Abstract
Background
The purpose of this study was to determine the spectrum of locally prevalent pathogens and their susceptibility patterns responsible for bacteremia in pediatric hemato-oncologic patients for empiric antimicrobial therapy.
Materials and Methods
A one-year retrospective study of pediatric hematooncologic patients with bacteremia in Seoul St. Mary's Hospital, the Catholic University of Korea, from April 2009 to March 2010 was conducted using previous medical records. The findings were compared with our previous data obtained from 2004 to 2006.
Results
Sixty-five episodes of bacteremia were recorded in 41 patients. Of them, 55 (84.6%) occurred in neutropenic and 10 (15.4%) in non-neutropenic patients. Gram-positive organisms were more commonly isolated than Gram-negative organisms (56.9% vs. 41.5%) in the following order: viridans streptococci (23.1%), Klebsiella pneumoniae (21.6%), coagulase-negative staphylococci (12.3%), Staphylococcus aureus (7.7%), Enterococcus faecium (7.7%). Susceptibility rates of viridans streptococci to penicillin, cefotaxime and vancomycin were 33.3%, 60% and 100%, and those of Enterobacteriaceae to amikacin, ceftazidime, piperacillin/ tazobactam and meropenem were 94.7%, 73.7%, 78.9%, and 100%, respectively. Compared to our previous data, infection still contributed towards a major fraction of mortality and morbidity in the management of patients with cancer. No differences in mortality rate were observed between isolated organisms from bacteremia.
Figures and Tables
Figure 1
Percentage of Gram-positive, Gram-negative bacteria and fungus isolated from blood stream infections during years of 2004-2006 versus years of 2009-2010
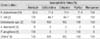
Table 2
Causative Organisms in 65 Episodes of Bacteremia Developed in Pediatric Hemato-Oncologic Patients with or without Neutropenia

Table 3
Causative Organisms in 65 Episodes of Bacteremia Developed in Pediatric Hemato-Oncologic Patients with or without Catheter

References
1. Kaddan-Lottick NS. Kliegman RM, Behman RE, Jenson HB, Stanton BF, editors. Epidemiology of childhood and adolescent cancer. Nelson textbook of pediatrics. 2007. 18th ed. Philadelphia: WB Saunders Co.;2097–2099.
2. Viscoli C, Varnier O, Machetti M. Infections in patients with febrile neutropenia: epidemiology, microbiology, and risk stratification. Clin Infect Dis. 2005. 40:Suppl 4. S240–S245.

3. Pizzo PA. Management of fever in patients with cancer and treatment-induced neutropenia. N Engl J Med. 1993. 328:1323–1332.

4. Lee HJ, Lee JW, Kim JH, Lee KH, Chung NG, Lee DG, Lee MJ, Choi SH, Kang JH, Lee SJ, Jeong DC, Cho B, Kim HK. A survey for causative organisms and antimicrobial susceptibilities of bacteremia in a single center children with hemato-oncologic diseases (2004~2006). Clin Pediatr Hematol Oncol. 2008. 15:65–74.
5. Bodey GP, Buckley M, Sathe YS, Freireich EJ. Quantitative relationships between circulating leukocytes and infection in patients with acute leukemia. Ann Intern Med. 1966. 64:328–340.

6. Mermel LA, Farr BM, Sherertz RJ, Raad II, O'Grady N, Harris JS, Craven DE. Infectious Diseases Society of America. American College of Critical Care Medicine. Society for Healthcare Epidemiology of America. Guidelines for the management of intravascular catheter-related infections. Clin Infect Dis. 2001. 32:1249–1272.

7. Schimpff SC. Empiric antibiotic therapy for granulocytopenic cancer patients. Am J Med. 1986. 80:13–20.
8. Yun BY, Lee LH. Septicemia in children with neoplastic disease. J Korean Pediatr Soc. 1992. 35:1481–1492.
9. Marron A, Carratalà J, Alcaide F, Fernández-Sevilla A, Gudiol F. High rates of resistance to cephalosporins among viridans-group streptococci causing bacteraemia in neutropenic cancer patients. J Antimicrob Chemother. 2001. 47:87–91.

10. Lee DG, Choi SM, Choi JH, Yoo JH, Park YH, Kim YJ, Lee S, Min CK, Kim HJ, Kim DW, Lee JW, Min WS, Shin WS, Kim CC. Selective bowel decontamination for the prevention of infection in acute myelogenous leukemia: a prospective randomized trial. Korean J Intern Med. 2002. 17:38–44.

