1. Cameron E, Pauling L, Leibovitz B. Ascorbic acid and cancer: a review. Cancer Res. 1979; 39:663–681. PMID:
371790.
2. Golde DW. Vitamin C in cancer. Integr Cancer Ther. 2003; 2:158–159. PMID:
15035904.

3. Cameron E, Pauling L. Supplemental ascorbate in the supportive treatment of cancer: reevaluation of prolongation of survival times in terminal human cancer. Proc Natl Acad Sci U S A. 1978; 75:4538–4542. PMID:
279931.

4. Padayatty SJ, Levine M. Reevaluation of ascorbate in cancer treatment: emerqing evidence, open minds and serendipity. J Am Coll Nutr. 2000; 19:423–425. PMID:
10963459.
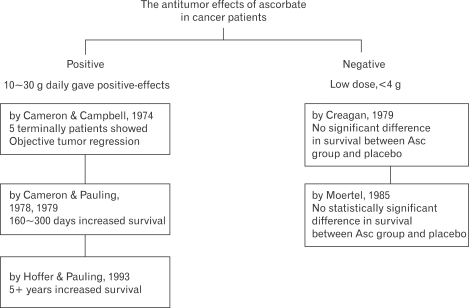
5. Creagan ET, Moertel CG, O'Fallon JR, Schutt AJ, O'Connell MJ, Rubin J, Frytak S. Failure of high-dose vitamin C (ascorbic acid) therapy to benefit patients with advanced cancer. A controlled trial. N Engl J Med. 1979; 301:687–690. PMID:
384241.
6. Moertel CG, Fleming TR, Creagan ET, Rubin J, O'Connell MJ, Ames MM. High-dose vitamin C versus placebo in the treatment of patients with advanced cancer who have had no prior chemotherapy. A randomized double-blind comparison. N Engl J Med. 1985; 312:137–141. PMID:
3880867.
7. Wittes RE. Vitamin C and cancer. N Engl J Med. 1985; 312:178–179. PMID:
3965937.

8. McCormick WJ. Cancer: the preconditioning factor in pathogenesis; a new etiologic approach. Arch Pediatr. 1954; 71:313–322. PMID:
13208373.
9. McCormick WJ. Cancer: a collagen disease, secondary to a nutritional deficiency. Arch Pediatr. 1959; 76:166–171. PMID:
13638066.
10. Cameron E, Rotman D. Ascorbic acid, cell proliferation, and cancer. Lancet. 1972; 1:542. PMID:
4110043.

11. Cameron E, Pauling L. Ascorbic acid and the glycosaminoglycans. An orthomolecular approach to cancer and other diseases. Oncology. 1973; 27:181–192. PMID:
4267127.
12. Cameron E, Campbell A. The orthomolecular treatment of cancer, II: clinical trial of high-dose ascorbic acid supplements in advanced human cancer. Chem Biol Interact. 1974; 9:285–315. PMID:
4430016.

13. Cameron E, Pauling L. Supplemental ascorbate in the supportive treatment of cancer: prolongation of survival times in terminal human cancer. Proc Natl Acad Sci U S A. 1976; 73:3685–3689. PMID:
1068480.

14. Head KA. Ascobic acid in the prevention and treatment of cancer. Altern Med Rev. 1998; 3:174–186. PMID:
9630735.
15. Cameron E, Campbell A. Innovation vs. quality control: an 'unpublishable' clinical trial of supplemental ascorbate in incurable cancer. Med Hypotheses. 1991; 36:185–189. PMID:
1787807.

