Abstract
Neisseria gonorrhoeae is the causative agent of gonorrhea, one of the most important sexually transmitted diseases. The incidence of gonorrhea is still prevalent and about 50,000 new cases have been reported annually during the late 2000s in Korea. The antimicrobial resistance of N. gonorrhoeae is very prevalent and most isolates are multi-drug resistant to penicillin G, tetracycline, and fluoroquinolones. The incidence of penicillinase-producing N. gonorrhoeae (PPNG) decreased significantly, but high-level tetracycline-resistant N. gonorrhoeae (TRNG) increased recently. The minimum inhibitory concentrations (MICs) of ceftriaxone were within the susceptible range for all isolates, but MIC creep has been apparent and one cefixime-nonsusceptible isolate (0.5 µg/ml) was found. Spectinomycin-resistant isolates remain rare, but caution should be required when dealing with gonococcal pharyngitis.
Neisseria gonorrhoeae is the causative agent of gonorrhea, one of the most important sexually transmitted diseases and results in a wide range of diseases from asymptomatic infection to severe complications (1). Humans are the only hosts of this pathogen, and N. gonorrhoeae is always considered pathogenic even in asymptomatic patients. Most common type of infection is acute urethritis in men and endocervicitis in women, but up to 10% of men and many women may be asymptomatic. Most cases of untreated infections resolve spontaneously after several weeks, but severe complications such as pelvic inflammatory diseases and disseminated gonococcal infections may occur.
The prevalence of N. gonorrhoeae infection has decreased in many developed countries during the past few decades (2~4), but it is still high in many developing countries (5). According to the global estimation by the World Health Organization in 2011, 88 million new cases of gonococcal infections have been reported annually (6). The incidence of gonorrhea seemed to decrease in Korea recently according to the data from the Korean Centers for Disease Control and Prevention (7), but the data from the Korea Health Insurance Review and Assessment Service showed that gonorrhea is still prevalent and about 50,000 new cases have been reported annually during the late 2000s in Korea. Moreover, gonorrhea is very problematic in certain patient groups, such as adolescents in youth shelters (8). The prevalence of gonorrhea among university students was as low as 0.4% (9), but adolescents who had a sexual experience in youth shelters showed very high prevalence of 28% by polymerase chain reaction in 2004 in Korea (8).
Historically, gonorrhea has been a community-acquired disease and treated empirically at a primary-care hospital, and it has responded well to antimicrobial agents such as penicillin G and fluoroquinolones. However, the emergence of antimicrobial resistance in N. gonorrhoeae has compromised the treatment and control of the disease (10, 11). Due to the recent use of molecular diagnostic methods, the routine isolation and susceptibility testing of N. gonorrhoeae are performed rarely; therefore, it is hard to select optimal antibiotics in clinical settings. Therefore, surveillance program of antimicrobial resistance is required to establish the guideline for empirical treatment and control of gonococcal infection. The antimicrobial resistance of N. gonorrhoeae has been a serious problem in Korea (12~17). In this review, we discussed the current status of antimicrobial resistance of N. gonorrhoeae and of gonococcal infection in Korea.
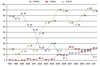
N. gonorrhoeae had been highly-susceptible to penicillin G. However, penicillin G lost its clinical usefulness rapidly since the clinical treatment failure of penicillin was reported in the 1950s in Korea (18). The annual rate of penicillin-susceptible N. gonorrhoeae collected during 1966-1975 varied from 7.7% to 26.7%, and the average rate of susceptible isolates during that period was only 12.1% in Korea (19). Resistance to penicillin G became more serious and no susceptible isolates were detected since the 1990s (12). Penicillin G resistance in N. gonorrhoeae is due to two different mechanisms: one is plasmid-mediated β-lactamase production (penicillinase-producing N. gonorrhoeae, PPNG) and another is changes in amino acid sequences in penicillin-binding protein (PBP) encoded by chromosomes (chromosomally-mediated penicillin-resistant N. gonorrhoeae, CMRNG). PPNG produces TEM-1 type β-lactamase, which confers high level resistance to penicillin G. The prevalence of PPNG increased steadily until the 1990s and remained high in many Asian countries as compared to most developed countries (20, 21). In Korea, the first case of PPNG was isolated in the US armed forces personnel, but he had a history of contract with the infection not in Korea but in South-East Asia where PPNG appeared for the first time (22). The true first case was isolated from 51-year-old housewife in Seoul in 1979, and it was supposed that PPNG occurred within Korea because both the patient and her husband had never traveled abroad (22). The proportion of PPNG steadily increased during the 1980s and 1990s and reached 84% in 1999 (Fig. 1), but decreased rapidly in the 2000s (12~17). The decline was also reported in other countries such as Hong Kong (23~25), but the exact cause was not known. Although the prevalence of PPNG decreased, all non-PPNG isolates was non-susceptible to penicillin G with elevated minimum inhibitory concentrations (MICs), indicating that penicillin G cannot be used to treat gonorrheal infection (14~17).
