Abstract
Continuous venovenous hemodiafiltration (CVVHDF) was used to eliminate pentobarbital from the blood of a 30-year-old potentially brain dead male patient with traumatic intracranial hemorrhage after a motorcycle accident. The Acute Physiology and Chronic Health Evaluation (APACHE) II score of hospital day 1 was 24, but by day 8 it was 36, when the patient was considered to be brain dead. To control seizures and reduce intracranial pressure, pentobarbital had been administered in a continuous flow (2,880 mg/day for 5 days). Coma can be induced by pentobarbital at a serum level of 1~5 mg/dL. However, drug intoxication should be excluded from a brain death evaluation; therefore, the patient was not given any drug for approximately 88 hrs after ceasing pentobarbital in order for serum level to dip below 0.5 mg/dL (which is the hypnotic level). At 48 hours from CVVHDF, the pentobarbital level was close to the hypnotic level (0.1~0.5 mg/dL). Before stopping, the serum level of pentobarbital was 3.89 mg/dL and between 48 and 72 hours from CVVHDF, 4 cycles of pentobarbital half-life elimination (0.24 mg/dL) could be measured. Therefore, we suggest that in case of potential brain dead patients who have been administered pentobarbital, CVVHDF can enhance the elimination of pentobarbital from the circulatory system and shorten the waiting time for a brain death evaluation.
Pentobarbital is short acting barbiturate with sedative, hypnotic, and anticonvulsant properties(1). Patients with severe traumatic brain injury resulting in increased intracranial pressure, barbiturate-induced coma can be used in an attempt to reduce intracranial pressure by suppressing cerebral metabolism, consequently reducing cerebral metabolic demands and cerebral blood volume(2,3). Therefore, many potential brain dead donors commonly referred from the department of neurosurgery which manages traumatic brain injury were eventually administered pentobarbital intravenously.
For diagnosis of brain death, prerequisite conditions are exclusion of complicating medical condition that may confound clinical assessment (electrolyte, acid base, and endocrine imbalances), no drug intoxication or poisoning, and core temperature above 35℃. All neurologic and metabolic states that can mimic brain death should be eliminated(4). At a level of serum pentobarbital 1~5 mg/dL can induce coma and dose-dependent respiratory depression(1). Therefore, if the serum pentobarbital level cannot be quantified, the patient should be observed at least four times the elimination half-life of the pentobarbital(4). The half-life elimination of pentobarbital is about 22 hours (range; 15~50 hours) in healthy adults(5). If serum pentobarbital level cannot be measured, we should wait 88 hours for bringing the sedative drug level down to 0.1~0.5 mg/dL before evaluating brain death(4).
In Korea, there is no hospital that can measure the pentobarbital serum level, therefore, presumed brain death patient administered with pentobarbital should wait for a long duration before diagnosis of brain death. There are several case reports on the use of hemodialysis or peritoneal dialysis for enhancing pentobarbital clearance in pentobarbital intoxication(6-10). Continuous venovenous hemodiafiltration (CVVHDF) is a mode of continuous renal replacement therapy (CRRT) commonly used in unstable critically ill patients in intensive care units (ICU) and it can be very useful for hemodynamically unstable brain dead patients(11).
We report the use of CVVHDF for enhancing clearance of pentobarbital in a presumed brain dead patient before the evaluation of brain death.
A 30-year-old male patient (165 cm/56 kg) with epidural hematoma and subdural hematoma due to a motorcycle traffic accident was admitted to the department of neurosurgery. Acute Physiology and Chronic Health Evaluation (APACHE) II score of on hospital admission day 1 (HOD1) was 24. His initial mental state was semicoma and emergency subdural hematoma removal was performed. On HOD2, follow-up brain computed tomography (CT) scan showed increased intracranial hemorrhage and brain swelling. Decompressive craniectomy was performed again. But brain swelling was not subsided. Thus, for reduction of intracranial pressure and seizure control, intravenous pentobarbital infusion was administered continuously at a rate of 2 mg/kg/hr (total 2,880 mg/day) for 120 hours. On HOD8, 3rd craniectomy was performed from 11:30 AM to 1:10 PM. Operation was stopped in the middle of the procedure because of the brain swelling with massive bleeding and severe hypoxemia (<PaO2 40 mmHg) even with 100% oxygen. Total 2,200 mL of crystalloid solution and 3,070 mL of blood products were infused during operation. In the intensive care unit, more 1,100 mL of colloid and 900 mL of crystalloid were infused from the end of operation until the start of CVVHDF. After operation, there was no self respiration and no brain stem reflexes, and his mental status was assessed as coma. Under the brain death impression, the patient was consulted to the brain death management team and consequently referred. At this point, he was on HOD8 and the APACHE II score was 36.
Even after high dose of vasopressor and administration of 100% O2, the patient was in severe hypoxemic status and was hemodynamically unstable; The symptom includes lactic acidosis and acute renal failure (ARF) (Table 1). High amounts of pentobarbital was also administered (2,880 mg/day for 5 days). Therefore, the patient needed continuous renal replacement therapy (CRRT). Because of the patient's poor condition, CVVHDF was chosen as CRRT modality for improving the hemodynamically instability and enhancing the clearance of pentobarbital. In Korea, there are no hospitals where can measure serum pentobarbital level. Therefore, we should wait 88 hours for evaluating brain death.
