Abstract
Background
The contribution of the private sector to the treatment of tuberculosis (TB) is getting larger, and the private sector pays more attention to individualized, intensive care than patient monitoring or education, which would improve the microbiological cure rate or at least completion of treatment. We aim in this paper to assess the impact of the improved monitoring of patient on the treatment outcome in the private tertiary healthcare center.
Materials and Methods
We compared the data of the positive sputum cultures for TB from March 1, 2003 to March 31, 2006 (37 months) with that data from July 1, 2007 to August 31, 2008 (14 months) in single private tertiary healthcare center in the Republic of Korea (ROK). In the latter period, we notified physicians of the new culture-confirmed cases via a cellular phone short-massage-service (SMS) to prevent delayed recognition of positive cultures and we gave calls to patients to encourage treatment adherence and to complete the whole schedule of medication.
The burden of tuberculosis in the Republic of Korea (ROK) has decreased considerably owing to the government's administrative priority for the prevention and treatment of the TB since the 1960's. The ROK no longer belongs to the group of countries with the high TB burden, rather, it is now a country with an intermediate burden of TB. A positive sputum acid fast bacilli (AFB) smear and culture positivity in the ROK have dramatically dropped from 0.94% in 1965 to 0.22% in 1995 with about a 5.1% decrease every year [1]. While the proportion of patients who receive advanced individualized treatment in private sector has currently increased up to 77.2% [2], TB cases are is still persistent in the ROK. The estimated incidence of TB in the ROK was 65.4 cases per 100,000 in 2004 and 97.0 cases per 100,000 in 2009 [3]. Among the countries in the Organization for Economic Cooperation and Development (OECD), the estimated incidence of TB and deaths from TB in the ROK are still about 29 times and 33 times higher than those of the lowest country like Iceland respectively [4].
Traditionally in the ROK, both public and private sector medical facilities have coexisted for decades. The contribution of private sector to the TB control has become more important as the number of private tertiary healthcare center has increased, and as more and more patients prefer private hospitals to public health care centers. The private tertiary healthcare center, unlike public health centers, usually pay more attention to making a precise diagnosis, intensive care and individualized treatment than to education and monitoring of patients to achieve microbiological cure or completion of treatment.
We organized a committee named "SCET" (Soon Chun Hyang Control and Elimination of Tuberculosis) along with this study for sustained future action against TB in our hospital. The committee includes infectious diseases specialists, pulmonologists, clinical microbiologists, family medicine physicians, computer programmers, laboratory technicians, specialized nurses for TB patient care and infection control practitioners. The goal of this study is to assess the impact of our strategies for the patients with positive AFB cultures on the TB treatment outcome in a private tertiary healthcare center.
We compared positive culture results for TB between 2 different periods in a single private tertiary healthcare center in the ROK using a computerized Order Communication System (OCS). The period before SCET was from March 1, 2003 to March 31, 2006 (37 months). The period after SCET was from July 1, 2007 to August 31, 2008 (14 months). WHO case definition was applied according to a previous history of anti-TB treatment as follows: 'New' is a patient who never had treatment for TB or who took anti-TB drugs for less than 1 month. 'Relapse' is a bacteriologically (smear or culture) positive, newly diagnosed patient who has a previous treatment history, which resulted in a cure, or the patient had just completed TB treatment, 'Treatment after failure' is a patient who started on a re-treatment regimen after having failed previous treatment. 'Treatment after default' is a bacteriologically positive patient who returns to treatment, followed by interruption of treatment for 2 months or more. 'Transfer in' is a patient who has been transferred from another TB register to continue treatment. 'Others' are all cases that do not fit the above definitions. This group includes the chronic cases and patients who are sputum-positive at the end of a re-treatment regimen.
Interventions of the SCET for AFB positive cases consisted of activities listed below. The SCET committee mainly focused on encouraging new culture-confirmed patients to visit a hospital. In private hospital, unlike in public health centers, the patient's visit to the clinic is depending on the patient's own decision to make an appointment with his or her doctor.