Tetracycline is another historical antimicrobial agent used to treat gonococcal infection but is no longer used. Tetracycline resistance arose from chromosomal mutations in tet, penB, and mtrR genes (low-level resistance) and acquisition of a conjugative tetM-containing plasmid (high-level tetracycline-resistant N. gonorrhoeae, TRNG) from other isolates (26). Although tetracycline is no longer prescribed as a treatment option, susceptibility to tetracycline can be tested routinely because the isolation trend of TRNG may be useful for epidemiologic studies. In Korea, tetracycline-susceptible isolates have not been detected since the early 1990s (12~17). The rate of TRNG was very low until 2004 (14), but the rate increased during the late 2000s (15~17) and finally reached to 22% in our 2011 study (Fig. 1), (unpublished data). The reason for the recent increase of TRNG is not clear, but the changes in epidemiology in gonococcal infection seemed to have happened and further investigation may be required.
Fluoroquinolones, such as ciprofloxacin and ofloxacin, started to be used for gonorrhea in the mid-1980s (27) and was one of the recommended drugs in the 1990s (28) because it had several advantages: it could be used orally in a single dose regimen and was highly concentrated in urine (29~31). However, frequent use of fluoroquinolones resulted in a wide spread of resistance (31, 32). In Korea, fluoroquinolone susceptibility was as high as 91% in 1992, but it rapidly decreased to 46% in 1996 (12). With continuous decrease of susceptible isolates, the resistance rate increased from 20% in 1997 (13) to 88% in 2011 in our present study (Fig. 1), (unpublished data). Fluoroquinolone resistance was mainly due to mutations in the target sites: the gyrA and parC genes. Most of the fluoroquinolone-resistant isolates had amino acid substitutions at the 91st and 95th positions in GyrA and a single substitution at the 86th or 87th position in ParC (14, 33). Accumulation of these mutations can lead to increased fluoroquinolone resistance. Because of rapid and progressive spread of resistance in clinical isolates, fluoroquinolones have not been recommended in the United States and Korea since 2007 (34~36). However, despite discontinuation of the use of fluoroquinolones, the prevalence of fluoroquinolone-resistant N. gonorrhoeae has not decreased and novel mutations in the gyrA and parC genes continued to be detected. This suggests slow but sustained evolution of the genes as a consequence of selection for fluoroquinolone resistance due to dual therapy for accompanying chlamydial infections. However, importation of strains with new QRDR substitutions is a more possible cause rather than de novo evolution.
Recently, cephalosporins have become one of the most active therapeutic choices for gonococcal infection. Ceftriaxone, cefotaxime, and cefixime are recommended by the Korean guideline for gonorrhea (34). Ceftriaxone is the predominantly used cephalosporin antimicrobial agent in gonococcal infection because of its high intrinsic activity against N. gonorrhoeae together with a long half-life and success in eradicating the organism from all sites of infection (37). Multi-drug resistance to penicillin G, tetracycline, and fluoroquinolone in N. gonorrhoeae led to a slight increase in the use of third-generation cephalosporins and spectinomycin in Korea (14). In 2002, only 9.5% of patients were treated with cephalosporins including parenteral ceftriaxone and oral cefixime. The rate increased to 30% in 2010. As cephalosporin is used more often, resistance to cephalosporin in N. gonorrhoeae has emerged (38~42). A recent Gonococcal Infection Surveillance Program in the U.S. showed an increasing trend of gonococcal isolates with elevated MICs of cefixime (≥0.25 µg/ml) from 0.2% in 2000 to 1.4% in 2010 and of ceftriaxone (≥0.125 µg/ml) from 0.1% in 2000 to 0.3% in 2010 (43). Sustained increase of MIC to near breakpoint within the susceptible range (MIC creep) hinders efficacy of cephalosporin antibiotics in gonorrheal treatment. Because the clinical efficacy of β-lactam antibiotics is related to the periods for which free drug concentration exceeds MIC (ƒT>MIC), increasing MIC decreases ƒT>MIC and clinical failure can arise. The current regimen of ceftriaxone (250 mg) and cefixme (400 mg) may be effective, but the MIC creep and resulting reduction of ƒT>MIC may be a cause of clinical failure in gonorrheal treatment with ceftriaxone and cefixime MICs of 0.125~0.25 µg/ml (44).
Ceftriaxone-resistant N. gonorrhoeae was not reported until 2011, but two cases of ceftriaxone-resistant isolates were reported in Japan (H041 strain, ceftriaxone MIC 2 µg/ml) and France (F89 strain, ceftriaxone MIC 2 µg/ml) in 2011 (45~47). The mechanism of resistance of these two strains was determined and seemed to be associated with novel penA mosaicism. In Korea, all isolates were susceptible to ceftriaxone in an annual successive study that was previously performed and supported by the Korea National Institute of Health. However, MIC creep was apparent (14): more than 32-fold difference was noted between the lowest and the highest MICs. The MIC range of ceftriaxone for N. gonorrhoeae in our previous study was ≤0.008~0.06 µg/ml during 1997 and 1999 (13), but the upper margin of MICs increased to 0.25 µg/ml near the breakpoint in isolates collected during the 2000s (14~17). The proportion of isolates inhibited by ≥0.06 µg/ml of ceftriaxone increased from less than 10% of the isolates from 1997-1999 (13) to 39% of the isolates from 2011 in our present study (unpublished data), and this meant 39% of N. gonorrhoeae isolated in Korea was not susceptible to ceftriaxone by the Australian guideline.