On the HOD8, pentobarbital was stopped after 3rd operation at 2 PM. CVVHDF was started at 6 PM on the same day. CVVHDF was performed through a dual lumen femoral catheter using the Prisma system (Prisma, Gambro-Hospal, Lund, Sweden) with a blood flow of 150 mL/hr, dialysate flow rate of 800 mL/hr and replacement flow rate of 1,200 mL/hr. We used biocompatible membrane with 1.0 m2 filter (AN69ST, Gambro-Hospal, Meyzieu, France). Replacement fluid (Haemosol-B0, Gambro-Hospal, Sondalo, Italy) was administered prefilter method. Anticoagulation with regional heparization was administered and flow rates remained constant during the entire therapy. CVVHDF was applied from HOD8 to HOD12, and the total duration of therapy was 120 hours.
Pentobarbital levels were measured 10 times from the radial arterial blood line; before stopping pentobarbital, just before starting CVVHDF, and 4, 8, 12, 24, 36, 48, 72, 96 hours after the starting CVVHDF. These specimens were sent to Korea Institute of Science and Technology (KIST) and results were obtained after one week. The drug levels were measured with high performance liquid chromatography (HPLC) and were as shown in Table 2 and Fig. 1. After decreasing pentobarbital levels and removing cytokine and toxic materials by CVVHDF, the patient showed clinical improvement and resumed self respiration. That means the patient was not brain death and was transferred back to the department of Neurosurgery on the HOD13, and eventually the patient expired 2 months later.
Pentobarbital is short acting barbiturate, molecular weight of 232 Dalton, lipid solubility (partition coefficient) 32, plasma protein binding 35%, brain protein binding 29%, volume of distribution 0.9 L/kg body weight, and metabolized by the liver and mostly excreted in urine. Because pentobarbital has high solubility, when administered for a long term period, pentobarbital tends to deposit throughout the brain and fat tissue(12,13). Instead of choosing serum level of 2.5 mg/dL which was the serum level prior to start CVVHDF, the level of 3.89 mg/dL was chosen as a basal level which was obtained at 6 AM on HOD8. The reason was the dilutional effect of serum pentobarbital; during 3 hours of operation, 5,270 mL of fluids, and during 5 hours before start of CVVHDF, 2,000 mL of fluids were infused.
When large amounts of sedative and anesthetic agents are ingested, they can cause a partial loss of brain-stem reflexes and can mimic brain death. Especially, intoxication with tricyclic antidepressants and barbiturates can induce very similar conditions to brain death(14,15). Therefore, we should exclude these confounding conditions before an accurate diagnosis of brain death. However, in real clinical situations, there is no ways to measure serum pentobarbital level in any hospital in Korea. Therefore, in case of pentobarbital coma therapy, we should wait at least 88 hours (four times the half-life elimination of the drug) after stopping the drug.
Brain death upregulates multiple lymphocyte and macrophage-derived cytokines and the injured brain itself may be the source of proinflammatory factors such as S100B(16). The sepsis syndrome is associated with an overwhelming, systemic overflow of proinflammatory and anti-inflammatory mediators(12-14). According to the Surviving Sepsis Campaign, they suggest the use of CRRT to facilitate management of fluid balance in hemodynamically unstable septic patients(17). During CVVHDF, small, medium and large solutes could be removed by mixed diffusion (up to 1 kDa) and convection (up to 35 kDa)(18).
CVVHDF has been used not only for poisoning such as barbiturates, ethylene glycol and lithium(15,16) but also for the treatment of shock and brain death(17,19). While the patient was on CVVHDF, we achieved a half life elimination time between 12 to 24 hours from CVVHDF. However, the drug level of half elimination was 1.95 mg/dL, and it was much closer to the drug level at 12 hours from CVVHDF (2.02 mg/dL) than the drug level at 24 hours from CVVHDF (1.31 mg/dL). 48 hours after starting CVVHDF, the pentobarbital level (0.53 mg/dL) was close to hypnotic level (0.1~0.5 mg/dL). Between 48 hours and 72 hours after starting CVVHDF, 4 times of half-life elimination of pentobarbital (0.24 mg/dL) was reached. Therefore, by applying the CVVHDF, four times of the elimination half-life of pentobarbital could be shortened to less than 72 hours.
Bironneau et al.(20) reported that the clearance of pentobarbital was enhanced with greater blood flow rate and effluent rates. We set the CVVHDF at a blood flow of 150 mL/hr, dialysate flow rate of 800 ml/hr and replacement flow rate of 1,200 mL/hr. If we increased the blood flow rate and the dialysate flow rate, the hypnotic drug level could possibly be reached earlier. If the appropriate setting of CVVHDF for elimination of pentobarbital is determined, this will significantly help the brain dead donor management team.
Brain dead patients often show hemodynamic instabilities and severe acid-base imbalances. Sometimes, it is difficult to maintain vital signs for only one or two days before organ harvest. Therefore, in the shortage of organ donor, brain death patients with pentobarbital administration, shortening the waiting time before evaluation of brain death is very important. For the brain dead donor management team, the most updated guideline should be applied, which includes 88 hours of waiting time prior to evaluate brain death in case of CVVHDF application.
In conclusion, in the case of brain dead patients administered with pentobarbital, CVVHDF can enhance the clearance of pentobarbital and shorten the waiting time for brain death evaluation.
Figures and Tables
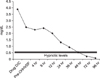 | Fig. 1This figure shows sequence of serum pentobarbital levels from during pentobarbital infusion, before CVVHDF, and after CVVHDF time sequences. After 48 hours CVVHDF start the serum pentobarbital levels were down to hypnotic levels (0.1~0.5 mg/dL). Abbreviation: CVVHDF, continuous venovenous hemodiafiltration. |
References
1. Lacy CF, et al. American Pharmacists Association. Drug information handbook: a comprehensive resource for all clinicians and healthcare professionals, 19th ed. (2010-2011). c2010. Hudson, Ohio; [Washington, D.C.]: Lexi-Comp; American Pahrmacists Association;1209–1211.
2. Roberts I. Barbiturates for acute traumatic brain injury. Cochrane Database Syst Rev. 2000. CD000033.

