Abstract
The female reproductive tract has two main functions: protection against microbial challenge and maintenance of pregnancy to term. The upper reproductive tract comprises the fallopian tubes and the uterus, including the endocervix, and the lower tract consists of the ectocervix and the vagina. Immune cells residing in the reproductive tract play contradictory roles: they maintain immunity against vaginal pathogens in the lower tract and establish immune tolerance for sperm and an embryo/fetus in the upper tract. The immune system is significantly influenced by sex steroid hormones, although leukocytes in the reproductive tract lack receptors for estrogen and progesterone. The leukocytes in the reproductive tract are distributed in either an aggregated or a dispersed form in the epithelial layer, lamina propria, and stroma. Even though immune cells are differentially distributed in each organ of the reproductive tract, the predominant immune cells are T cells, macrophages/dendritic cells, natural killer (NK) cells, neutrophils, and mast cells. B cells are rare in the female reproductive tract. NK cells in the endometrium significantly expand in the late secretory phase and further increase their number during early pregnancy. It is evident that NK cells and regulatory T (Treg) cells are extremely important in decidual angiogenesis, trophoblast migration, and immune tolerance during pregnancy. Dysregulation of endometrial/decidual immune cells is strongly related to infertility, miscarriage, and other obstetric complications. Understanding the immune system of the female reproductive tract will significantly contribute to women's health and to success in pregnancy.
The female reproductive tract comprises the fallopian tubes, the uterus, and the vagina. This system has several functions, including transportation of gametes and embryo, outflow of the uterine and vaginal secretions (e.g., menstrual blood), service as a birth canal, and protection against microbial challenge.
It is a unique system that is able to balance mucosal immunity against microbes and immune tolerance against sperms and the embryo(s) and fetus(es). The mucosa of the female reproductive tract differs between the upper and the lower tracts. While the upper female reproductive tract includes the uterine tubes, the uterus, and the endocervix, and is covered by a single-layered columnar epithelium, the lower reproductive tract includes the ectocervix and the vagina and is lined with a single layer of stratified, squamous, non-keratinized epithelium, which forms a more protective barrier than the columnar epithelium (1).
The female reproductive tract is highly sensitive to sex steroid hormones and has the potential for rapid proliferation and differentiation of cells during the menstrual cycle. We have reported that lymphocytes in the peripheral blood fluctuated during the menstrual cycle, and that the proportion and cytotoxicity of natural killer (NK) cells increased in the secretory phase (2). In addition to lymphocytes in the peripheral blood, leukocytes in the female reproductive tract fluctuate cyclically through the menstrual cycle, probably as an indirect response to estrogen and progesterone (3).
In the past few decades, many investigators have focused on cyclic changes of uterine endometrial tissues and their immune cells. However, recently, investigation of other reproductive tissues such as the cervix and vagina has become easier with methodological improvements in tissue dispersal (4), and the characteristics of the immune system and the role of each immune cell in the female reproductive tract are still under investigation. New subclasses of immune cells have been introduced, and their functions are being identified via new analytic technologies.
Understanding the immune system of the female reproductive tract is extremely important in the management of sexually transmitted infections, including human immunodeficiency virus (HIV) infection, and in the improvement of fertility and pregnancy outcomes. Herein, we review the updated knowledge and discuss the clinical significance of the immune system in the female reproductive tract.
There are inconsistent reports in terms of the leukocyte population in the female reproductive tract. This discrepancy comes from the differences in the sampling phase in the menstrual cycle, the sample size, the analytic methods, and the antibodies used to determine immune cells. In addition, some types of immune cells, such as dendritic cells (DCs), Treg, and Th17 cells have barely been explored, and new subclasses of immune cells are still emerging. Although there are these limitations, we have summarized the representative data available to date.
CD3+ T cells are distributed throughout the lamina propria of the cervix and vagina as dispersed single cells and as aggregates (5). Unlike CD3+ T cells in the peripheral blood, CD3+ T cells in the female reproductive tract consist of more CD8+ and less CD4+ T cells. Lymphocyte aggregates have frequently been found in the cervix: CD19+CD20+ B cells form follicle-like structures that are surrounded by numerous T cells. These B cells are found only in these lymphoid aggregates of the cervix. Immunoglobulin-producing CD38+ cells, probably plasma cells, were scattered in the lamina propria of the cervix and vagina. In contrast to B cells, these CD38+ cells did not closely localize with CD3+ T cells (5). Neutrophils comprised about 10% of CD45+ cells in the cervix (1) (Fig. 1).
For a more precise review, the vagina was classified into two parts: the upper vagina close to the cervix and the lower vagina close to the vaginal introitus. The lower vagina contains a high concentration of CD8+ T cells in the lamina propria. In contrast, very few CD4+ T cells were found in the lamina propria. A small number of CD68+ macrophages and a low concentration of HLA-DR+ DC-like cells were detected in the lamina propria and epithelium (6). The upper vagina showed a similar pattern of immune cell distribution as in the lower vagina (6). In the upper vagina, CD8+ cells were the major leukocytes and CD1a+ immature DCs followed in number. The majority of CD8+ and CD4+ T cells were detected within the lamina propria, but these cells were also found in the epithelial layer in some samples (6). Thus, CD8+ cell aggregates were frequently found in the vaginal epithelium surrounding the papilla. CD45RO expression was detected on most T cells, but a small portion of CD45RA+ naïve lymphocytes were also found in the lamina propria (6). The concentration of CD68+ macrophages varied substantially from person to person, with most samples showing a low concentration in the lamina propria and a few of these cells in the epithelium (6).
