare in Korea [2, 3]. We encountered a case of infection caused by D. hominis in a 56-year-old man who developed bacteremia and he finally expired from septic shock.
Case Report
A 56-year-old man was admitted to our emergency department with cardiac arrest. At the time, he was in an asystolic state. Spontaneous circulation was returned after ten minutes of cardiopulmonary resuscitation (CPR) and the patient showed significant neurologic sequelae. A cerebral computed tomography (CT) scan and a magnetic resonance imaging (MRI) diffusion image showed hydrocephalus. Electroencephalography demonstrated severe hypoxic brain damage. Laboratory tests were performed and the results were hemoglobin: 14.6 g/dL, WBC: 12,900/mm3, platelets: 131,000/mm3 , sodium: 140 mmol/L, potassium: 3.9 mmol/L, chloride: 100 mmol/L, prothrombin time (PT): 13 seconds and the activated partial thromboplastin time (aPTT): 33.5 seconds. He had no specific personal history of chronic disease or immune suppression. After two days, his vital signs were stable, but spontaneous breathing without a mechanical ventilator was impossible. His mental status was comatose and he experienced intermittent seizures. In the following days, he suffered several febrile episodes. Two sets of blood cultures (each set consisted of one aerobic culture bottle and one anaerobic culture bottle) and sputum culture were taken. D. hominis was isolated from two aerobic culture bottles and one anaerobic culture bottle. Haemophilus infuluenzae was isolated from the tracheal aspirates. The urine culture and central venous catheter culture were negative. A chest X-ray revealed pulmonary congestion of both lung fields. Because pneumonia was suspected, the first empirical antibiotic treatment was started using ciprofloxacin for two days. And then, the antimicrobial therapy was then changed to intravenous vancomycin after D. hominis was isolated. While in the hospital, the patient suffered hypoxic brain damage, decreased blood pressure and continued febrile peaks of higher than 38℃. Unfortunately, the patient's condition progressively worsened and he expired from septic shock.
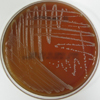
Blood was cultured from this patient, and it yielded bacteria that grew on 5% sheep blood agar plates (HanilKomed, Gyeonggi-do, Korea) as 0.5- to 1 mm diameter colonies after 24 hours in a room air. The colonies were grayish-white, convex and slightly viscid with a sweet, pungent odor (Fig. 1). The isolate was non-spore forming, small gram-positive bacilli with a corynefrom appearance. Biochemical analysis showed that the colonies were positive for catalase and esculin hydrolyses and negative for urease, oxidase and nitrate reductions. Glucose, sucrose, maltose, lactose and xylose were fermented by this isolate, but mannitol was not fermented. The bacterium was identified using the API Coryne system (AB bioMérieux, Hazelwood, MO, USA) as D. hominis (code 4770765). Antibiotic susceptibility testing was initially performed using Sensi-discs (BD, Franklin Lakes, NJ, USA) on Mueller-Hinton blood agar plates. The isolated D. hominis was resistant to clindamycin, erythromycin, levofloxacin, penicillin, oxacillin and trimethoprim/sulfamethoxazole. The isolate was susceptible to vancomycin and teicoplanin. The MICs (Minimal Inhibitory Concentrations) for several antibiotics were determined with E-test strips (AB Biodisc, Solna, Sweden) on Mueller-Hinton blood agar plates and the results were penicillin G: 12 µg/mL, cefotaxime: 8 µg/mL and vancomycin: 0.25 µg/mL.
DNA was purified from the bacterial colonies using the DNeasy Tissue Kit (Qiagen, Hilden, Germany). The 16S rRNA gene was amplified by PCR (ABI 9700, Applied Biosystems, CA, USA); the reactions were heated to 95℃ for five min, followed by 30 cycles of 95℃ for 20 s, 52℃ for 20 s and 72℃ for 30 s. A final extension was carried out at 72℃ for two minutes. The amplicon (approximately 1,500 bp) was run on agarose gel, and the bands were confirmed by ultraviolet (UV) transillumination. Analysis of the nucleotide sequence was performed using an ABI PRISM 3130 Sequencer (Applied Biosystems). The resulting 1,468-bp sequence was compared to the available sequences in the GenBank databases using the BLAST program [4]. More than 99% similarity was found with the D. hominis published sequences.
Discussion
D. hominis is a gram-positive, asporogenous, non-motile, rod-shaped bacterium that produces small grayish-white colonies with an intense, pungent odor [1, 5, 6]. D. hominis bacteria have previously been defined as coryneform groups 3 and 5 in the Special Bacteriology Reference Laboratory collection of the Centers for Disease Control and Prevention (CDC). Groups 3 and 5 are identical except for their ability (group 3) or inability (group 5) to ferment xylose [1].
The bacteria were assigned to the genus and species D. hominis based on the chemotaxonomic, 16S rDNA sequence analyses and DNA-DNA hybridization studies [1, 7]. Chemotaxonomically, D. hominis has a cell wall based on meso-diaminopimelic acid and branched cellular fatty acids. These structures are also found in species of the genus Brevibacterium. However, Brevibacterium spp. are nonfermentative and are phylogenentically quite distant from D. hominis [8].
D. hominis belongs to a new genus and it has recently been recognized as an opportunistic human pathogen. It has primarily been isolated from blood and less commonly from abscesses, wounds, skin lesions, eyes and other body sites. Very few case reports of documented infections caused by D. hominis have been described [2, 3, 9-11]. D. hominis has been shown to cause various conditions including cerebral abscess [2], bacteremia [3], peritoneal dialysis-associated peritonitis [10], chronic osteomyelitis [11], and chronic cutaneous abscesses [9]. In most cases, the patients had severe underlying conditions that caused the patients to be immunocompromised. Only one case of recurrent abscesses caused by D. hominis in an immunocompetent patient has been published [9]. It is known that brain injury and ischemia are related to the various immune mediators. Brain mediated immunosuppression increases the risk of infectious complications [12]. In this context, the severe hypoxic brain damage in this patient might have caused immunosuppression. The virulence of D. hominis is augmented in individuals with compromised defensive capacities or those individuals who are undergoing administration of broad spectrum antimicrobial treatment [3]. In the current study, fever episodes occurred prior to the antibiotic treatment. These findings illustrated that the pathogenesis of the severe infection in this patient was the compromised immune function rather than the broad spectrum antimicrobial treatment.
D. hominis is a rare, opportunistic pathogen and its clinical role has not yet been fully elucidated. The septicemia of D. hominis and the clinical course of the patient described in this report illustrate that D. hominis may well have the potential to cause severe systemic infection, and especially in patients with defective immune function and severe underlying diseases.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download