Ceftriaxone had a good activity in treating gonococcal infection, but it had to be given as an intramuscular injection that is locally painful and requires co-administration of a local anesthetic such as lidocaine. For this reason, the use of a number of oral cephalosporins was evaluated. Cefixime is one of the orally absorbed cephalosporins that is not only active against penicillin-resistant N. gonorrhoeae regardless of production of β-lactamase but also has pharmacokinetic activity suitable for single-dose administration. In a randomized unblinded multicenter study reported in 1991, a single dose of oral cefixime appeared to be as effective as ceftriaxone in the treatment of uncomplicated gonorrhea (48). Thereafter, cefixime and other oral cephalosporins such as cefuroxime axetil (49), ceftibuten (50), cefoperazone (51), cefdinir (52), cefpodoxime proxetil (53), and cefaclor (54) were used to treat gonococcal infection in many countries. However, an increasing number of treatment failures with oral cephalosporin regimens, especially with cefixime (55) and ceftibuten (42), were reported recently. Treatment failure with cefixime was reported first in 2001 in Japan, which was 10 years earlier than when ceftriaxone-resistant N. gonorrhoeae was reported in Japan in 2011. Cefixime-resistant N. gonorrhoeae disseminated widely and became common in Japan since 2001, and cefixime was no longer recommended as a treatment option in Japan (56~59). In Korea, cefixime non-susceptible N. gonorrhoeae (cefixime MIC, 0.5 µg/ml) was first isolated in 2004 (60), but there was no additional cefixime non-susceptible strain isolated in a successive study until 2010. This isolate had the identical genetic background and mechanism with isolates that were reported to be cefixime resistant in Japan in 2001.
The mechanism of resistance to cephalosporin has not been completely understood yet, but alterations in PBP2 seem to play an important role in cephalosporin resistance in N. gonorrhoeae. When the first cefixime-resistant N. gonorrhoeae was reported in Japan in 2001, it was suggested that mosaicism (Pattern X) in PBP2 encoded by the penA gene was associated with clinical failure and cefixime resistance because PBP2 was a main target of β-lactam antibiotics in N. gonorrhoeae (55, 61). The relationship between PBP2 alteration and cephalosporin susceptibility was supported by other studies (58, 61~63). In direct assays, mosaic PBP2 showed lower affinity with oral cephalosporins including cefixime and cefdinir than that of non-mosaic-structure PBP2, but affinity with ceftriaxone was not affected (61). In the modeling study, the A501V substitution in PBP2 also induced a conformational alteration of the β-lactam-binding pocket such as mosaic PBP2, making a major contribution to the reduced susceptibility to cephalosporin (58, 62, 63). A recent report on ceftriaxone-resistant N. gonorrhoeae showed that novel PBP2 mosaicism (46) (97.6% similarity with Pattern X) and A501P substitution (47) were also associated with ceftriaxone resistance. However, the mechanism of reduced susceptibility was not explained by penA mosaicism alone. N. gonorrhoeae with the mosaic PBP2 (Pattern X) showed variable MICs for cefixime from susceptible to resistant (56), and all N. gonorrhoeae with A501V were still susceptible to ceftriaxone despite elevated MICs, suggesting that other genetic changes may be needed to provoke resistance to cefixime. Reduced susceptibility of N. gonorrhoeae to cephalosporin was associated with diverse penA mutations, together with mtrR mutations (60). Mutations in the mrtR gene induced the derepression of an efflux pump repressor, and these mutations occurred almost always with an alteration in penB gene that encodes porin proteins (64) and in ponA gene that encodes PBP1. A mutation in recently identified pilQ gene (previously named penC) was also associated with reduced susceptibility of cephalosporins (65), but this mutation has not been observed in clinical settings. Sequential alterations of the penA, mtrR, penB, ponA,and pilQ genes have been shown to induce chromosomally mediated high-level resistance to penicillin and cephalosporin (60, 66).
Spectinomycin is another active antimicrobial agent that is cheap and active in uncomplicated gonorrhea (67). However, spectinomycin has to be administered as an intramuscular injection and can cause treatment failure in gonococcal pharyngitis (68). Although spectinomycin resistance had been reported in Korea in 1986 and 1993 (51), it has been very rare, and spectinomycin-resistant N. gonorrhoeae was not isolated in the 2000s (14~17). For this reason, numerous gonococcal infections were treated with spectinomycin in Korea during the 2000s. However, recent changes in sexual behavior may have caused treatment failure in patients with gonococcal pharyngitis who are treated with spectinomycin (68). These patients may serve as a source of dissemination of gonorrhea and provide the means for in-vivo intragenic transfer in PBP2 between N. gonorrhoeae and other commensal Neisseria species (58).
In Korea, the antimicrobial resistance of N. gonorrhoeae is very severe and most isolates are multi-drug resistant to penicillin G, tetracycline, and fluoroquinolones. The incidence of PPNG decreased significantly, but the incidence of TRNG increased recently. The MICs of ceftriaxone were within the susceptible range for all isolates, but MIC creep was apparent and one cefixime non-susceptible isolate (0.5 µg/ml) was found. Almost all isolates were susceptible to spectinomycin, but caution should be required when dealing with gonococcal pharyngitis.
Figures and Tables
References
1. Versalovic James, Carroll Karen C, Funke Guido, Jorgensen James H., Landry Marie Louise, Warnick David W., editors. Manual of Clinical Microbiology. 2011. 10th ed. Amer Society for Microbiology;559–573.
2. Fenton KA, Lowndes CM. Recent trends in the epidemiology of sexually transmitted infections in the European Union. Sex Transm Infect. 2004. 80:255–263.