The cervix can be divided into the endocervix and the ectocervix. The endocervix contains mucus-producing glands, which contribute to the prevention of ascending infections by microbial pathogens. Because of this protection, the endocervical cells seldom have contact with pathogens. On the other hand, the ectocervix is exposed to microorganisms, including probiotics, commensal flora, and pathogens. Thus, these two cervices have significant differences in their immune cell distributions. Among CD45+ mononuclear cells in the ectocervix, CD3+ T cells were predominant at 35%, followed by CD14+ cells, and of the CD3+ cells, 40% were CD4+ and 60% were CD8+ (1). About 70% of CD4+ T cells in the ectocervix were effector/memory (CD27-CD45RA-) or effector T cells (CD27-CD45RA+). The majority of CD8+ T cells were CD45RA+CD27-, the effector cell phenotype. CD3-CD56+ NK cells were 2.7% of the CD45+ cells (CD3-CD56brightCD16- NK, 1.7%, and CD3-CD56dimCD16+ NK cells, 1%). CD19+ B cells were only 0.9% of total immune cells. CD4+ T and CD1a+ immature DCs were significantly more abundant in the ectocervix than in the vagina (1).
Antigen-presenting cells (APCs), CD14+ and lymphocyte lineage (CD3, CD20, CD56, and CD16) negative, were the major immune cells in the cervix, ranging 37~55% of CD45+ mononuclear cells (1). CD11c- macrophages were the dominant cells at approximately 30% of CD14+ cells in the cervix. CD14+CD11c+ cells were the second major APCs at about one-third of CD14+ cells. CD11c+HLA-DR+ myeloid DCs (mDCs) and CD123+HLA-DR+ plasmacytoid DCs (pDCs) were each about 1% of cervical CD45+ cells. The cervical DCs were slightly more prevalent than peripheral blood DCs, which were less than 1% of CD45+ cells. DC-SIGN+ cells mostly expressed CD14 molecules, and were preferentially localized in the stroma of both the endocervix and ectocervix (1).
Comparing immune cells in the endocervix and ectocervix, the CD3+ cell population was twice as large in the ectocervix (median of 36%) as in the endocervix (median of 17%) (1). Both CD4+ and CD8+ T cells were more prevalent in the ectocervix. B cells in the ectocervix were twice as abundant as in the endocervix, with median values of 0.9% and 0.4%, respectively. NK cell subsets of CD56brightCD16- and CD56dimCD16+ were not significantly different between the endocervix and ectocervix, with each NK cell subset ranging 1~2% of CD45+ cells in either cervix (1). IL-22 producing NK cells (NK22 cells), known to play an important role in mucosal immunity, were detected very rarely in the cervix (medians of 0.2% and 0.1% of CD3- cells in the endocervix and ectocervix, respectively) (1).
The endometrium is the most abundant cellular tissue in the female reproductive tract. The number of leukocytes per gram of endometrial tissue is greater than that of other reproductive tissues, such as those in the fallopian tube, endocervix, ectocervix, and vagina.
Endometrial lymphoid aggregates comprised a CD19+ B cell core, surrounding T cells, and an outer halo of macrophages in the stratum basalis (3,7). These lymphocyte aggregates varied in size with the phase of the menstrual cycle, becoming larger in the secretory phase (3,000~4,000 cells) than the proliferative phase (300~400 cells) (3). To form lymphoid aggregates, immune cell trafficking to nucleation sites is likely to be the principle mechanism, rather than in situ proliferation of precursor cells (8).
There are several hypotheses regarding the origins of endometrial leukocytes. One hypothesis was that leukocytes are brought in with the circulating blood into the endometrium. Circulating leukocytes are recruited to the endometrium following evasion of endothelial cells expressing adhesion molecules that serve as ligands for homing receptors of immune cells (5). Another hypothesis was that there is in situ proliferation of resident immune cells (9,10). Yet another was that hematopoietic precursors are recruited and differentiated within the endometrium (11,12). Recruited immune cells from the circulation are likely to undergo tissue-specific differentiation in the local microenvironment, which confers new characteristics on these tissue-specific cells that are distinct from their original properties (7,11).
CD3+ T cells are a minor population in the endometrium, comprising only 1~2% of the total lymphomyeloid cells (13). These T cells are distributed in three different sites of the endometrium: aggregated in the basal lymphoid, and scattered in the stroma, and in the epithelial sites (14). In contrast with CD3+ T cells in peripheral blood, endometrial CD3+ T cells consisted of a larger proportion of CD8+ cells (66%) and smaller proportion of CD4+ cells (33%) (14). Cytolytic activity of endometrial CD8+ T cells was maintained during the proliferative phase, but this activity weakened in the secretory phase without any drop in the CD8+ cell number (3,14). This suppression of CD8+ cell cytolytic activity was observed only in the fallopian tubes and endometrium, but not in the cervix and vagina (3). CD45RA+ B cells were found throughout the cycle, but their numbers were very low (14).
Uterine NK cells have also been called large granular lymphocytes (LGL), endometrial granulocytes, K cells, endometrial granulated lymphocytes (eGL), and decidual granulated lymphocytes (dGL) (7). The major phenotype of endometrial NK cells is CD3-CD56brightCD16-, which distinguishes this cell subset from CD3-CD56dimCD16+ NK cells in the peripheral blood (7,15). It is possible that peripheral blood CD56bright NK cells home to the uterus where they undergo tissue-specific differentiation.
In the proliferative phase, only a few NK cells are scattered throughout the stroma of the functional layer. In contrast, the NK cells show a dramatic increase in number after ovulation and continue to increase until a few days prior to menstruation. In the late secretory phase, the number of NK cells surges up to 30~40% of cells in the stromal compartment and 70% of endometrial leukocytes (7,15). NK cells, particularly, surround both the arteries and glands of the endometrium. Since there are few NK cells in the endometrium in the menstrual and proliferative phases, an association between falling progesterone and apoptosis of uterine NK cells has been suggested. Considering NK cells and other leukocytes in the uterus do not express progesterone receptors, progesterone might exert its effects indirectly via cytokines or other soluble factors produced by stromal cells. Stromal cells strongly express both estrogen receptors (ERs) and progesterone receptors (PRs). Intriguingly, nuclear morphological features that are similar to apoptotic NK cells are found in decidua from miscarriages, and in the endometria of patients who have discontinued progesterone treatment (7).
