Abstract
Background
Influenza transmission in households a subject of renewed interest especially in pandemic situation. We performed this study to investigate the laboratory-confirmatory rate in household contacts with index cases of pandemic influenza (H1N1 2009).
Materials and Methods
For three months from 1 September and 29 November 2009, people who had a history of close contact with confirmed cases of pandemic influenza (index case) were recruited. The information on the study participants was collected using a standardized questionnaire. Presence of the pandemic influenza (H1N1 2009) infection was confirmed by real-time reverse-transcription polymerase chain reaction (RT-PCR).
Results
A total of 113 index cases and 141 household contacts were investigated. One hundred and four index cases (92.0%) were younger than 20 years. The median age of household contacts was 40 years. Twenty eight household contacts (19.8%) had acute respiratory illness (ARI). Overall, 10.6% of enrolled household contacts were positive in RT-PCR for pandemic influenza (H1N1 2009). The positive rate of household contacts with ARI was 25.0% and it was 7.1% in household contacts without ARI. The positive rate was significantly higher in children and young adults under 30 years (28.3%) compared with that in household contacts older than 30 years (8.3%).
Influenza virus can spread rapidly between people in close settings, through inhalation or contact with infected droplets, to those around them such as members of households, classmates at school, co-workers at work, and comrade in a military (1). Information on the dynamics of viral transmission is required to effectively control the viral spread. Traditionally, seasonal influenza transmission dynamics has been best characterized based on the household data (2). Pandemic influenza (H1N1 2009) is also known to spread rapidly within members of households (3) and several epidemiologic studies described the transmissibility of the pandemic influenza (H1N1 2009) in household settings (3-6). However, most of the studies used influenza-like illness (ILI) as a parameter of influenza even though many ILI cases were not confirmed as influenza by laboratory test (7).
The present study was conducted to investigate the laboratory-confirmatory rate of the household contacts with index case of pandemic influenza (H1N1 2009).
Close contact was defined as exposure to an index case at a distance of <1 meter over 1 hour beginning 7 days before or after symptom onset of the index case (5, 8). An acute respiratory illness (ARI) was defined by the presence of at least two of the symptoms of fever or feverishness, cough, sore throat, and rhinorrhea (4). We defined index case as the first person in a household who had influenza-like illness and was positive for pandemic influenza (H1N1 2009) virus by real-time reverse-transcriptase polymerase chain reaction (RT-PCR).
This study was performed in Armed Forces Seoul Hospital (Seoul, Republic of Korea), that provides primary health care services to live-out military personnel and their family members residing in Seoul. Between 1 September and 29 November 2009, people who had a history of close contact with index case were recruited in this study. The index cases were identified at either our hospital or other hospitals. When the an index case were identified at other hospitals, we got their medical records to confirm whether they satisfied the definitions of index case. All index cases took oseltamivir immediately after the positive confirmatory test. The information of household contacts was collected using a standardized questionnaire regarding demographic characteristics, underlying diseases and influenza symptoms. We collected throat swabs from the household contacts, which were tested to confirm the diagnosis of pandemic influenza (H1N1 2009) infection by real-time RT-PCR. After initial visit to hospital, all the household contacts were instructed to be confined at home while their clinical signs and symptoms were monitored for 7 days. If the household contacts had a new ARI during this period, they visited our hospital again and a throat swab was repeated. This epidemiologic study was approved by the Institutional Review Boards of The Armed Forces Medical Command (Seongnam-si, Gyeonggi-do, Republic of Korea). Informed consent was obtained from all study participants.
A total of 113 index cases from 111 households were identified in this study. Data on 141 household contacts were available. One hundred four (92.0%) of the index cases were younger than 20 years and their median age was 11.7 years. All patients took oseltamivir within 72 hours after symptoms onset. There was no hospitalization or death associated with pandemic influenza (H1N1 2009) infection among the participants in this study.
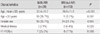
Table 1 shows the characteristics of enrolled household contacts. Their median age was 40 years, ranged 2-72 years. Most of them (79.4%) were middle aged (20-49 years) adults. Sixteen household contacts (11.3%) were younger than 20 years. Thirty four household contacts (24.1%) were female. Seven (5.0%) had chronic medical illnes such as hypertension (n=5), chronic hepatitis (n=2), previous myocardial infarction (n=1), hypercholesterolemia (n=1). One hundred seven household contacts (75.9%) were parents of the index cases and 19 (13.5%) were siblings. Forty household contacts (28.4%) had one or more influenza-like symptoms. Most common presenting symptoms were cough (9.9%), throat pain (9.2%) and rhinorrhea (8.5%). Twenty eight household contacts (19.8%) manifested the defined symptoms of ARI. Of 141 household contacts, 15 (10.6%) were positive by the real-time RT-PCR for pandemic influenza (H1N1 2009).
