Abstract
Purpose
This study was conducted to obtain difference in fracture strength according to the diameter of one-body O-ring-type of mini implant fixture, to determine the resistance of mini implant to masticatory pressure, and to examine whether overdenture using O-ring type mini implant is clinically usable to maxillary and mandibular edentulous patients.
Materials and methods
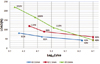
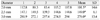
For this study, 13 mm long one body O-ring-type mini implants of different diameters (2.0 mm, 2.5 mm and 3.0 mm) (Dentis, Daegu, Korea) were prepared, 5 for each diameter. The sample was placed at 30° from the horizontal surface on the universal testing machine, and off-axis loading was applied until permanent deformation occurred and the load was taken as maximum compressive strength. The mean value of the 5 samples was calculated, and the compressive strength of implant fixture was compared according to diameter. In addition, we prepared 3 samples for each diameter, and applied loading equal to 80%, 60% and 40% of the compressive strength until fracture occurred. Then, we measured the cycle number on fracture and analyzed fatigue fracture for each diameter. Additionally, we measured the cycle number on fracture that occurred when a load of 43 N, which is the average masticatory force of complete denture, was applied. The difference on compressive strength between each group was tested statistically using one-way ANOVA test.
Results
Compressive strength according to the diameter of mini implant was 101.5 ± 14.6 N, 149 ± 6.1 N and 276.0 ± 13.4 N, respectively, for diameters 2.0 mm, 2.5 mm and 3.0 mm. In the results of fatigue fracture test at 43 N, fracture did not occur until 2×106 cycles at diameter 2.0 mm, and until 5×106 cycles at 2.5 mm and 3.0 mm.
Conclusion
Compressive strength increased significantly with increasing diameter of mini implant. In the results of fatigue fracture test conducted under the average masticatory force of complete denture, fracture did not occur at any of the three diameters. All of the three diameters are usable for supporting overdenture in maxillary and mandibular edentulous patients, but considering that the highest masticatory force of complete denture is 157 N, caution should be used in case diameter 2.0 mm or 2.5 mm is used.
Figures and Tables
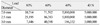
 | Fig. 6Permanent deformed mini implants caused by static loading test. A: ∅2.0 mm, B: ∅2.5 mm, C: ∅3.0 mm. |
References
1. Albrektsson T, Braånemark PI, Hansson HA, Lindstro¨m J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981. 52:155–170.

2. Buser D, Mericske-Stern R, Bernard JP, Behneke A, Behneke N, Hirt HP, Belser UC, Lang NP. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implants Res. 1997. 8:161–172.

3. Davarpanah M, Martinez H, Tecucianu JF, Celletti R, Lazzara R. Small-diameter implants: indications and contraindications. J Esthet Dent. 2000. 12:186–194.

4. Zinsli B, Sa¨gesser T, Mericske E, Mericske-Stern R. Clinical evaluation of small-diameter ITI implants: a prospective study. Int J Oral Maxillofac Implants. 2004. 19:92–99.
5. Barber HD, Seckinger R. The role of the small diameter implant: a preliminary report on the mini implant system. Compendium. 1994. 15:1390–1392.
6. Cho YS. The comparison of compression strength of the smallest implant various diameter mini-implants. 2008. Korea: Yonsei University School of Dentistry;MS Thesis.
7. Michael CG, Javid NS, Colaizzi FA, Gibbs CH. Biting strength and chewing forces in complete denture wearers. J Prosthet Dent. 1990. 63:549–553.

8. Shatkin TE, Shatkin S, Oppenheimer BD, Oppenheimer AJ. Mini dental implants for long-term fixed and removable prosthetics: a retrospective analysis of 2514 implants placed over a five-year period. Compend Contin Educ Dent. 2007. 28:92–99.
9. Bulard RA, Vance JB. Multi-clinic evaluation using mini-dental implants for long-term denture stabilization: a preliminary biometric evaluation. Compend Contin Educ Dent. 2005. 26:892–897.
10. Cho SC, Froum S, Tai CH, Cho YS, Elian N, Tarnow DP. Immediate loading of narrow-diameter implants with overdentures in severely atrophic mandibles. Pract Proced Aesthet Dent. 2007. 19:167–174.
11. Tagger Green N, Machtei EE, Horwitz J, Peled M. Fracture of dental implants: literature review and report of a case. Implant Dent. 2002. 11:137–143.

12. Binon PP, McHugh MJ. The effect of eliminating implant/abutment rotational misfit on screw joint stability. Int J Prosthodont. 1996. 9:511–519.
13. Allum SR, Tomlinson RA, Joshi R. The impact of loads on standard diameter, small diameter and mini implants: a comparative laboratory study. Clin Oral Implants Res. 2008. 19:553–559.

14. Kanie T, Nagata M, Ban S. Comparison of the mechanical properties of 2 prosthetic mini-implants. Implant Dent. 2004. 13:251–256.

15. Park WJ, Cho IH. Fatigue fracture of different dental implant system under cyclic loading. J Korean Acad Prosthodont. 2009. 47:424–434.

16. Huang HM, Tsai CM, Chang CC, Lin CT, Lee SY. Evaluation of loading conditions on fatigue-failed implants by fracture surface analysis. Int J Oral Maxillofac Implants. 2005. 20:854–859.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download