CD68+ macrophages are also detected in all phases of the menstrual cycle (14). These macrophages are scattered throughout the endometrium, and are found especially around the glands (16). There is a significant increase in macrophage numbers in the secretory phase, especially prior to menses, and this increase is particularly notable at the implantation site (7,17).
The density of endometrial CD1a+ immature DCs was significantly higher than that of CD83+ mature DCs throughout the menstrual cycle (7). The proportion of CD1a+ and CD83+ DCs was not different between the fundus and isthmus of the uterus.
The major population of leukocytes in the fallopian tube is CD3+ cells, representing approximately 40% of all CD45+ cells (4). CD66b+ granulocytes, including neutrophils, mast cells, and eosinophils, were the second major constituent, making up a quarter of the CD45+ cells. CD14+ cells and CD19+ cells each consisted of about 10% of total leukocytes (4).
Comparing the immune cells between the different reproductive organs, the upper reproductive tract showed a higher proportion of leukocytes and a greater number of leukocytes per gram of tissue than the lower reproductive tract (4). The number of CD3+ T cells of the fallopian tube was significantly higher than that of the ectocervix and the vagina (4). Similarly, the percentage of CD66b+ granulocytes was significantly higher in the fallopian tube than in the endometrium, the endocervix, and the other parts of the lower reproductive tract. In contrast, CD19+ B cells and CD14+ cells showed no difference throughout the reproductive tract (4).
Antimicrobial molecules are another important factor in mucosal immunity and are produced in the mucosa of the female reproductive tract. These secretory molecules are significantly influenced by estrogen, which acts differently in the upper and lower reproductive tracts. High levels of estrogen, a characteristic of the preovulatory period, increase the production of some antimicrobial peptides, such as secretory leukocyte peptidase inhibitor (SLPI), β-defensin 1-2 (HBD 1-2), and elafin from the endometrial epithelium (3) (Fig. 2). On the other hand, estrogen suppresses the LPS- and poly (I:C)-induced secretion of proinflammatory cytokines, including TNF-α, macrophage inflammatory protein 3α (MIP3α, CCL20), IL-1β, IL-6, and IL-8 from uterine epithelial cells. Immunoglobuin (Ig) G levels in the uterine cavity peak in the periovulatory period. In contrast, the lower reproductive tract, including the cervix and the vagina, maintains a low level of IgA, IgG, and lactoferrin and decreased secretions of β-defensin 2, elafin, SLPI, and α-defensin1-3 (HNP1-3). Furthermore, concentrations of IL-6 and IL-8 in the vagina are decreased in the period of highest estrogen concentration (3). This decreased immunity in the lower genital tract may contribute to enhanced sperm survival in the periovulation period. In addition, the estrogen rise in the periovulatory period increases antimicrobial peptides and decreases proinflammatory cytokines in the upper genital tract, which prevents ascending infections by vaginal pathogens and provides favorable conditions for the transit of sperm and embryos.
T cells, APCs, and CD1a+ cells in the vagina and cervix were not significantly different between the follicular and luteal phases of the menstrual cycle (6). However, endometrial leukocytes demonstrated profound cyclic fluctuations (Fig. 3).
The mean number of CD45+ cells in the endometrium remained low from the early follicular phase to the early secretory phase, but robustly increases (about 5-fold) during the secretory phase as compared with all other phases (18). As a result, the total number of leukocytes peaked in the premenstrual period corresponding to the late secretory phase (14). The major population of CD45+ leukocytes in the late secretory phase was NK cells comprising approximately 80% of CD45+ cells, while CD3+ T cells decreased to less than 10% (18). Even though the percentage of CD3+ T cells was lower in the late secretory phase, the absolute number of T cells remained unchanged during the menstrual cycle. Comparing the late proliferative phase with the late secretory phase, the proportion of CD3+CD8+ T cells of total CD3+ T cells decreased significantly from 63% to 54% (18).
The number of CD3-CD56+ NK cells was significantly increased in the late secretory phase compared with other phases (18). The cytotoxicity of endometrial NK cells is high and comparable with that of peripheral blood NK cells in the late proliferative phase (19). Similarly, the expression of the activation markers CD69 and HLA-DR were increased on NK cells in the proliferative phase (20). These characteristics of NK cells are likely to contribute to protective immunity against microbial infections. However NK cell cytotoxicity decreased during the secretory phase, which suggests that local functional regulation works in the secretory phase.
During the menstrual cycle, neutrophils and eosinophils remain at very low concentrations in the endometrium, but their numbers profoundly increase in the premenstrual period, up to 6~15% and 3~5% of endometrial cells, respectively (13,14). Mast cells were identified in the endometrium throughout the menstrual cycle, but did not fluctuate greatly throughout the cycle (21). However, the activation of mast cells was most significant just prior to menstruation (21).
CD68+ macrophages were found throughout the cycle and significantly increased from the proliferative phase to the secretory phase (22). The density of endometrial CD1a+ DCs, but not CD83+ DCs, in the basal layer gradually increased through the menstrual cycle, showing a nadir at the proliferative phase and reaching its peak in the menstrual phase (23). Only in the secretory phase was the density of CD1a+ DCs greater in the basal layer than in the functional layer. Endometrial CD83+ DCs showed greater density in the basal layer than in the functional layer throughout the menstrual cycle (23).
In the pregnant uterus, some immune cells play an important role in immune tolerance, providing for the acceptance of a semi-allogeneic fetus. The principle cells involved are NK cells and Treg cells.