When household contacts were compared according to whether they had ARI or not, household contacts with ARI were younger than those without ARI (Table 2). Sexual difference was not observed between two groups. Laboratory-confirmatory rate was 25.0% in household contacts with ARI and 7.1% in those without ARI (P=0.006).
Fig. 1 shows the positive rates of 2009 H1N1 virus in RT-PCR according to age groups. The rate of positive results in RT-PCR was significantly higher in young household contacts under 30 years compared with that in household contacts older than 30 years (28.3 vs 8.3%, P=0.03). There was no positive case in people over 50 years.
When RT-PCR positivity of household contact was analyzed according to index case ages (<20 years vs ≥20 years), there was no significant differences (10.8% vs. 9.1%, P>0.05).
Two cases developed new ARI during the follow-up; and repeated swab revealed that the test result was turned to positive in one of them. All confirmed household contacts were treated with oseltamivir. No pandemic vaccine was used in any study participants before and during the study period.
This study described the real-time RT-PCR positive rate for pandemic influenza (H1N1 2009) in household contacts in Korean households. Overall, 10.6% of enrolled household contacts were positive in the real time RT-PCR. Laboratory-confirmatory rate of pandemic influenza (H1N1 2009) was 25.0% in household contacts with ARI, while it was 7.1% in household contacts without ARI. Asymptomatic infected persons play an possible role as virus carriers since they might potentially spread virus to others (9). Investigators previously detected influenza viruses in respiratory specimens from healthy children without symptom (10, 11). In case of seasonal influenza, asymptomatic infection accounts for about one thirds of all influenza cases (12). In our results, infection rate of pandemic influenza (H1N1 2009) in asymptomatic household contacts was relatively low when compared with seasonal influenza. We thought that these findings did not mean lower infectivity of pandemic influenza (H1N1 2009). This finding might be explained as follows. First, we did not estimate the number of cases with ILI but laboratory-confirmed cases. Secondly, the use of antiviral agent in the early phase of pandemic influenza might lower infection rate. Sophia et al. reported recently that household contacts of index patients who had taken oseltamivir in seasonal influenza had a statistically insignificant but lower risk of developing laboratory-confirmed infection (13). Asymptomatic household contacts with viral carriage can continue to work or go to school, increasing the chance of exposure of other workers or classmates. Therefore, isolation of asymptomatic or mild symptomatic household contacts who continue their daily activities in the early phase of pandemic is justified to decrease the risk of virus spread. Early and accurate identification through laboratory confirmation such as RT-PCR can be helpful to decide patient isolation.
In this study, household contacts of younger than 30 years had higher positive rate in RT-PCR. Our result is consistent with those of previous reports describing suggesting that children and adolescents are especially vulnerable to pandemic influenza (H1N1 2009) than adults and elderly (4, 14). This can be explained by the suggestion that pandemic influenza (H1N1 2009) has enough antigenic similarity to related H1N1 influenza virus strains of the past and it protects older people exposed to them previously (14).
In seasonal flu, children shed virus for 40-80% longer periods than adults, and household contacts of index patients younger than 20 years had a higher risk of laboratory-confirmed secondary infection (13). In this study, however, laboratory confirmatory rate of household contacts were not different by two age groups of index cases. Because most index patients (92.0%) were younger than 20 years in this study, further study is needed to clarify this point.
This study has at least two potential limitations. First, there was a shortage of information on other family members who did not visit our hospital and we could not assess household secondary attack rate. Second, if infected household contacts had not been shedding virus at the time of specimen collection, they would have tested negative in confirmatory test. Therefore, there would be a possibility of underestimating the number of cases with positive results.
In conclusion, laboratory-confirmatory rate was higher in young household contacts, implying their vulnerability to pandemic influenza (H1N1 2009) infection. In addition, 7.1% in household contacts without ARI were positive in confirmatory test. Considering the important role of asymptomatic virus carriers, this finding suggests that mild symptomatic or asymptomatic household contacts should receive strict infection control measures, especially during early pandemic period.
Figures and Tables
Figure 1
Positive rates in RT-PCR according to age groups of enrolled household contacts. The rate of positive results in RT-PCR is significantly higher in children and young adults, and there is no positive case in people over 50 years. Numbers on the bar represent the ratio of positive cases to total cases. RT-PCR, reverse-transcription polymerase chain reaction.