3. Van Duynhoven YT. The epidemiology of Neisseria gonorrhoeae in Europe. Microbes Infect. 1999. 1:455–464.
4. Sexually transmitted diseases surveillance 2010. Centers for Disease Control and Prevention (CDC). Last visited on 8 February 2012. http://www.cdc.gov/std/stats10/surv2010.pdf. [Online].
5. Gerbase AC, Rowley JT, Heymann DH, Berkley SF, Piot P. Global prevalence and incidence estimates of selected curable STDs. Sex Transm Infect. 1998. 74:S12–S16.
6. Emergence of multi-drug resistant Neisseria gonorrhoeae-Threat of global rise in untreatable sexually transmitted infections. World Health Organization. Last visited on 8 February 2012. http://whqlibdoc.who.int/hq/2011/WHO_RHR_11.14_eng.pdf [Online].
7. Korean Centers for Disease Control and Prevention (CDC). Sentinel surveillance report. Communicable Diseases Monthly Report. 2007. 18:14.
8. Lee SJ, Cho YH, Ha US, Kim SW, Yoon MS, Bae K. Sexual behavior survey and screening for chlamydia and gonorrhea in university students in South Korea. Int J Urol. 2005. 12:187–193.

9. Lee SJ, Cho YH, Kim CS, Shim BS, Cho IR, Chung JI, et al. Screening for Chlamydia and gonorrhea by strand displacement amplification in homeless adolescents attending youth shelters in Korea. J Korean Med Sci. 2004. 19:495–500.