1) Notification of the positive results for TB (the new culture-confirmed cases of TB) via a cellular phone short-message service (SMS) to the physicians who had ordered the AFB culture. The messages were automatically sent by a computerized program as soon as a clinical microbiologist confirmed the culture results.
2) Monitoring of new culture-confirmed TB patients who did not start anti-TB treatment after 2 months of SMS notifications. These patients were informed of the positive result for TB by telephone and they made a new appointment with physicians after communication with the SCET members.
3) Monitoring of the patients' visits to the clinic at the programmed schedule and their compliance with taking the anti-TB drugs.
We compared the characteristics of the subject population in the 2 different periods. We surveyed the demographic characteristics, the diseased organ of TB infection (whether pulmonary or extra pulmonary) and any history of previous TB treatment. The institutional ethics committee approved this retrospective study and the need for informed consent from the patients was waived.
During the two periods, we used Ogawa media for sputum AFB culture. Specimens were inoculated on Ogawa medium after proper decontamination and concentration by sodium hydroxide method. The inoculated media was incubated at 35℃ for 8 weeks. Colonies were identified by AFB staining and conventional biochemistry tests. When a positive culture was detected, we reported the positive results and the duration (days) of incubation for the sputum culture.
The primary outcome was to improve the completion rate of treatment for the patients with a positive TB culture. The secondary outcome was to improve the patients' ultimate cure. We defined the treatment outcomes to clarify the results of the SCET interventions based upon the definition of 'cure' and 'completion' as proposed by the WHO.
1) Completion of anti-TB treatment
Those patients who maintained the treatment for at least 6 months without interruption, irrespective of the clinical or microbiological cure.
>2) Initiation of anti-TB medication
Those patients who started anti-TB treatment within a month since the date of culture results report.
3) Failure of anti-TB treatment
Those patients who failed to initiate treatment within a month since the reported date for the culture results, or who had initiated the treatment, but it was interrupted within a month.
Antimicrobial susceptibility test was recommended for the patients at the initial assessments. But as the test is performed after an additional request and charge, this testing was not done in many cases.
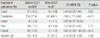
Our study included a total of 604 patients with positive AFB culture results. Four hundred forty one patients were enrolled before the SCET intervention period, from March 1, 2003 to March 31, 2006 (37 months) and 163 patients were enrolled after SCET intervention, from July 1, 2007 to August 31, 2008 (14 months). Before the intervention, 282 (63.9%) were males, while 93 (57.0%) were males after the intervention (Table 1).
According to the previous anti-TB treatment history, new patients were still dominant though they were slightly decreased from 316 (86.3%) to 74 (81.3%) after intervention period. The number of non-tuberculous mycobacteria (NTM) isolates among the positive AFB culture cases was markedly increased after intervention from 75 (17.0%) to 72 (44.2%) (Table 1).
Antimicrobial susceptibility test was done for 49.2% of the patients before SCET, and for 73.6% of the patients after SCET. The drug-resistances among the TB cases were not significantly different before and after SCET intervention (37 [20.3%] patients before SCET versus 13 [19.4%] patients after SCET). However, the prominent impact of the SCET activities was shown in the portion of patients without drug susceptibility test SCET which was considerably decreased from 50.8% to 26.4% (Table 2).
After SCET intervention, initiation of anti-TB medication for Mycobacterium tuberculosis significantly increased from 86.3% to 94.5% (P<0.05); the interval to medication from the first AFB culture results was shortened from 22.9 days to 5.6 days, without a significant difference (P=0.19). Interruption of anti-TB medication within 1 month and within 6 months was not significantly changed (5.5% to 4.7% and 13.0% to 11.6%) (Table 3). The completion rate of anti-TB treatment increased from 57.4% to 68.1% (P<0.01). A significant decrease of the number of default patients was also noticeable (P<0.01) (Table 4). The proportion of cured patients was 8.5% before SCET intervention and 9.9% after SCET intervention, without statistical significance (P=0.67). But the success rate (sum of the cure rate and completion rate) was significantly increased (OR: 0.54, CI: 0.32-0.93, P=0.03).