Table 1
Characteristics of the Household Contacts

MI, myocardial infarction; ARI, acute respiratory illness; RT-PCR, reverse-transcription polymerase chain reaction.
*travel history to risk area within 14 days before study participation.
†3 was repeated throat swabs due to inadequate sampling at the first swab and 2 was due to newly developed ARI during the follow-up.
References
1. Santibañez S, Fiore AE, Merlin TL, Redd S. A primer on strategies for prevention and control of seasonal and pandemic influenza. Am J Public Health. 2009. 99:Suppl 2. S216–S224.

2. Longini IM Jr, Koopman JS, Monto AS, Fox JP. Estimating household and community transmission parameters for influenza. Am J Epidemiol. 1982. 115:736–751.

3. Health Protection Agency. Health Protection Scotland. National Public Health Service for Wales. HPA Northern Ireland Swine influenza investigation teams. Epidemiology of new influenza A (H1N1) virus infection, United Kingdom, April-June 2009. Euro Surveill. 2009. 14:pii: 19232.
4. Cauchemez S, Donnelly CA, Reed C, Ghani AC, Fraser C, Kent CK, Finelli L, Ferguson NM. Household transmission of 2009 pandemic influenza A (H1N1) virus in the United States. N Engl J Med. 2009. 361:2619–2627.

5. Yang Y, Sugimoto JD, Halloran ME, Basta NE, Chao DL, Matrajt L, Potter G, Kenah E, Longini IM Jr. The transmissibility and control of pandemic influenza A (H1N1) virus. Science. 2009. 326:729–733.

6. Odaira F, Takahashi H, Toyokawa T, Tsuchihashi Y, Kodama T, Yahata Y, Sunagawa T, Taniguchi K, Okabe N. Assessment of secondary attack rate and effectiveness of antiviral prophylaxis among household contacts in an influenza A(H1N1) outbreak in Kobe, Japan, May-June 2009. Euro Surveill. 2009. 14:pii: 19320.
7. Kelly H, Carville K, Grant K, Jacoby P, Tran T, Barr I. Estimation of influenza vaccine effectiveness from routine surveillance data. PLoS One. 2009. 4:e5079.

8. Calatayud L, Kurkela S, Neave PE, Brock A, Perkins S, Zuckerman M, Sudhanva M, Bermingham A, Ellis J, Pebody R, Catchpole M, Heathcock R, Maguire H. Pandemic (H1N1) 2009 virus outbreak in a school in London, April-May 2009: an observational study. Epidemiol Infect. 2010. 138:183–191.

9. Foy HM, Cooney MK, Allan ID, Albrecht JK. Influenza B in households: virus shedding without symptoms or antibody response. Am J Epidemiol. 1987. 126:506–515.

10. Winther B, Alper CM, Mandel EM, Doyle WJ, Hendley JO. Temporal relationships between colds, upper respiratory viruses detected by polymerase chain reaction, and otitis media in young children followed through a typical cold season. Pediatrics. 2007. 119:1069–1075.

11. Winther B, Hayden FG, Hendley JO. Picornavirus infections in children diagnosed by RT-PCR during longitudinal surveillance with weekly sampling: Association with symptomatic illness and effect of season. J Med Virol. 2006. 78:644–650.

12. Carrat F, Vergu E, Ferguson NM, Lemaitre M, Cauchemez S, Leach S, Valleron AJ. Time lines of infection and disease in human influenza: a review of volunteer challenge studies. Am J Epidemiol. 2008. 167:775–785.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download