10. Tapsall JW. Implications of current recommendations for third-generation cephalosporin use in the WHO Western Pacific Region following the emergence of multiresistant gonococci. Sex Transm Infect. 2009. 85:256–258.

11. Lewis DA. The Gonococcus fights back: is this time a knock out? Sex Transm Infect. 2010. 86:415–421.

12. Lee K, Chong Y, Erdenechemeg L, Song K, Shin K. Incidence, epidemiology and evolution of reduced susceptibility to ciprofloxacin in Neisseria gonorrhoeae in Korea. Clin Microbiol Infect. 1998. 4:627–633.

13. Lee K, Shin JW, Lim JB, Kim YA, Yong D, Oh HB, et al. Emerging antimicrobial resistance, plasmid profile and pulsed-field gel electrophoresis pattern of the endonuclease-digested genomic DNA of Neisseria gonorrhoeae. Yonsei Med J. 2000. 41:381–386.

14. Lee H, Hong SG, Soe Y, Yong D, Jeong SH, Lee K, et al. Trends in antimicrobial resistance of Neisseria gonorrhoeae isolated from Korean patients from 2000 to 2006. Sex Transm Dis. 2011. 38:1082–1086.

15. Lee H, Lee SG, Yong D, Jeong SH, Lee YS, Lee K, et al. Antimicrobial susceptibility of cephalosporin to Neisseria gonorrhoeae isolated in Korea: Emergence of cefixime non-susceptible Neisseria gonorrhoeae. Infect Chemother. 2008. 40:Suppl 1. S57.
16. Lee H, Suh Y, Kim HM, Lee Y, Chung KT, Lee YS, et al. Antimicrobial susceptibility of Neisseria gonorrhoeae isolated in Korea in 2008. Korean J Clin Microbiol. 2009. 12:Suppl 1. S115.
17. Lee H, Suh Y, Jong S, Chung KT, Lee YS, Lee K, et al. Antimicrobial susceptibility of Neisseria gonorrhoeae isolated in Korea in 2009. Korean J Clin Microbiol. 2010. 13:Suppl 1. S88.
18. Epstein E. Failure of penicillin in treatment of acute gonorrhea in American troops in Korea. J Am Med Assoc. 1959. 169:1055–1059.

19. Chong Y, Kim SO, Yi KN, Lee SY. Penicillin and tetracycline susceptibility of Neisseria gonorrhoeae strains isolated during 1966 to 1975. Yonsei Med J. 1976. 17:46–51.