16. Graumlich JF, Ludden TM, Conry-Cantilena C, Cantilena LR Jr, Wang Y, Levine M. Pharmacokinetics model of ascorbic acid in healthy male volunteers during depletion and repletion. Pharm Res. 1997; 14:1133–1139. PMID:
9327438.
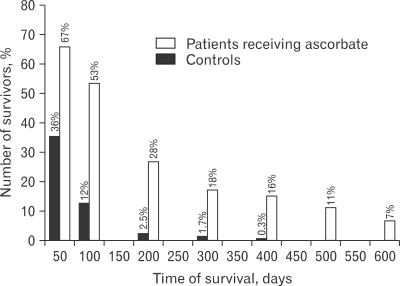
17. Satoshi O, Yumiko O, Nobutaka S, Gen-Ichiro S, Masaki I. High-dose vitamin C (Ascorbic acid) therapy in the treatment of patient with advanced cancer. Anticancer Res. 2009; 29:809–816. PMID:
19414313.
18. Keith I, Block MD, Mark N, Mead MS. Vitamin C in alternative cancer treatment: Historical background. Integrative Cancer Therapies. 2003; 2:147–154. PMID:
15035902.
19. González MJ, Miranda-Massari JR, Mora EM, Guzmán A, Riordan NH, Riordan HD, Casciari JJ, Jackson JA, Ráman-Franco A. Orthomolecular oncology review: ascorbic acid and cancer 25 years later. Interg cancer therapies. 2005; 4:32–44.

20. Levine M. New concepts in the biology and biochemistry of ascorbic acid. N Engl J Med. 1986; 314:892–902. PMID:
3513016.

21. Block G. Vitamin C and cancer prevention: the epidemiologic evidence. Am J Clin Nutr. 1991; 53:s270–s282.

22. Rebouche CJ. Ascorbic acid and carnitine biosynthesis. Am J Clin Nutr. 1991; 54:s1147–s1152.

23. Englard S, Seifter S. The biochemical functions of ascorbic acid. Annu Rev Nutr. 1986; 6:365–406. PMID:
3015170.

24. Sies H, Stahl W, Sundquist AR. Antioxidant functions of vitamins. Vitamins E and C, beta-carotene and other carotenioids. Ann N Y Acad Sci. 1992; 669:7–20. PMID:
1444060.
25. Niki E. Action of ascorbic acid as a scavenger of active and stable oxygen radicals. Am J Clin Nutr. 1991; 54:1119–1124.

26. Frei B, England L, Ames B. Ascorbate is an outstanding antioxidant in human blood plasma. Proc Natl Acad Sci U S A. 1989; 86:6377–6381. PMID:
2762330.

27. Ramp WK, Thorton PA. The effects of ascorbic acid on the glycolytic and respiratory metabolism of embryonic chick tibias. Calcif Tissue Res. 1968; 2:77–82. PMID:
5674916.
28. Mikino Y, Sakagami H, Takeda M. Induction of cell death by ascorbic acid derivatives in human renal carcinoma and glioblastoma cell lines. Anticancer Res. 1999; 19:3125–3132. PMID:
10652601.
29. Poydock ME, Reikert D, Rice J, Aleandri L. Inhibiting effect of dehydroascorbic acid on cell division in ascites tumors in mice. Exp Cell Biol. 1982; 50:34–38. PMID:
7060819.

30. Tomita Y, Eto M, Lio M. Antitumor potency of 3-methyl-3,4-dihydroxytetrone. Sci Bull Fac Agr Kyushu Univ. 1974; 28:131–137.
31. Gonzalez MJ, Mora E, Riordan NH, Riordan HD, Mojica P. Rethinking vitamin C and cancer: an uptake on nutritional oncology. Cancer Prev Int. 1998; 3:215–224.
32. Jampel HD. Ascorbic acid is cytotoxic to dividing human Tenon's capsule fibroblasts. A possible contributing factor in glaucoma filtration surgery success. Arch Ophthalmol. 1990; 108:1323–1325. PMID:
2095758.
33. Tsao CS, Dunhan WB, Leung PY.
In vivo antineoplastic activity of ascorbic acid for human mammary tumor. In vivo. 1988; 2:147–150. PMID:
2979831.
34. Tsao CS, Dunhan WB, Leung PY. Effect of ascorbic acid and its derivatives on the growth of human mammary tumor xenografts in mice. Cancer J. 1989; 5:53–59.
35. Bram S, Froussard P, Guichard M, Jasmin C, Augery Y, Sinoussi-Barre F, Wray W. Vitamin C preferential toxicity for malignant melanoma cells. Nature. 1980; 284:629–631. PMID:
7366735.

