Abstract
Purpose
Patients who treated implant immediate loading within a week after implant placement at Wonkwang University Dental Hospital Implant Center were evaluated marginal bone resorption. These retrospective analyses are intended to reinforce the clinical evidence for the implant immediate loading.
Materials and methods
Medical history and radiographic data were investigated, which were the patients' who treated implant immediate loading and restoration with provisional prostheses between January 2005 and June 2016, at Wonkwang University Dental Hospital Implant Center. Total number of implants was 70, marginal bone resorption was measured according to implant length, diameter and connection type. To measure marginal bone resorption, periapical radiographs were taken when the implants were placed and after 6 month. Statistical analysis was done in Mann-whitney U test and Kruskal-wallis test with SPSS 22.0 software (P<.05).
Results
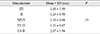
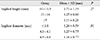
Mean marginal bone resorption around immediately loaded implants according to implant connection type was shown 1.24 ± 0.72 mm in internal hexagon connection type and 1.73 ± 1.27 mm in external hexagon connection type. There was no statically significant difference in marginal bone resorption with implant length and diameter.
Figures and Tables
 | Fig. 2References used to measure the actual marginal bone resorption.B′: marginal bone resorption on digital subtraction image. P′: width of implant platform on digital subtraction image.
B = P × B′ / P′
P: actual width of implant platform (mm)
P′: width of implant platform on digital subtraction image (mm)
B: actual marginal bone resorption (mm)
B′: marginal bone resorption on digital subtraction image (mm)
|
Table 2
Marginal bone resorption around immediate loading implants according to implant connection type

References
1. Cochran DL. The evidence for immediate loading of implants. J Evid Based Dent Pract. 2006; 6:155–163.

2. Bergman B. Evaluation of the results of treatment with osseointegrated implants by the Swedish National Board of Health and Welfare. J Prosthet Dent. 1983; 50:114–115.

3. Buser D, Mericske-Stern R, Dula K, Lang NP. Clinical experience with one-stage, non-submerged dental implants. Adv Dent Res. 1999; 13:153–161.

4. Schnitman PA, Wohrle PS, Rubenstein JE. Immediate fixed interim prostheses supported by two-stage threaded implants: methodology and results. J Oral Implantol. 1990; 16:96–105.
5. Esposito M, Grusovin MG, Maghaireh H, Worthington HV. Interventions for replacing missing teeth: different times for loading dental implants. Cochrane Database Syst Rev. 2013; (3):CD003878.

6. Brånemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, Ohman A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977; 16:1–132.
7. Malchiodi L, Cucchi A, Ghensi P, Nocini PF. Evaluation of the esthetic results of 64 nonfunctional immediately loaded postextraction implants in the maxilla: correlation between interproximal alveolar crest and soft tissues at 3 years of follow-up. Clin Implant Dent Relat Res. 2013; 15:130–142.

8. Chaushu G, Chaushu S, Tzohar A, Dayan D. Immediate loading of single-tooth implants: immediate versus non-immediate implantation. A clinical report. Int J Oral Maxillofac Implants. 2001; 16:267–272.
9. Brägger U, Bürgin W, Lang NP, Buser D. Digital subtraction radiography for the assessment of changes in peri-implant bone density. Int J Oral Maxillofac Implants. 1991; 6:160–166.
10. Queiroz PM, Oliveira ML, Tanaka JL, Soares MG, Haiter-Neto F, Ono E. Assessment of three methods of geometric image reconstruction for digital subtraction radiography. Dentomaxillofac Radiol. 2016; 45:20160120.

11. Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, Trisi P, Steigmann M, Rebaudi A, Palti A, Pikos MA, Schwartz-Arad D, Choukroun J, Gutierrez-Perez JL, Marenzi G, Valavanis DK. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008; 17:5–15.

12. Galindo-Moreno P, Fernández-Jiménez A, O'Valle F, Monje A, Silvestre FJ, Juodzbalys G, Sánchez-Fernández E, Catena A. Influence of the crown-implant connection on the preservation of peri-implant bone: a retrospective multifactorial analysis. Int J Oral Maxillofac Implants. 2015; 30:384–390.

13. Tsouknidas A, Lympoudi E, Michalakis K, Giannopoulos D, Michailidis N, Pissiotis A, Fytanidis D, Kugiumtzis D. Influence of alveolar bone loss and different alloys on the biomechanical behavior of internal-and external-connection implants: A three-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2015; 30:e30–e42.

14. Chun HJ, Shin HS, Han CH, Lee SH. Influence of implant abutment type on stress distribution in bone under various loading conditions using finite element analysis. Int J Oral Maxillofac Implants. 2006; 21:195–202.
15. Buser D, Mericske-Stern R, Bernard JP, Behneke A, Behneke N, Hirt HP, Belser UC, Lang NP. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implants Res. 1997; 8:161–172.

16. Ellegaard B, Kølsen-Petersen J, Baelum V. Implant therapy involving maxillary sinus lift in periodontally compromised patients. Clin Oral Implants Res. 1997; 8:305–315.

17. Feldman S, Boitel N, Weng D, Kohles SS, Stach RM. Five-year survival distributions of short-length (10 mm or less) machined-surfaced and Osseotite implants. Clin Implant Dent Relat Res. 2004; 6:16–23.

18. Lemmerman KJ, Lemmerman NE. Osseointegrated dental implants in private practice: a long-term case series study. J Periodontol. 2005; 76:310–319.

19. Pierrisnard L, Renouard F, Renault P, Barquins M. Influence of implant length and bicortical anchorage on implant stress distribution. Clin Implant Dent Relat Res. 2003; 5:254–262.

20. Degidi M, Piattelli A. Immediate functional and non-functional loading of dental implants: a 2- to 60-month follow-up study of 646 titanium implants. J Periodontol. 2003; 74:225–241.

21. Ding X, Zhu XH, Liao SH, Zhang XH, Chen H. Implant-bone interface stress distribution in immediately loaded implants of different diameters: a three-dimensional finite element analysis. J Prosthodont. 2009; 18:393–402.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download