20. WHO Western Pacific Programme. Surveillance of antibiotic resistance in Neisseria gonorrhoeae in the WHO Western Pacific and South East Asian regions, 2007-2008. Commun Dis Intell. 2010. 34:1–7.
21. WHO Western Pacific and South East Asian Gonococcal Antimicrobial Surveillance Programmes. Surveillance of antibiotic resistance in Neisseria gonorrhoeae in the WHO Western Pacific and South East Asian Regions, 2009. Commun Dis Intell. 2011. 35:2–7.
22. Chong Y, Park HJ, Kim HS, Lee SY, Ahn DW. Isolation of beta-lactamase-producing Neisseria gonorrhoeae. Yonsei Med J. 1979. 20:133–137.

23. Kam KM, Lo KK, Ho NK, Cheung MM. Rapid decline in penicillinase-producing Neisseria gonorrhoeae in Hong Kong associated with emerging 4-fluoroquinolone resistance. Genitourin Med. 1995. 71:141–144.

24. Su X, Jiang F, Qimuge , Dai X, Sun H, Ye S. Surveillance of antimicrobial susceptibilities in Neisseria gonorrhoeae in Nanjing, China, 1999-2006. Sex Transm Dis. 2007. 34:995–999.

25. Matsumoto T. Trends of sexually transmitted diseases and antimicrobial resistance in Neisseria gonorrhoeae. Int J Antimicrob Agents. 2008. 31:S35–S39.
26. Dillon JA, Yeung KH. Beta-lactamase plasmids and chromosomally mediated antibiotic resistance in pathogenic Neisseria species. Clin Microbiol Rev. 1989. 2:S125–S133.
27. Centers for Disease Control (CDC). 1989 sexually transmitted diseases treatment guidelines. MMWR Morb Mortal Wkly Rep. 1989. 38:Suppl 8. 1–43.
28. Centers for Disease Control and Prevention. 1993 sexually transmitted diseases treatment guidelines. MMWR Recomm Rep. 1993. 42:1–102.
29. Roddy RE, Handsfield HH, Hook EW 3rd. Comparative trial of single-dose ciprofloxacin and ampicillin plus probenecid for treatment of gonococcal urethritis in men. Antimicrob Agents Chemother. 1986. 30:267–269.

30. Scott GR, McMillan A, Young H. Ciprofloxacin versus ampicillin and probenecid in the treatment of uncomplicated gonorrhoea in men. J Antimicrob Chemother. 1987. 20:117–121.

31. Dan M. The use of fluoroquinolones in gonorrhoea: the increasing problem of resistance. Expert Opin Pharmacother. 2004. 5:829–854.

32. Tanaka M, Kumazawa J, Matsumoto T, Kobayashi I. High prevalence of Neisseria gonorrhoeae strains with reduced susceptibility to fluoroquinolones in Japan. Genitourin Med. 1994. 70:90–93.

33. Yong D, Kim TS, Choi JR, Yum JH, Lee K, Chong Y, et al. Epidemiological characteristics and molecular basis of fluoroquinolone-resistant Neisseria gonorrhoeae strains isolated in Korea and nearby countries. J Antimicrob Chemother. 2004. 54:451–455.

34. Centers for Disease Control and Prevention (CDC). Updated to CDCs sexually transmitted diseases treatment guidelines, 2006: fluoroquinolones no longer recommended for treatment of gonococcal. MMWR Morb Mortal Wkly Rep. 2007. 56:332–336.
35. Korea Center for Disease Control & Prevention. Management guidelines for sexually transmitted disease. 2007. 12.
36. Korean Association of Urogenital Tract Infection and Inflammation. Korean guideline for sexually transmitted infections. 2011. 10.
37. Newman LM, Moran JS, Workowski KA. Update on the management of gonorrhea in adults in the United States. Clin Infect Dis. 2007. 44:S84–S101.

38. Akasaka S, Muratani T, Yamada Y, Inatomi H, Takahashi K, Matsumoto T. Emergence of cephem- and aztreonam-high-resistant Neisseria gonorrhoeae that does not produce beta-lactamase. J Infect Chemother. 2001. 7:49–50.