36. Sies H, Stahl W. Vitamin E and C, beta-carotene, and other carotenoids as antioxidants. Am J Clin Nutr. 1995; 62:1315–1321.
37. Hemila H. Vitamin C and the common cold. Br J Nutr. 1992; 67:3–16. PMID:
1547201.

38. Jeng KC, Yang CS, Siu WY, Tsai YS, Liao WJ, Kuo JS. Supplementation with vitamin C and E enhances cytokine production by peripheral blood mononuclear cells in heathly adults. Am J Clin Nutr. 1996; 64:960–965. PMID:
8942423.
39. Cho D, Hahm E, Kang JS, Kim YI, Yang YH, Park JH, Kim D, Kim S, Kim YS, Hur D, Park H, Pang S, Hwang YI, Lee WJ. Vitamin C downregulates interleukin-18 production by increasing reactive oxygen intermediate and mitogen-activated protein kinase signaling in B16F10 murine melanoma cells. Melano Res. 2003; 13:549–554.
40. Okamura H, Tsutsi H, Komatsu T, Yutsudo M, Hakura A, Tanimoto T, Torigoe K, Okura T, Nukada Y, Hattori K, et al. Cloning of a new cytokine that induces IFN-gamma production by T cells. Nature. 1995; 378:88–91. PMID:
7477296.
41. Park HU, Byun DG, Kim TG, Kim YI, Kang JS, Hahm ES, Lee WJ. Enhanced IL-18 expression in common skin tumors. Immunol Lett. 2001; 79:215–219. PMID:
11600201.

42. Kim KE, Song H, Kim TS, Yoon D, Kim CW, Bang SI, Hur DY, Park H, Cho DH. Interleukin-18 is a critical factor for vascular endothelial growth factor-enhanced migration in human gastric cancer cell lines. Oncogene. 2007; 26:1468–1476. PMID:
17001321.

43. Park S, Yoon SY, Kim KE, Lee HR, Hur DY, Song H, Kim D, Bang SI, Cho DH. Interleukin-18 induces transferrin expression in breast cancer cell line MCF-7. Cancer Lett. 2009; 6. 15.

44. Park S, Cheon S, Cho D. The dual effects of interleukin-18 in tumor progression. Cell & Mol Immunol. 2007; 4:329–335. PMID:
17976312.
45. Vera JC, Rivas CI, Fischbarg J, Golde DW. Mammalian facilitative hexose transports mediate the transport of dehydroascorbic acid. Nature. 1993; 364:79–82. PMID:
8316303.
46. Vera JC, Rivas CI, Zhang RH, Farber CM, Golde DW. Human HL-60 myeloid leukemia cells transport dehydroascorbic acid via the glucose transporters and accumulate reduced ascorbic acid. Blood. 1994; 84:1628–1634. PMID:
8068952.

47. Guaiquil VH, Farber CM, Golde DW, Vera JC. Efficient transport and accumulation of vitamin C in HL-60 cells depleted of glutathione. J Biol Chem. 1997; 272:9915–9921. PMID:
9092530.

48. Guaiquil VH, Vera JC, Golde DW. Mechanism of vitamin C inhibition of cell death induced by oxidative stress in glutathione- depleted HL-60 cells. J Biol Chem. 2001; 276:40955–40961. PMID:
11533037.
49. Galleano M, Aimo L, Puntarulo S. Ascorbyl radical/ascorbate ratio in plasma from iron overloaded rats as oxidative stress indicator. Toxical Lett. 2002; 133:193–201.

50. Heaney ML, Gardner JR, Karasavvas N, Golde DW, Scheinberg DA, Smith EA, O'Connor OA. Vitamin C antagonizes the cytotoxic effects of antineoplastic drugs. Cancer Res. 2008; 68:8031–8038. PMID:
18829561.

51. Lee SH, Oe T, Blair IA. Vitamin C-induced decomposition of lipid hydroperoxides to endogenous genotoxins. Science. 2001; 292:2083–2086. PMID:
11408659.