NK cells are the major leukocytes in the decidua. The number of decidual NK cells continues to increase until the end of the first trimester and then decreases near term (15). Decidual NK cells contribute to pregnancy by increasing the blood flow at the fetomaternal interface and helping the migration of the trophoblast. The main role of NK cells in pregnancy is the secretion of angiogenic factors such as VEGF and angiopoietin-2, as well as cytokines and growth factors such as TNF-α, IL-10, GM-CSF, placental growth factor (PlGF), IL-1β, TGF-β1, CSF-1, LIF, and IFN-γ (15).
Treg cells are considered key players in immune regulation during pregnancy. While it is known that CD4+CD25bright T cells of peripheral blood increase from early pregnancy until the second trimester, there is little data in terms of the proportional change of endometrial and decidual Treg cells (24). One study demonstrated that the percentage of decidual Treg cells peaked in the second trimester just like Treg cells in the peripheral blood (25). However, another study did not find any change in the number of Treg cells of human decidua basalis during pregnancy, but found that there was a greater number of Treg cells in the decidua parietalis in the third trimester relative to the second trimester (26). The proportion of decidual Treg cells, defined as CD4+CD25bright cells, was significantly higher than that of Treg cells in the peripheral blood in the first trimester (27). Tilburgs et al. reported that maternal blood and decidual CD4+CD25bright Treg cells were functionally active, and that fetus-specific Treg cells were selectively recruited from peripheral blood into the decidua (26). Another Treg cell study performed in early human pregnancy showed that decidual Foxp3+ Treg cells expressed Ki67 more highly than peripheral blood Treg cells, perhaps explaining the mechanism of Treg cell enrichment in the decidua during pregnancy (28).
Similar to Treg cells, Th17 cells are preferentially recruited to the decidua during pregnancy. As a result, the proportion of Th17 cells in the decidua is higher than that of the peripheral blood in normal pregnancy (29). During pregnancy, macrophages and DCs are likely to support fetal acceptance in the uterus. In a comparison between decidual and peripheral monocytes/macrophages in early human pregnancy, the number of IL-10 secreting cells was significantly higher in decidual macrophages than in peripheral blood monocytes (30). This indicates that decidual macrophages play a role in immune regulation in the early pregnant uterus. In decidua of early pregnancy in humans, Th2-promoting DCs were predominant. Even though the percentage of DCs, relative to mononuclear cells (leukocytes), in the early pregnancy decidua was significantly higher than that of the peripheral blood, the number of IL-12 producing the total and the myeloid DCs of the decidua was significantly lower than that in the peripheral blood (31).
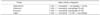
Just as the proportion of immune cells in the peripheral blood changes following menopause, some differences in the immune cells of the female reproductive tract in postmenopausal vs. premenopausal women are also apparent (Table I).
In the endometrium, the number of CD45+ cells per gram of tissue was profoundly decreased in postmenopausal women as compared with that of the proliferative phase in premenopausal women (4). Similarly, the percentage of leukocytes in the endocervix was decreased in the postmenopausal period as compared with that in the premenopausal period (4). Comparing the immune cells between the endocervix and ectocervix, both CD4+ and CD8+ T cells were found to be significantly more abundant in the ectocervix than in the endocervix during the reproductive period (1). However, in postmenopausal women, only the number of CD4+ T cells was higher in the ectocervix; the number of CD8+ cells was not. Therefore, the ratio of CD4+:CD8+ cells in the ectocervix increases in the postmenopausal period (1). CD56dimCD16+ NK cells in the endocervix are less relevant in postmenopausal period than in the reproductive period (1).
However, most immune cells, including CD4+ T, CD8+ T, CD19+ B, and CD56brightCD16- NK cells are not changed in their proportions of total CD45+ cells between premenopausal and postmenopausal cervical tissues (1). Furthermore, APCs and CD1a+ DCs were also found in similar proportions between premenopausal and postmenopausal periods (6).
The clinical significance of uterine leukocytes has been well-documented in reproductive medicine literature, along with the role of immune cells in the peripheral blood.
Treg cells are the most important immune component in immune tolerance of pregnancy, as well as autoimmune diseases and chronic inflammation. Insufficiency and/or functional defects of Treg cells in the decidua have been reported as a pathophysiology of obstetric complications, such as recurrent pregnancy loss, preterm births, and preeclampsia (27,32,33). Conversely, decidual Treg cells were more abundant in women with placenta accreta than in women with healthy pregnancies (34). Th17 cells, one type of effector T cells, have been proposed to be involved in spontaneous abortions, preeclampsia, and preterm labor (35,36,37,38). Furthermore, an imbalance in the Th17/Treg cell ratio in the peripheral blood and/or decidua has been found to be associated with the poor obstetric outcomes mentioned previously (39).
It is evident that abnormalities in the proportion and activity of decidual NK cells are related to poor pregnancy outcomes. Higher decidual NK cell cytotoxicity was observed in cases of spontaneous abortion and recurrent pregnancy loss (38,40). Women with recurrent pregnancy loss showed increased proportions of secretory endometrial NK cells (41,42), and increased expression of CD94 and CD158 on endometrial NK cells was demonstrated in infertility patients (43). A decreased percentage of CD56+ decidual NK cells and low level of CD56+ endometrial NK cells were shown in women with recurrent pregnancy loss and in women with polycystic ovarian syndrome, respectively (44,45). An imbalance in NK cell activation and inhibitory receptors may also be involved in obstetric complications. Women who spontaneously aborted in their index pregnancies had increased expression of NKp46 and NKp44 or lacked the appropriate inhibitory receptors on decidual NK cells (46,47).