39. Muratani T, Akasaka S, Kobayashi T, Yamada Y, Inatomi H, Takahashi K, et al. Outbreak of cefozopran (penicillin, oral cephems, and aztreonam)-resistant Neisseria gonorrhoeae in Japan. Antimicrob Agents Chemother. 2001. 45:3603–3606.

40. Deguchi T, Yasuda M, Yokoi S, Ishida K, Ito M, Ishihara S, et al. Treatment of uncomplicated gonococcal urethritis by double-dosing of 200 mg cefixime at 6-h interval. J Infect Chemother. 2003. 9:35–39.

41. Yokoi S, Deguchi T, Ozawa T, Yasuda M, Ito S, Kubota Y, et al. Threat to cefixime treatment for gonorrhea. Emerg Infect Dis. 2007. 13:1275–1277.
42. Lo JY, Ho KM, Leung AO, Tiu FS, Tsang GK, Lo AC, et al. Ceftibuten resistance and treatment failure of Neisseria gonorrhoeae infection. Antimicrob Agents Chemother. 2008. 52:3564–3567.

43. Centers for Disease Control and Prevention (CDC). Cephalosporin susceptibility among Neisseria gonorrhoeae isolates-United States, 2000-2010. MMWR Morb Mortal Wkly Rep. 2011. 60:873–877.
44. Chisholm SA, Mouton JW, Lewis DA, Nichols T, Ison CA, Livermore DM. Cephalosporin MIC creep among gonococci: time for a pharmacodynamic rethink? J Antimicrob Chemother. 2010. 65:2141–2148.

45. Ohnishi M, Saika T, Hoshina S, Iwasaku K, Nakayama S, Watanabe H, et al. Ceftriaxone-resistant Neisseria gonorrhoeae, Japan. Emerg Infect Dis. 2011. 17:148–149.
46. Ohnishi M, Golparian D, Shimuta K, Saika T, Hoshina S, Iwasaku K, et al. Is Neisseria gonorrhoeae initiating a future era of untreatable gonorrhea?: detailed characterization of the first strain with high-level resistance to ceftriaxone. Antimicrob Agents Chemother. 2011. 55:3538–3545.

47. Unemo M, Golparian D, Nicholas R, Ohnishi M, Gallay A, Sednaoui P. High-level cefixime- and ceftriaxone-resistant N. gonorrhoeae in Europe (France): novel penA mosaic allele in a successful international clone causes treatment failure. Antimicrob Agents Chemother. 2012. Epub 2011 Dec 12.
48. Handsfield HH, McCormack WM, Hook EW 3rd, Douglas JM Jr, Covino JM, Verdon MS, et al. The Gonorrhea Treatment Study Group. A comparison of single-dose cefixime with ceftriaxone as treatment for uncomplicated gonorrhea. N Engl J Med. 1991. 325:1337–1341.

49. Thorpe EM, Schwebke JR, Hook EW 3rd, Rompalo A, McCormack WM, Mussari KL, et al. Comparison of single-dose cefuroxime axetil with ciprofloxacin in treatment of uncomplicated gonorrhea caused by penicillinase-producing and non-penicillinase-producing Neisseria gonorrhoeae strains. Antimicrob Agents Chemother. 1996. 40:2775–2780.

50. Chong LY, Cheung WM, Leung CS, Yu CW, Chan LY. Clinical evaluation of ceftibuten in gonorrhea. A pilot study in Hong Kong. Sex Transm Dis. 1998. 25:464–467.
51. Kim JH, Ro YS, Kim YT. Cefoperazone (Cefobid) for treating men with gonorrhoea caused by penicillinase producing Neisseria gonorrhoeae. Br J Vener Dis. 1984. 60:238–240.

52. Neu HC, Saha G, Chin NX. Comparative in vitro activity and beta-lactamase stability of FK482, a new oral cephalosporin. Antimicrob Agents Chemother. 1989. 33:1795–1800.