52. Lee KW, Lee HJ, Surh YJ, Lee CY. Vitamin C and cancer chemoprevention: reappraisal. Am J Clin Nutr. 2003; 78:1074–1078. PMID:
14668266.

53. Levine M, Wang Y, Padayatty SJ, Morrow J. A new recommended dietary allowance of vitamin C for healthy young women. Proc Natl Acad Sci U S A. 2001; 98:9842–9846. PMID:
11504949.

54. Hahm E, Jin DH, Kang JS, Kim YI, Hong SW, Lee SK, Kim HN, Jung da J, Kim JE, Shin DH, Hwang YI, Kim YS, Hur DY, Yang Y, Cho D, Lee MS, Lee WJ. The molecular mechanisms of vitamin C on cell cycle regulation in B16F10 murine melanoma. J Cell Biochem. 2007; 102:1002–1010. PMID:
17455238.

55. Kang JS, Cho D, Kim YI, Hahm E, Yang Y, Kim D, Hur D, Park H, Bang S, Hwang YI, Lee WJ. L-ascorbic acid (vitamin C) induces the apoptotic of B16 murine melanoma cells via a caspase-8-independent pathway. Cancer Immunol Immunother. 2003; 52:693–698. PMID:
12827307.
56. Kim JE, Jin DH, Lee SD, Hong SW, Shin JS, Lee SK, Jun DJ, Kang JS, Lee WJ. Vitamin C inhibits p53-induced replicative senescence through suppression of ROS production and p38 MAPK activity. Int J Mol Med. 2008; 22:651–655. PMID:
18949386.

57. Lee SK, Kang JS, Jung da J, Hur DY, Kim JE, Hahm E, Bae S, Kim HW, Kim D, Cho BJ, Cho D, Shin DH, Hwang YI, Lee WJ. Vitamin C suppresses proliferation of the human melanoma cell SK-MEL-2 through the inhibition of cyclooxygenase (COX-2) expression and the modulation of insulin- like growth factor (IGF-II) production. J Cell Physiol. 2008; 216:180–188. PMID:
18297687.
58. Ashino H, Shimamura M, NaKajima H, Dombou M, Kawanaka S, Oikawa T, Iwaguchi T, Kawashima S. Novel function of ascorbic acid as an angiostatic factor. Angiogenesis. 2003; 6:259–269. PMID:
15166494.

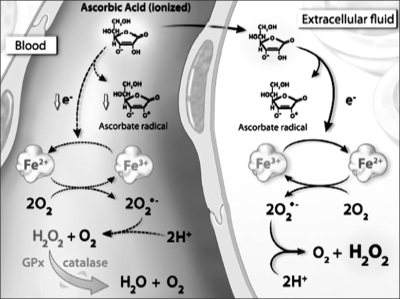
59. Chen Q, Espey MG, Sun AY, Pooput C, Kirk KL, Krishna MC, Khosh DB, Drisko J, Levine M. Pharmacologic doses of ascorbate act as a prooxidant and decrease growth of aggressive tumor xenografts in mice. Proc Natl Acad Sci U S A. 2008; 105:11105–11109. PMID:
18678913.

60. Chen Q, Espey MG, Sun AY, Lee JH, Krishna MC, Shacter E, Choyke PL, Pooput C, Kirk KL, Buettner GR, Levine M. Ascorbate in pharmacologic concentrations selectively generates ascorbate radical and hydrogen peroxide in extracellular fluid
In vivo. Proc Natl Acad Sci U S A. 2007; 104:8749–8754. PMID:
17502596.
61. White JD. Complementary and alternative medicine research: a National Cancer institue perspective. Semin Oncol. 2002; 29:546–551. PMID:
12516037.
62. Nahin RL. Use of the best case series to evaluate complementary and alternative therapies for cancer: a systematic review. Semin Oncol. 2002; 29:552–562. PMID:
12516038.

63. Padayatty SJ, Riordan HD, Hewitt SM, Katz A, Hoffer LJ, Levine M. Intravenously administered vitamin C as cancer therapy: three cases. CMAJ. 2006; 174:937–942. PMID:
16567755.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download