Physicians usually get information about the AFB smear results early, so that smear positive TB patients are seldom neglected for TB treatment. However, smear negative TB patients are often neglected owing to the long incubation period for the culture results in solid media. Joh et al. showed that it took physicians an average of 37 days to receive positive-culture results and the median interval between the initiation of anti-TB treatment and positive AFB cultures was 20 days [5]. These intervals were similar to our result before the SCET interventions (22.9 days). Because of the delay, patients as well as his or her physicians often forgot that they had ever performed AFB culture. Paradoxically, private tertiary health care or specialized tertiary care centers are much more vulnerable to such neglect, while health the public healthcare centers have an effective mass-treatment pathway for TB control.
The primary goal of SCET activities was to reduce the neglected positive AFB culture results by means of notification strategies. The impact of the SCET was proven by the significant increase (86.5% to 94.5%) of the initiation rate for TB treatment without an increase of the interruption rate of anti-TB treatment. The time from the first AFB culture results to the initiation of medication was markedly shortened from 22.9 days to 5.6 days after SCET intervention (P=0.19).
The next goal of the intervention was to ultimately improve the treatment outcomes. The rate of completing treatment increased from 57.4% to 68.1% (P<0.01). The SCET activities contributed to remarkable progress of controlling TB at our hospital. The lack of a significant increase of the cure rate in our study was due to the fact that a negative culture was not microbiologically demonstrable once the patient's sputum production decreased.
According to the latest Nationwide Tuberculosis Prevalence Survey of Korea in 1995, 53% of TB patients were reported to have received treatment in public healthcare centers and 47% received treatment in the private sector [2]. However, the majority of patients (77.2%) are treated in the private sector nowadays [3]. As for the results of treatment, only 57% of the patients were cured after anti-TB treatment in the private sector [6]. Therefore, treatment of TB under administrative supervision should be reemphasized in the following manner: 1) direct observation of therapy (DOT), 2) monitoring the adherence to drug treatments, 3) counseling to encourage completion of the treatment schedule, and finally to achieve cure and to prevent the emergence of drug resistance.
TB is still a considerable threat to global health due to the emergence of multi-drug resistant-tuberculosis (MDR-TB) outbreaks among young adults and the elderly of developing countries in Africa and Asia. Percentages of MDR strains were 3.9% among new cases and 27.2% among the previously treated cases in the private sector [7] while 2.7% among the new cases and 14.0% among the previously treated cases in the public health centers in ROK [8]. Therefore, better treatment adherence in TB patients would theoretically reduce the emergence of MDR-TB. In our study, drug-resistant TB for one or more drugs paradoxically increased during the study periods. Considering the fact that treatment naïve new patients were decreased and the susceptibility testing had increased after SCET, this apparent increased resistance has to be explained by a selection bias from the increased susceptibility test for the at-risk population, which was encouraged by the SCET activity, rather than being a true increase of MDR-TB in the community.
The number of NTM isolates was markedly increased from 17.0% to 44.2% after SCET intervention. As we used the same solid media culture techniques during both periods, this increase of the NTM is not the result of increased laboratory sensitivity, but it has to do with the relative increase of NTM organisms. Similar results have been reported in different university hospitals in the ROK [9, 10]. Our results did not differentiate clinical NTM lung diseases from simple colonization. Usually 40-50% of the patients with NTM isolates were determined to have definite NTM lung disease in the Unites States of America, Canada and Western Europe [11]. Koh et al. reported that 17% of the patients with NTM isolates were determined to have definite NTM lung disease in the ROK [12]. The evaluation process of NTM lung disease requires a clinician's experience and timely diagnostic decisions [13].