11. Choi EH, Pyo JW, Park JY, Kwon KB, Yun BY, Shin HY, Lee HJ, Ahn HS. Infections in children with neoplastic disease. J Korean Pediatr Soc. 1995. 38:366–377.
12. Kim YH, Lee HD, Hah JO. Bacteremia in pediatric cancer patients: causative organisms and antibiotic sensitivities. Korean J Pediatr. 2005. 48:619–623.
13. Park HW, Youn HS, Im HJ, Kim MN, Seo JJ, Moon HN. Risk factors of bloodstream infection associated mortality in pediatric patients with hemato-oncologic disease. Korean J Hematol. 2007. 42:343–352.

14. Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T, Feld R, Pizzo PA, Rolston KV, Shenep JL, Young LS. 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis. 2002. 34:730–751.

15. Celkan T, Ozkan A, Apak H, Diren S, Can G, Yuksel L, Yildiz I. Bacteremia in childhood cancer. J Trop Pediatr. 2002. 48:373–377.

16. Shenep JL. Viridans-group streptococcal infections in immunocompromised hosts. Int J Antimicrob Agents. 2000. 14:129–135.

17. Tunkel AR, Sepkowitz KA. Infections caused by viridans streptococci in patients with neutropenia. Clin Infect Dis. 2002. 34:1524–1529.

18. Weisman SJ, Scoopo FJ, Johnson GM, Altman AJ. Quinn JJ. Septicemia in pediatric oncology patients: the significance of viridans streptococcal infections. J Clin Oncol. 1990. 8:453–459.

19. Uh Y, Hwang GY, Jang IH, Yoon KJ, Kim HY. Antimicrobial susceptibilities of viridans streptococci isolated recently. J Lab Med Qual Assur. 2002. 24:225–230.
20. Cho EH, Lee NY. Clinical significance of viridans streptococcal bacteremia. Korean J Lab Med. 2003. 23:246–250.
21. Kim SH, Lee YA, Eun BW, Kim NH, Lee JA, Kang HJ, Choi EH, Shin HY, Lee HJ, Ahn HS. Etiological agents isolated from blood in children with hemato-oncologic diseases (2002-2005). Korean J Pediatr. 2007. 50:56–64.

22. Park SM, Choe BK, Kim CS, Kim JS, Kim HS, Ryoo NH. Bacteremia in pediatric cancer patients: a single center study. Korean J Pediatr. 2006. 49:882–888.

23. Paterson DL, Ko WC, Von Gottberg A, Casellas JM, Mulazimoglu L, Klugman KP, Bonomo RA, Rice LB, McCormack JG, Yu VL. Outcome of cephalosporin treatment for serious infections due to apparently susceptible organisms producing extended-spectrum beta-lactamases: implications for the clinical microbiology laboratory. J Clin Microbiol. 2001. 39:2206–2212.

24. Carmeli Y, Akova M, Cornaglia G, Daikos GL, Garau J, Harbarth S, Rossolini GM, Souli M, Giamarellou H. Controlling the spread of carbapenemase-producing gram-negatives: therapeutic approach and infection control. Clin Microbiol Infect. 2010. 16:102–111.

25. Caselli D, Cesaro S, Ziino O, Zanazzo G, Manicone R, Livadiotti S, Cellini M, Frenos S, Milano GM, Cappelli B, Licciardello M, Beretta C, Aricò M, Castagnola E. Infection Study Group of the Associazione Italiana Ematologia Oncologia Pediatrica (AIEOP). Multidrug resistant Pseudomonas aeruginosa infection in children undergoing chemotherapy and hematopoietic stem cell transplantation. Haematologica. 2010. 95:1612–1615.

26. Oliveira AL, de Souza M, Carvalho-Dias VM, Ruiz MA, Silla L, Tanaka PY, Simões BP, Trabasso P, Seber A, Lotfi CJ, Zanichelli MA, Araujo VR, Godoy C, Maiolino A, Urakawa P, Cunha CA, de Souza CA, Pasquini R, Nucci M. Epidemiology of bacteremia and factors associated with multi-drug-resistant gram-negative bacteremia in hematopoietic stem cell transplant recipients. Bone Marrow Transplant. 2007. 39:775–781.

27. Song JH. Current status and future strategies of antimicrobial resistance in Korea. Korean J Med. 2009. 77:143–151.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download