Some APCs of the uterus have been studied in obstetric diseases. Fewer decidual CD209+ immature DCs were found in women with placenta accreta than in women with healthy pregnancies (34). Women experiencing preterm preeclampsia showed CD14+CD163+ macrophages more frequently in the decidua compared with preterm control women (48). These findings suggest that decidual APCs may play a role in regulation of trophoblast invasion and differentiation.
The female reproductive tract is crucial for the establishment and maintenance of pregnancy as well as protective immunity from microbial challenge. During pregnancy, the upper reproductive tract harbors the key organs to accept and nourish a fetus through immune tolerance and angiogenesis. The lower reproductive tract is essential for both pregnant and non-pregnant women to prevent ascending infection by pathogenic micro-organisms. These contradictory immune responses are working simultaneously, and their distinct functions are especially prominent during pregnancy.
It is well known that the cervix and vagina encounter commensal bacteria and prevent them from invading the endometrium, even though micro-organisms multiply in the vaginal mucosa. There has been a belief that the placenta in normal pregnancy is sterile, but placentas harboring microorganisms in healthy pregnancies were recently shown in a whole-genome shotgun metagenomic study (49). Further studies are needed to elucidate the mechanisms underlying how the pregnant uterus and placenta control microbes during pregnancy without negative impacts on the fetus.
Estrogen has been suggested as one of the key regulators of immune cells in the female reproductive tract. However, the changes in endometrial leukocytes are not significant in the late proliferative period, so estrogen seems to contribute little to recruitment or proliferation of endometrial immune cells. On the other hand, progesterone has also been considered a dominant regulator, since the greatest increase in endometrial immune cells are noted in the late secretory phase when the level of progesterone falls (17). This progesterone effect on immune cells is less likely to be mediated by PR, because uterine CD45+ leukocytes do not express ER and PR (14). Sex steroid hormones seem to control uterine leukocytes indirectly. Uterine immune cells have crosstalk with endometrial epithelial and stromal cells, which are tightly controlled by estrogen and progesterone. Considering the structural similarity between progesterone and glucocorticoids, and between PR and glucocorticoid receptor (GR), progesterone may act similarly through PR and GR (14).
It is very intriguing that the characteristics of endometrial/decidual leukocytes are significantly different from those of leukocytes in the peripheral blood. With tissue-specific cell differentiation, the microenvironment of the local tissue is highly important in cyclic alterations of the numbers and phenotypes of immune cells in the endometrium (17). Uterine NK cells and mast cells are involved in the implantation of the embryo in the endometrium, while neutrophils, eosinophils, and mast cells are key players in the initiation of menstruation (17).
Leukocytes, especially in the endometrium and decidua, have been vigorously studied in women with infertility and pregnancy complications. Immune activation or imbalance between immune effectors and regulators has been reported in the patients with reproductive failure. There are several reports demonstrating a strong correlation between immune cells of the endometrium or the decidua and peripheral blood (50,51), although there is a concern that peripheral blood NK cells may not inform what is happening in the uterus (52). Further studies are needed to show the value of using peripheral blood to investigate intrauterine immunity.
This review has some limitations due to a relative lack of data regarding immune cells in the reproductive tract, the recent introductions of new subclasses of immune cells, and the emergence of comprehensive analytic equipment and methods that have yet to answer fundamental questions. Nevertheless, understanding female reproductive organs and their immune cells is very important for women's health and their successful pregnancies. Through such investigation, new immune markers can be introduced as diagnostic tools and prognostic markers. Recently, immunomodulatory treatments using immunoglobulin, glucocorticoids, and anti-TNFα have been applied in women with reproductive failure, based on the findings of immune dysregulation in women with infertility and obstetric complications. We hope to discover new, effective immune therapies to overcome the unsolved issues in reproductive medicine.
In conclusion, investigation of the immune system in the female reproductive tract can solve the puzzle of semi-allograft acceptance during pregnancy and contribute to better women's health and saving life.
Figures and Tables
 | Figure 1Distribution of major leukocytes in the female reproductive tract in premenopausal women. There are some discrepancies in the proportion of each leukocyte population, since several reports have been published using different study designs. Most data represent leukocyte populations in all phases of the menstrual cycle. T, T cells; B, B cells; NK, natural killer cells; Mφ, macrophages; DC, dendritic cells. Data were collected from Givan et al. (4), Salamonsen and Woolley (13), and Trifonova et al. (1). |
 | Figure 2Secretion of antimicrobial molecules in the female reproductive tract in the periovulatory period. High estrogen concentration significantly affects the production of antimicrobial peptides and proinflammatory cytokines which are differentially regulated in the upper and the lower reproductive tracts (3). SLPI, secretory leukocyte peptidase inhibitor. |
 | Figure 3Cyclic fluctuation of endometrial leukocytes during the menstrual cycle. Immune cells in the endometrium are indirectly regulated by ovarian sex steroid hormones. Several leukocytes are significantly increased in the premenstrual phase, but some cells do not fluctuate during the menstrual cycle. The density of leukocyte population is expressed as -, +, ++, and ++ +, which represent 0%, 1~2%, 3~5%, and 6~15% of total numbers of endometrial cells, respectively. Data were collected from Salamonsen and Woolley (13), Flynn et al. (18), and Givan et al. (4). |
Table I
Distribution of major leukocytes in the female reproductive tract in postmenopausal women (4)
ACKNOWLEDGEMENTS
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HI 14C0368).
References
1. Trifonova RT, Lieberman J, van Baarle D. Distribution of immune cells in the human cervix and implications for HIV transmission. Am J Reprod Immunol. 2014; 71:252–264.

