Abstract
Infections due to Candida species are becoming more frequent in several patient population and settings. The proportion of non-albicans Candida spp. causing candidemia has increased during the recent decades. Especially, fungaemia due to Candida glabrata has reduced susceptibility to azoles. We report a case of iliopsoas abscess caused by Candida glabrata. A 51-year-old male diabetic patient was admitted with fever and both hip joint pain. Abdominal CT scan revealed huge left iliopsoas intramuscular abscess and left perinephric abscess. The abscess was drained percutaneously. Cultures of the pus were positive for Candida glabrata. The patient's condition improved after abscess drainage and was discharged with oral antifungal agent.
Figures and Tables
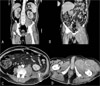
Figure 1
Contrast-enhanced CT scan shows a huge left iliopsoas intramuscular abscess (30 cm) and left perinephric abscess (10.4 cm) (A, B).

References
1. Krcmery V, Barnes AJ. Non-albicans Candida spp. causing fungaemia: pathogenicity and antifungal resistance. Hosp Infect. 2002. 50:243–260.

2. Oh BJ, CHoi HW, Lee JS, Cho D, Kee SJ, Shin MG, Shin JH, Suh SP, Ryang DW. Clinical and laboratory features of candidemia caused by different Candida spercies. Korean J Lab Med. 2005. 25:317–323.
3. Fidel PL Jr, Vazquez JA, Spbel JD. Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to Candida albicans. Clin Microbiol Rev. 1999. 12:80–96.

4. Tan TY, Tan AL, Tee NW, Ng KS. A retrospective analysis of antifungal susceptibilities of Candida blood stream isolates from Singapore hospitals. Ann Acad Med Singapore. 2008. 37:835–840.
5. Crum-Cianflone NF. Bacterial, fungal, parasitic, and viral myositis. Clin Microbiol Rev. 2008. 21:473–494.

6. Edmond MB, Wallace SE, McClish DK, Pfaller MA, Jones RN, Wenzel RP. Nosocomial bloodstream infections in United States hospitals: a three-year analysis. Clin Infect Dis. 1999. 29:239–244.

7. Weems JJ Jr. Candida parapsilosis : Epidemiology, pathogenicity, clinical manifestations and antimicrobial susceptibility. Clin Infect Dis. 1992. 14:756–766.

8. Viudes A, Peman J, Canton E, Ubeda P, Gobernado M. Candidaemia at a tertiary-care hospital: epidemiology, treatment, clinical outcome and risk factors for death. Eur J Clin Microbiol Infect Dis. 2002. 21:767–774.

9. Samonis G, Kofteridis DP, Saloustros E, Giannopoulou KP, Ntziora F, Christidou A, Maraki S, Falagas ME. Candida albicans versus non-albicans blood stream infection in patients in a tertiary hospital : an analysis of microbiological data. Scand J infect Dis. 2008. 40:414–419.

10. Pfaller MA, Diekema DJ. Twelves years of fluconazole in clinical practice: global trends in species distribution and fluconazole susceptibility of bloodstream isolates of Candida. Clin Microbiol Infect. 2004. 10:Suppl 1. 11–23.

11. Presterl E, Daxbock F, Graninger W, Willinger B. Changing pattern of candidaemia 2001-2006 and use of antifungal therapy at the University Hospital of Vienna, Austria. Clin Microbiol Infect. 2007. 13:1072–1076.

12. Thuraisingam AI, Denning DW. Candida glabrata oesophagitis in a patient without HIV infection. Eur J Clin Microbiol Infect Dis. 2000. 19:561–562.
13. Drago M, Scaltrito MM, Morace G. GISIA-2 Group. In vitro activity of voriconazole and other antifungal agents against clinical isolates of Candida glabrata and Candida krusei. Eur J Clin Microbiol Infect Dis. 2004. 23:619–624.

14. Tumbarello M, Sanguinetti M, Trecarichi EM, La Sorda M, Rossi M, De Carolis E, De Gaetano Donati K, Fadda G, Cauda R, Posteraro B. Fungaemia caused by Candida glabrata with reduced susceptibility to fluconazole due to altered gene expression: risk factors, antifungal treatment and outcome. Antimicrob Chemother. 2008. 62:379–385.
15. National committee for clinical laboratory standards. Reference method for broth dilution antifungal susceptibility testing of conidium-forming filamentous fingi. Proposed standard M38-P. 1998. Villanova, Pa: National Committee for clinical laboratory standards.
16. White TC, Marr KA, Bowden RA. Clinical, cellular, and molecular factors that contribute to antifungal drug resistance. Clin Microbiol Rev. 1998. 11:382–402.

17. Yacoub WN, Sohn HJ, Chan S, Petrosyan M, Vermaire HM, Kelso RL, Towfigh S, Mason RJ. Psoas abscess rarely requires surgical intervention. Am J Surg. 2008. 196:223–227.

18. Charalampopoulos A, Macheras A, Charalabopoulos A, Fotiadis C, Charalabopoulos K. Iliopsoas abscesses: Diagnostic, aetiologic and therapeutic approach in five patients with a literature review. Scand J Gastroenterol. 2009. 19:1–6.

19. Fukuhara S, Nishimura K, Yoshimura K, Okuyama A, Yamato M, Kawamori D, Matsuhisa M. A case of psoas abscess caused by Candida albicans. Hinyokika Kiyo. 2003. 49:141–143.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download