Abstract
Streptomycin is currently utilized to treat advanced tuberculosis in Korea. However, the usefulness of intravascular streptomycin is not fully understood. In this study, streptomycin was administered intravenously in 30 patients. Intravenous administration of streptomycin may be a useful route of administration without undesirable toxicities.
According to the Korean national tuberculosis (TB) incidence survey data from 1965 to 1995, the overall risk of TB infection and the incidence of positive acid fast bacillus(AFB) culture have been shown to have decreased to 7.5% and 6.8% per annum, respectively. However, 44,174 new TB cases have been reported in 2008 (90.9 per 100,000), and the incidence showed typical twin peak TB prevalence: 94.8/100,000 in the twenties and 281.8/100,000 in the seventies (1). Moreover, resistance rate to the primary TB drugs in Korea has been increasing and this trend may be an indication of emerging multiple drug resistance(MDR) and extensive drug resistance (XDR) TB in the future (2).
Streptomycin (SM), an aminoglycoside antibiotic, has been used for the treatment of Mycobacterium tuberculosis infection since 1948. However, the use of SM as a primary therapy has been replaced by the subsequent introduction of oral drugs such as isoniazid, rifampin, ethambutol, and pyrazinamide.
Recently, SM attracted attention as an effective TB drug in this era of increasing MDR (3-6). Generally, SM is given intramuscularly (IM) to avoid possible development of toxicities associated with intravenous (IV) SM infusion. However, IV infusion has become a frequent alternative route of administration at some centers (4, 7). The usefulness of IV infusion of SM has not been fully documented. In this study, we assessed the clinical usefulness of IV administration of SM by monitoring the incidences of acute adverse effects, renal, vestibular, and auditory toxicities.
Patients with confirmed pulmonary TB receiving primary or secondary therapy at National Medical Center, Seoul, Republic of Korea, from May, 2008 to February, 2009 were enrolled. Each patient signed an informed consent. This study was approved by the institutional review board of the National Medical Center. The medical history and the findings of physical examinations (including data on renal disease, hearing loss, and neurologic problems), blood chemistry, hematologic analysis, the results of vestibular function testing, and audiogram findings were recorded for all patients at baseline. Patients with unstable renal function, estimated creatinine clearance of <30 mL/min, or allergy to aminoglycoside were excluded from the study. SM (diluted in 100 mL of water with 5% dextrose or normal saline) was administered intravenously over 30 min, 5 times a week (15 mg/kg q.d.: total dosage of 75 mg/kg per week). Patients were monitored during the first week to check for any acute adverse reactions including circumoral numbness, tingling, facial flushing, and headache developing immediately and/or at 2 hours after IV administration. Blood chemistry tests, including blood urea nitrogen, serum creatinine, calcium, magnesium, alanine aminotransferase, and aspartate aminotransferase, were performed weekly. Tests for vestibular function, caloric, Romberg, heel to toe, nystagmus, and evaluation of subjective symptoms (dizziness, nausea, balance change) were performed weekly. An audiogram was checked every 2 weeks to test bilateral hearing at 250, 500, 1000, 2000, 4000, and 8000 Hz. Serum creatinine level >1.2 mg/dL was set as an indication of nephrotoxicity and monitored throughout the study. Vestibular toxicity was defined as any positive result in the vestibular function test. Ototoxicity was defined as >20-db neurosensory hearing loss from the baseline in either one of the ears at any frequency.
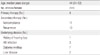
Patient characteristics are shown in Table 1; among a total of 30 subjects, 90% were male and 10% were female, with the mean age of 44 years. Seventy-three percent of patients were below ideal body weight with decreased skeletal muscle mass. Seventy percent of patients, including 9 patients with MDR, were on secondary t herapy. Thirty percent of patients on primary therapy, including those with large lung cavities (6 cases), pleural effusion (2 cases), and pyothorax (1 case) had very advanced TB.
Primary anti-TB medication regimen included isoniazid, rifampin, ethambutol, pyrazinamide plus SM. Cycloserine, prothionamide, para-aminosalicylic acid, and levofloxacin plus SM were used as secondary therapy. SM was administered intravenously for 2-6 weeks (median duration, 3 weeks) with the doses of 500-1,000 mg (median dose, 875 mg). Table 2 shows concurrent anti-TB medications, duration, and dose of IV SM infusion.
Acute adverse reactions, such as circumoral numbness, tingling, facial flushing, and headache were not observed after the first IV infusion. One patient complained of dizziness and nausea during the first 10 minutes of IV infusion. However, symptoms were alleviated after infusion time was increased to over 30 minutes. No incidence of ototoxicity was observed. One patient experienced ringing in the ears but displayed no change from the baseline audiogram and ringing gradually resolved. Vestibular function tests were normal with no balance changes.
Serum creatinine levels were normal (<1.2 mg/dL) and hypocalcemia, hypokalemia or hypomagnesemia were not observed. Table 3 summarizes all toxicities and side effects.
SM has been used for treating pulmonary TB, which requires a prolonged period of administration, often more than 2 months. Thus, patient compliance is the primary concern in treating TB. Traditionally, IM administration of SM has been the gold standard, but concerns about pain and scarring at the injection sites mandated a search for an alternate approach such as IV administration.
Previous pharmacokinetic studies showed that SM was poorly absorbed from the gastrointestinal tract, and thus parenteral administration has been recommended (8, 9). However, pharmacokinetic studies comparing IV and IM administration of SM demonstrated that serum concentrations of SM were not different regardless of the route of administration (8-10). In addition, impure preparations of SM may have contributed to the development of facial flushing and headaches in IV recipients (11). Current SM preparations are superior to the earlier products in terms of purity. Early large scale studies employing administration of SM only through IM route were conducted by the Joint Streptomycin Committee for Tuberculosis (JSCT) and Medical Research Council (MRC). A JSCT study reported that slow IV SM administration was also recommended in addition to the conventional IM method (12). However, the IV SM group showed higher serum concentrations than the IM group at 2 hours after the administration (10, 11). The administration of SM by IM route was not superior to IV route in terms of patient compliance because of pain lasting up to 1 week at the injection site. Moreover, a small percentage of patients showed that prolonged IM administration of SM also caused reversible renal, vestibular, and auditory side effects (9, 13).
Oral TB medications have rapidly replaced SM for primary TB treatment. Recently, SM is gaining popularity again because it can control MDR TB strains. Since 1990, SM has been recommended for patients with advanced or MDR TB (5). The American Thoracic Society (ATS) and the Centers for Disease Control and Prevention(CDC) recommend that patients with TB should initiate therapy with an intensive four-drug regimen, including SM (or ethambutol) in addition to isoniazid, rifampin, and pyrazinamide, to prevent emergence of MDR TB (14, 15).
SM has been typically administrated intramuscularly in Korea. However, intolerable pain and scarring at injection sites may develop with multiple IM injections. While the pain from IV infusion is not as severe as IM injection, long-term treatment (e.g., >2 months) of IV can generate substantial discomfort to patients. Therefore, placing an IV central line can be an option for patients requiring long term TB care. For further evaluation, study with larger study population and longer treatment duration is warranted in the future.
In conclusion, our study suggests that SM can be administered IV without fear of significant toxicities. Therefore, IV infusion of SM could be considered an option for patients who are intolerable to pain caused by IM injection, which can also prevent the occurrence of muscle dystrophy at injection site.
Figures and Tables
References
1. Hong YP, Kim SJ, Lew WJ, Lee EK, Han YC. The seventh nationwide tuberculosis prevalence survey in Korea, 1995. Int J Tuberc Lung Dis. 1998. 2:27–36.
2. Bai GH, Park YK, Choi YW, Bai JI, Kim HJ, Chang CL. Trend of anti-tuberculosis drug resistance in Korea, 1994-2004. Int J Tuberc Lung Dis. 2007. 11:571–576.
3. Centers for Disease Control and Prevention. Initial therapy for tuberculosis in the era of multidrug resistance. Recommendation of the Advisory Council for the Elimination of Tuberculosis. MMWR Recomm Rep. 1993. 42(RR-7):1–8.
5. Ellner JJ, Hinman AR, Dooley SW, Fischl MA, Sepkowitz KA, Goldberger MJ, Shinnick TM, Iseman MD, Jacobs WR Jr. Tuberculosis symposium: emerging problems and promise. J Infect Dis. 1993. 168:537–551.