2. Lee S, Kim J, Jang B, Hur S, Jung U, Kil K, Na B, Lee M, Choi Y, Fukui A, Gilman-Sachs A, Kwak-Kim JY. Fluctuation of peripheral blood T, B, and NK cells during a menstrual cycle of normal healthy women. J Immunol. 2010; 185:756–762.

3. Wira CR, Fahey JV, Rodriguez-Garcia M, Shen Z, Patel MV. Regulation of mucosal immunity in the female reproductive tract: the role of sex hormones in immune protection against sexually transmitted pathogens. Am J Reprod Immunol. 2014; 72:236–258.

4. Givan AL, White HD, Stern JE, Colby E, Gosselin EJ, Guyre PM, Wira CR. Flow cytometric analysis of leukocytes in the human female reproductive tract: comparison of fallopian tube, uterus, cervix, and vagina. Am J Reprod Immunol. 1997; 38:350–359.

5. Johansson EL, Rudin A, Wassen L, Holmgren J. Distribution of lymphocytes and adhesion molecules in human cervix and vagina. Immunology. 1999; 96:272–277.

6. Pudney J, Quayle AJ, Anderson DJ. Immunological microenvironments in the human vagina and cervix: mediators of cellular immunity are concentrated in the cervical transformation zone. Biol Reprod. 2005; 73:1253–1263.

8. Yeaman GR, Collins JE, Fanger MW, Wira CR, Lydyard PM. CD8+ T cells in human uterine endometrial lymphoid aggregates: evidence for accumulation of cells by trafficking. Immunology. 2001; 102:434–440.

9. van den Heuvel M, Peralta C, Bashar S, Taylor S, Horrocks J, Croy BA. Trafficking of peripheral blood CD56(bright) cells to the decidualizing uterus--new tricks for old dogmas? J Reprod Immunol. 2005; 67:21–34.

10. Kitaya K, Yamaguchi T, Yasuo T, Okubo T, Honjo H. Post-ovulatory rise of endometrial CD16(-) natural killer cells: in situ proliferation of residual cells or selective recruitment from circulating peripheral blood? J Reprod Immunol. 2007; 76:45–53.