In the ROK, owing to the historical background of the government's dominant role in the mass treatment of infectious diseases, public health care providers still have administrative authority over the private sector [14]. However, due to people's preference for private clinics or university hospitals, the provider's role for TB control in the private sector had increased. Positive collaboration between the government's TB surveillance and monitoring programs and the private sector's specialized and individualized care might synergistically improve the national TB control ("Public-Private Mix" or "Public-Private Partnership")[15]. Health care providers in the private sector should focus more on reducing diagnostic delays, performing susceptibility testing and proper notification for all the diagnosed cases for completion of the 6-to-9-month course of treatment. Our results showed the possibility to reduce treatment delay for the TB patients in the private tertiary healthcare center setting. These effective strategies can improve the success rate of anti-TB treatment and possibly contribute to eradicating TB in the ROK.
Figures and Tables
Acknowledgements
The authors express our gratitude to all the SCET members who participated in the monitoring activities.
References
1. Ministry of Health and Welfare. Korean National Tuberculosis Association. Report on the 7th tuberculosis prevalence survey in Korea. 1995.
2. Korean Center for Disease Control and Prevention. 2007 Annual report on the notified tuberculosis patients in Korea. 2008. Seoul: KCDC.
3. Korea Centers for Disease Control and Prevention. 2009 Annual report on the notified tuberculosis patients in Korea. 2010.
4. Global Tuberculosis Control, 2010. World Health Organisation. Accessed 2 February 2011. Available at: http://www.who.int/tb/country/en/.
5. Joh JS, Lee CH, Lee JE, Park YK, Bai GH, Kim EC, Han SK, Shim YS, Yim JJ. The Interval between initiation of anti-tuberculosis treatment in patients with culture-positive pulmonary tuberculosis and receipt of drug-susceptibility test results. J Korean Med Sci. 2007. 22:26–29.

6. Kim HJ, Hong YP, Kim SJ, Lew WJ, Lee EG. Ambulatory treatment of multidrug-resistant pulmonary tuberculosis patients at a chest clinic. Int J Tuberc Lung Dis. 2001. 5:1129–1136.
7. Choi JC, Lim SY, Suh GY, Chung MP, Kim H, Kwon OJ, Lee NY, Park YK, Bai GH, Koh WJ. Drug resistance rates of Mycobacterium tuberculosis at a private referral center in Korea. J Korean Med Sci. 2007. 22:677–681.

8. Bai GH, Park YK, Choi YW, Bai JI, Kim HJ, Chang CL, Lee JK, Kim SJ. Trend of anti-tuberculosis drug resistance in Korea, 1994-2004. Int J Tuberc Lung Dis. 2007. 11:571–576.
9. Koh WJ, Kwon OJ, Yu CM, Jeon KM, Suh GY, Chung MP, Kim HJ, Han SW, Park SY, Lee NY. Recovery rate of Nontuberculous Mycobacteria from acid-fast-bacilli smear-positive sputum specimens. Tuberc Respir Dis. 2003. 54:22–32.

10. Lee JY, Choi HJ, Lee H, Joung EY, Huh JW, Oh YM, Lee SD, Kim WS, Kim DS, Kim WD, Shim TS. Recovery rate and characteristics of Nontuberculous Mycobacterial isolates in a university hospital in Korea. Tuberc Respir Dis. 2005. 58:385–391.

11. Marras TK, Daley CL. Epidemiology of human pulmonary infection with nontuberculous mycobacteria. Clin Chest Med. 2002. 23:553–567.
12. Koh WJ, Kwon OJ, Jeon K, Kim TS, Lee KS, Park YK, Bai GH. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest. 2006. 129:341–348.

13. Koh WJ, Kwon OJ, Lee KS. Diagnosis and treatment of nontuberculous mycobacterial pulmonary diseases: A Korean perspective. J Korean Med Sci. 2005. 20:913–925.

14. Seung KJ, Bai GH, Kim SJ, Lew WJ, Park SK, Kim JY. The treatment of tuberculosis in South Korea. Int J Tuberc Lung Dis. 2003. 7:912–919.
15. Ambe G, Lönnroth K, Dholakia Y, Copreaux J, Zignol M, Borremans N, Uplekar M. Every provider counts: effect of a comprehensive public-private mix approach for TB control in a large metropolitan area in India. Int J Tuberc Lung Dis. 2005. 9:562–568.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download