6. Choi SI, Bae JH, Kong SJ, Park JH. The actual condition of drug-resistant tuberculosis and treatment outcomes at a tuberculosis specialized hospital. Korean J Med. 2006. 70:172–182.
7. Peloquin CA, Berning SE. Comment: intravenous streptomycin. Ann Pharmacother. 1993. 27:1546–1547.

8. Zintel HA, Flippin HF, Nichols AC, Wiley MM, Rhoads JE. Studies on streptomycin in man, absorption, distribution, excretion and toxicity. Am J Med Sci. 1945. 210:421–430.
9. Medical Research Council. Streptomycin treatment of pulmonary tuberculosis. Br Med J. 1948. 2:769–782.
10. Anderson DG, Jewell M. The absorption, excretion, and toxicity of streptomycin in man. N Engl J Med. 1945. 233:485–491.

11. Heilman DH, Heilman FR, Hinshaw HC, Nichols DR, Herrell WE. Streptomycin; absorption, diffusion, excretion and toxicity. Am J Med Sci. 1945. 210:576–584.
12. Herrell WE. Waksman S, editor. Methods of administration and dosage. Streptomycin : nature and practical application. 1949. Baltimore: Williams & Wilkins Co.
13. Joint Streptomycin Committee for Tuberculosis. The effects of streptomycin on tuberculosis in man. JAMA. 1947. 135:634–641.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download