11. Keskin DB, Allan DS, Rybalov B, Andzelm MM, Stern JN, Kopcow HD, Koopman LA, Strominger JL. TGFbeta promotes conversion of CD16+ peripheral blood NK cells into CD16- NK cells with similarities to decidual NK cells. Proc Natl Acad Sci U S A. 2007; 104:3378–3383.

12. Manaster I, Mandelboim O. The unique properties of uterine NK cells. Am J Reprod Immunol. 2010; 63:434–444.

13. Salamonsen LA, Woolley DE. Menstruation: induction by matrix metalloproteinases and inflammatory cells. J Reprod Immunol. 1999; 44:1–27.

14. Salamonsen LA, Lathbury LJ. Endometrial leukocytes and menstruation. Hum Reprod Update. 2000; 6:16–27.

15. Lee JY, Lee M, Lee SK. Role of endometrial immune cells in implantation. Clin Exp Reprod Med. 2011; 38:119–125.

16. Song JY, Fraser IS. Effects of progestogens on human endometrium. Obstet Gynecol Surv. 1995; 50:385–394.

17. Salamonsen LA, Zhang J, Brasted M. Leukocyte networks and human endometrial remodelling. J Reprod Immunol. 2002; 57:95–108.

18. Flynn L, Byrne B, Carton J, Kelehan P, O'Herlihy C, O'Farrelly C. Menstrual cycle dependent fluctuations in NK and T-lymphocyte subsets from non-pregnant human endometrium. Am J Reprod Immunol. 2000; 43:209–217.

19. Jones RK, Bulmer JN, Searle RF. Phenotypic and functional studies of leukocytes in human endometrium and endometriosis. Hum Reprod Update. 1998; 4:702–709.

20. Kodama T, Hara T, Okamoto E, Kusunoki Y, Ohama K. Characteristic changes of large granular lymphocytes that strongly express CD56 in endometrium during the menstrual cycle and early pregnancy. Hum Reprod. 1998; 13:1036–1043.

21. Jeziorska M, Salamonsen LA, Woolley DE. Mast cell and eosinophil distribution and activation in human endometrium throughout the menstrual cycle. Biol Reprod. 1995; 53:312–320.

22. Bonatz G, Hansmann ML, Buchholz F, Mettler L, Radzun HJ, Semm K. Macrophage- and lymphocyte-subtypes in the endometrium during different phases of the ovarian cycle. Int J Gynaecol Obstet. 1992; 37:29–36.

23. Schulke L, Manconi F, Markham R, Fraser IS. Endometrial dendritic cell populations during the normal menstrual cycle. Hum Reprod. 2008; 23:1574–1580.

24. Somerset DA, Zheng Y, Kilby MD, Sansom DM, Drayson MT. Normal human pregnancy is associated with an elevation in the immune suppressive CD25+ CD4+ regulatory T-cell subset. Immunology. 2004; 112:38–43.

25. Quinn KH, Lacoursiere DY, Cui L, Bui J, Parast MM. The unique pathophysiology of early-onset severe preeclampsia: role of decidual T regulatory cells. J Reprod Immunol. 2011; 91:76–82.

26. Tilburgs T, Roelen DL, van der Mast BJ, de Groot-Swings GM, Kleijburg C, Scherjon SA, Claas FH. Evidence for a selective migration of fetus-specific CD4+CD25bright regulatory T cells from the peripheral blood to the decidua in human pregnancy. J Immunol. 2008; 180:5737–5745.

27. Sasaki Y, Sakai M, Miyazaki S, Higuma S, Shiozaki A, Saito S. Decidual and peripheral blood CD4+CD25+ regulatory T cells in early pregnancy subjects and spontaneous abortion cases. Mol Hum Reprod. 2004; 10:347–353.

28. Mjosberg J, Berg G, Jenmalm MC, Ernerudh J. FOXP3+ regulatory T cells and T helper 1, T helper 2, and T helper 17 cells in human early pregnancy decidua. Biol Reprod. 2010; 82:698–705.
29. Nakashima A, Ito M, Yoneda S, Shiozaki A, Hidaka T, Saito S. Circulating and decidual Th17 cell levels in healthy pregnancy. Am J Reprod Immunol. 2010; 63:104–109.
30. Lidstrom C, Matthiesen L, Berg G, Sharma S, Ernerudh J, Ekerfelt C. Cytokine secretion patterns of NK cells and macrophages in early human pregnancy decidua and blood: implications for suppressor macrophages in decidua. Am J Reprod Immunol. 2003; 50:444–452.

31. Miyazaki S, Tsuda H, Sakai M, Hori S, Sasaki Y, Futatani T, Miyawaki T, Saito S. Predominance of Th2-promoting dendritic cells in early human pregnancy decidua. J Leukoc Biol. 2003; 74:514–522.

32. Mei S, Tan J, Chen H, Chen Y, Zhang J. Changes of CD4+CD25high regulatory T cells and FOXP3 expression in unexplained recurrent spontaneous abortion patients. Fertil Steril. 2010; 94:2244–2247.