53. Novak E, Paxton LM, Tubbs HJ, Turner LF, Keck CW, Yatsu J. Orally administered cefpodoxime proxetil for treatment of uncomplicated gonococcal urethritis in males: a dose-response study. Antimicrob Agents Chemother. 1992. 36:1764–1765.

54. Crabbé F, Grobbelaar TM, van Dyck E, Dangor Y, Laga M, Ballard RC. Cefaclor, an alternative to third generation cephalosporins for the treatment of gonococcal urethritis in the developing world? Genitourin Med. 1997. 73:506–509.

55. Ameyama S, Onodera S, Takahata M, Minami S, Maki N, Endo K, et al. Mosaic-like structure of penicillin-binding protein 2 Gene (penA) in clinical isolates of Neisseria gonorrhoeae with reduced susceptibility to cefixime. Antimicrob Agents Chemother. 2002. 46:3744–3749.

56. Ito M, Deguchi T, Mizutani KS, Yasuda M, Yokoi S, Ito S, et al. Emergence and spread of Neisseria gonorrhoeae clinical isolates harboring mosaic-like structure of penicillin-binding protein 2 in Central Japan. Antimicrob Agents Chemother. 2005. 49:137–143.

57. Yokoi S, Deguchi T, Ozawa T, Yasuda M, Ito S, Kubota Y, et al. Threat to cefixime treatment for gonorrhea. Emerg Infect Dis. 2007. 13:1275–1277.
58. Osaka K, Takakura T, Narukawa K, Takahata M, Endo K, Kiyota H, et al. Analysis of amino acid sequences of penicillin-binding protein 2 in clinical isolates of Neisseria gonorrhoeae with reduced susceptibility to cefixime and ceftriaxone. J Infect Chemother. 2008. 14:195–203.

59. Japanese Society for Sexually Transmitted Disease. Guidelines for diagnosis and treatment of sexually transmitted disease, 2006. Jpn J Sex Transm Dis. 2006. 17:Suppl 1. 35–39.
60. Lee SG, Lee H, Jeong SH, Yong D, Chung GT, Lee YS, et al. Various penA mutations together with mtrR, porB and ponA mutations in Neisseria gonorrhoeae isolates with reduced susceptibility to cefixime or ceftriaxone. J Antimicrob Chemother. 2010. 65:669–675.

61. Ochiai S, Sekiguchi S, Hayashi A, Shimadzu M, Ishiko H, Matsushima-Nishiwaki R, et al. Decreased affinity of mosaic-structure recombinant penicillin-binding protein 2 for oral cephalosporins in Neisseria gonorrhoeae. J Antimicrob Chemother. 2007. 60:54–60.

62. Takahata S, Senju N, Osaki Y, Yoshida T, Ida T. Amino acid substitutions in mosaic penicillin-binding protein 2 associated with reduced susceptibility to cefixime in clinical isolates of Neisseria gonorrhoeae. Antimicrob Agents Chemother. 2006. 50:3638–3645.

63. Whiley DM, Limnios EA, Ray S, Sloots TP, Tapsall JW. Diversity of penA alterations and subtypes in Neisseria gonorrhoeae strains from Sydney, Australia, that are less susceptible to ceftriaxone. Antimicrob Agents Chemother. 2007. 51:3111–3116.

64. Shafer WM, Folster JP. Towards an understanding of chromosomally mediated penicillin resistance in Neisseria gonorrhoeae: evidence for a porin-efflux pump collaboration. J Bacteriol. 2006. 188:2297–2299.

65. Ropp PA, Hu M, Olesky M, Nicholas RA. Mutations in ponA, the gene encoding penicillin-binding protein 1, and a novel locus, penC, are required for high-level chromosomally mediated penicillin resistance in Neisseria gonorrhoeae. Antimicrob Agents Chemother. 2002. 46:769–777.

66. Lindberg R, Fredlund H, Nicholas R, Unemo M. Neisseria gonorrhoeae isolates with reduced susceptibility to cefixime and ceftriaxone: association with genetic polymorphisms in penA, mtrR, porBIb and ponA. Antimicrob Agents Chemother. 2007. 51:2117–2122.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download