3. Chen HI, Malhotra NR, Oddo M, Oddo M, Heuer GG, Levine JM, et al. Barbiturate Infusion for intractable intracranial hypertension and its effect on brain oxygenation. Neurosurgery. 2008. 63:880–887. discussion 886-7.

5. Wikipedia. Pentobarbital [Internet]. 2010. cited 2010 Dec 20. San Francisco, CA: Wikimedia Foundation, Inc.;Available from: http://en.wikipedia.org/wiki/Pentobarbital.
6. Berman LB, Vogelsang P. Removal rates for barbiturates using two types of peritoneal dialysis. N Engl J Med. 1964. 270:77–80.

7. Hudson JB, Dennis AJ Jr, Hobbs DR, Sussman HC. Extended hemodialysis in short acting barbiturate poisoning: case report. South Med J. 1969. 62:457–460.
8. Chow-Tung E, Lau AH, Vidyasagar D, John EG. Clearance of phenobarbital by peritoneal dialysis in a neonate. Clin Pharm. 1982. 1:268–271.
9. Wermeling D, Record K, Bell R, Porter W, Blouin R. Hemodialysis clearance of pentobarbital during continuous infusion. Ther Drug Monit. 1985. 7:485–487.
10. Porto I, John EG, Heilliczer J. Removal of phenobarbital during continuous cycling peritoneal dialysis in a child. Pharmacotherapy. 1997. 17:832–835.
11. Lal R, Faiz S, Garg RK, Baweja KS, Guntupalli J, Finkel KW. Use of continuous venovenous hemodiafiltration in a case of severe phenobarbital poisoning. Am J Kidney Dis. 2006. 48:e13–e15.

12. Harvey SC. Goodman LS, Gilman A, editors. Hypnotics and sedatives: the barbiturates. The pharmacological basis of therapeutics. 1975. 5th ed. New York: Macmillan;102–123.
13. Trevor AJ, Way WL. Katzung BG, editor. Sedative-Hypnotics. Basic and clinical pharmacology. 1982. Los Altos: Lange;221–230.
14. Grattan-Smith PJ, Butt W. Suppression of brainstem reflexes in barbiturate coma. Arch Dis Child. 1993. 69:151–152.

15. Yang KL, Dantzker DR. Reversible brain death. A manifestation of amitriptyline overdose. Chest. 1991. 99:1037–1038.
16. Venkataraman R, Song M, Lynas R, Kellum JA. Hemoadsorption to improve organ recovery from brain-dead organ donors: a novel therapy for a novel indication? Blood purify. 2004. 22:143–149.

17. Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008. 36:296–327. Erratum in: Crit Care Med 2008;36:1394-6.

18. Belloma R, D'Intini V, et al. Fink MP, Abraham E, editors. Renal replacement therapy in the ICU. Textbook of critical care. 2005. 5th ed. Philadelpia: Elsevier Saunders;1151–1158.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download