33. Galazka K, Wicherek L, Pitynski K, Kijowski J, Zajac K, Bednarek W, Dutsch-Wicherek M, Rytlewski K, Kalinka J, Basta A, Majka M. Changes in the subpopulation of CD25+ CD4+ and FOXP3+ regulatory T cells in decidua with respect to the progression of labor at term and the lack of analogical changes in the subpopulation of suppressive B7-H4 macrophages--a preliminary report. Am J Reprod Immunol. 2009; 61:136–146.

34. Schwede S, Alfer J, von Rango U. Differences in regulatory T-cell and dendritic cell pattern in decidual tissue of placenta accreta/increta cases. Placenta. 2014; 35:378–385.

35. Lee SK, Kim JY, Hur SE, Kim CJ, Na BJ, Lee M, Gilman-Sachs A, Kwak-Kim J. An imbalance in interleukin-17-producing T and Foxp3+ regulatory T cells in women with idiopathic recurrent pregnancy loss. Hum Reprod. 2011; 26:2964–2971.

36. Toldi G, Rigo J Jr, Stenczer B, Vasarhelyi B, Molvarec A. Increased prevalence of IL-17-producing peripheral blood lymphocytes in pre-eclampsia. Am J Reprod Immunol. 2011; 66:223–229.

37. Ito M, Nakashima A, Hidaka T, Okabe M, Bac ND, Ina S, Yoneda S, Shiozaki A, Sumi S, Tsuneyama K, Nikaido T, Saito S. A role for IL-17 in induction of an inflammation at the fetomaternal interface in preterm labour. J Reprod Immunol. 2010; 84:75–85.

38. Wang WJ, Hao CF, Yi L, Yin GJ, Bao SH, Qiu LH, Lin QD. Increased prevalence of T helper 17 (Th17) cells in peripheral blood and decidua in unexplained recurrent spontaneous abortion patients. J Reprod Immunol. 2010; 84:164–170.

39. Lee SK, Kim JY, Lee M, Gilman-Sachs A, Kwak-Kim J. Th17 and regulatory T cells in women with recurrent pregnancy loss. Am J Reprod Immunol. 2012; 67:311–318.

40. Chao KH, Yang YS, Ho HN, Chen SU, Chen HF, Dai HJ, Huang SC, Gill TJ III. Decidual natural killer cytotoxicity decreased in normal pregnancy but not in anembryonic pregnancy and recurrent spontaneous abortion. Am J Reprod Immunol. 1995; 34:274–280.

41. Clifford K, Flanagan AM, Regan L. Endometrial CD56+ natural killer cells in women with recurrent miscarriage: a histomorphometric study. Hum Reprod. 1999; 14:2727–2730.

42. Tuckerman E, Laird SM, Prakash A, Li TC. Prognostic value of the measurement of uterine natural killer cells in the endometrium of women with recurrent miscarriage. Hum Reprod. 2007; 22:2208–2213.

43. McGrath E, Ryan EJ, Lynch L, Golden-Mason L, Mooney E, Eogan M, O'Herlihy C, O'Farrelly C. Changes in endometrial natural killer cell expression of CD94, CD158a and CD158b are associated with infertility. Am J Reprod Immunol. 2009; 61:265–276.

44. Yamamoto T, Takahashi Y, Kase N, Mori H. Decidual natural killer cells in recurrent spontaneous abortion with normal chromosomal content. Am J Reprod Immunol. 1999; 41:337–342.

45. Matteo M, Serviddio G, Massenzio F, Scillitani G, Castellana L, Picca G, Sanguedolce F, Cignarelli M, Altomare E, Bufo P, Greco P, Liso A. Reduced percentage of natural killer cells associated with impaired cytokine network in the secretory endometrium of infertile women with polycystic ovary syndrome. Fertil Steril. 2010; 94:2222–2227.

46. Zhang Y, Zhao A, Wang X, Shi G, Jin H, Lin Q. Expressions of natural cytotoxicity receptors and NKG2D on decidual natural killer cells in patients having spontaneous abortions. Fertil Steril. 2008; 90:1931–1937.

47. Varla-Leftherioti M, Spyropoulou-Vlachou M, Keramitsoglou T, Papadimitropoulos M, Tsekoura C, Graphou O, Papadopoulou C, Gerondi M, Stavropoulos-Giokas C. Lack of the appropriate natural killer cell inhibitory receptors in women with spontaneous abortion. Hum Immunol. 2005; 66:65–71.

48. Schonkeren D, van der Hoorn P, Khedoe P, Swings G, van Beelen E, Claas F, van Kooten C, de Heer E, Scherjon S. Differential distribution and phenotype of decidual macrophages in preeclamptic versus control pregnancies. Am J Pathol. 2011; 178:709–717.

49. Aagaard K, Ma J, Antony KM, Ganu R, Petrosino J, Versalovic J. The placenta harbors a unique microbiome. Sci Transl Med. 2014; 6:237ra65.

50. Park DW, Lee HJ, Park CW, Hong SR, Kwak-Kim J, Yang KM. Peripheral blood NK cells reflect changes in decidual NK cells in women with recurrent miscarriages. Am J Reprod Immunol. 2010; 63:173–180.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download