Abstract
Dysfunction of gut immune regulation is involved in mucosal damage in inflammatory bowel disease (IBD). However, there is still no efficacious immune-regulator for the treatment of IBD. Alloferon is a novel immune-modulatory peptide that was originally isolated from infected insects. It shows anti-inflammatory effects by the regulation of cytokine production by immune cells and their activities. Therefore, we investigated the effect of alloferon in a mouse model of colitis using dextran sulfate sodium (DSS). Colitis was induced by administration of DSS in drinking water for 7 consecutive days. It was confirmed by the presence of weight loss, diarrhea, hematochezia, and colon contraction. Alloferon was injected 4 days after DSS administration. We found that alloferon improved the pathogenesis of IBD based on the reduced disease activity index (DAI) and colon contraction. Edema, epithelial erosion, and immune cell infiltration were found in mice administered DSS, but the phenomena were reduced following alloferon treatment. The plasma level of IL-6, a classical pro-inflammatory cytokine in colitis, was also decreased by alloferon. Moreover, alloferon inhibited the TNF-α-induced degradation and phosphorylation of IκB in Colo205 colon cancer cells. Taken together, these results show that alloferon has anti-inflammatory effects and attenuates DSS-induced colitis.
Inflammatory bowel disease (IBD) is a term that describes a group of inflammatory conditions of the gastrointestinal tract. This chronic disease is characterized by abdominal pain, vomiting, diarrhea, rectal bleeding, and weight loss. The major forms of idiopathic IBD are Crohn's disease (CD) and ulcerative colitis (UC). UC is characterized by diffused mucosal inflammation with extensive superficial mucosal ulceration. Histopathological features include a significant number of neutrophils in the lamina propria and the crypts as well as the depletion of goblet cells. CD is characterized by the aggregation of macrophages that frequently form non-caseating granulomas. Unlike UC, CD may be patchy, segmental, and typically transmural (12).
The onset of IBD typically occurs in the second and third decades of life and the majority of affected individual progress to relapses and a chronic condition. A rising trend has been reported in the incidence and prevalence of IBD in Asia and it is postulated that this increase may be related to the westernized lifestyle including changes in diet and environment, such as improved sanitation and industrialization (3). During the past two decades in Korea, the mean annual incidence rates of CD and UC increased significantly from 0.05 and 0.34 per 100,000 inhabitants, respectively, in 1986~1990 to 1.34 and 3.08 per 100,000 inhabitants, respectively, in 2001~2005. In addition, the adjusted prevalence rates of CD and UC per 100,000 inhabitants were 11.24 and 30.87, respectively in 2005. Although the incidence and prevalence of CD and UC in Korea are still lower than those in Western countries, they are rapidly increasing (4). The cause of IBD is known to be an inadequate and exaggerated immune response against commensal microbiota, especially in genetically susceptible individuals (15). There is no well-established therapy for IBD and, therefore, the quality of life and expectancy are compromised in patients with IBD.
Alloferon is a bioactive, slightly cationic peptide originally isolated from an experimentally infected blowfly, Calliphora vicina. It consists of 13 amino acids with the following sequence: HGVSGHGQHGVHG (6). Alloferon has stimulatory effects on natural killer (NK) cells and induces in vivo interferon (IFN) production in mice, which indicates the anti-viral and anti-tumor capabilities of alloferon as an immunomodulatory peptide (6). The tumoristatic and tumoricidal activities of alloferon were also reported in DBA/2 mice grafted with syngeneic P388 murine leukemia cells (7). We recently reported that alloferon has dual functions; one involves direct inhibition of the replication of the Kaposi's sarcoma-associated herpesvirus (KSHV) and the other is the effective eradication of virus-infected cells by the activation of NK cells. Alloferon regulated the KSHV life cycle by the down-regulation of activator protein (AP)-1 activity and enhanced anti-viral immunity by up-regulation of NK cell cytotoxicity (8). It was also found that alloferon has anti-tumor effects mediated by the up-regulation of the NK-activating receptor 2B4 and enhancement of granular exocytosis from NK cells (9). In addition, the anti-inflammatory effects of alloferon on UVB-induced inflammation was observed in the human keratinocyte HaCaT cell line and hairless mouse skin (10).
In the present study, we examined the anti-inflammatory effect of alloferon and its possible therapeutic efficacy in a murine colitis model induced with DSS.
C57BL/6 mice were maintained under specific pathogen-free conditions at the animal facility of the Seoul National University College of Medicine. Eight- to ten-week-old male mice were used in the experiments. All animal experiments were reviewed and approved by the Institutional Animal Care and Use Committee of the Seoul National University. Mice were administered 3% DSS (MP Biomedicals Irvine, CA, USA) dissolved in drinking water for 7 days to induce colitis. Alloferon was kindly provided by EntoPharm (Seoul, Korea). Alloferon (50 µg) in normal saline was intraperitoneally (i.p.) injected to mice. On day 4 after DSS administration, alloferon was injected for another 4 consecutive days.
The mice were monitored daily for behavior, water and food consumption, body weight, stool consistency, and the presence of gross blood in the stool or anus, which were presented as the disease activity index (DAI). The DAI was calculated as follows, (stool consistency+gross bleeding+weight loss)/3, based on Table I.
After the mice had been euthanized, the colon was excised, and the length was measured from the anus to the ileocecal valve.
The colon was washed in PBS, fixed in 4% paraformaldehyde (PFA), paraffin-embedded, sectioned, and then stained with H&E. The histological assessment was performed by a trained pathologist who was blinded to the treatment. All histological quantification was performed in a blinded fashion using a scoring system. The histological grade was calculated based on Table II. The sum of each score in the five denoted categories was divided by five.
The blood was collected from the orbital plexus using heparinized capillary tubes under anesthesia with zoletil and xylazine (25 and 10 mg/kg, respectively). After centrifugation at 14,000 rpm for 30 min at 4℃, the plasma obtained was stored at -70℃ until used. The plasma IL-6 concentration measured using an ELISA kit according to the manufacturer's instruction (R&D Systems, Minneapolis, MN, USA).
The Colo205 (human colon cancer cell line) was maintained in Roswell Park Memorial Institute (RPMI)) 1640 medium (Welgene, Seoul, Korea) supplemented with 10% heat-inactivated FBS (HyClone, Logan, UT, USA), 100 U/ml penicillin, and 100 µg/ml streptomycin (Welgene, Seoul, Korea) at 37℃ in an atmosphere of 5% CO2.
The Colo205 cells (1×106) were seeded on a 6-well plate and treated with alloferon (1 µg) for 24 h. Then, TNF-α (10 ng/ml) was added for 10 min. After washing the cells with PBS, they were homogenized with lysis buffer and total proteins were quantified using the bicinchoninic acid (BCA) assay. Equal amounts of protein were resolved using a 10% SDS-PAGE and then transferred to a nitrocellulose membrane. After blocking with 5% nonfat milk, the membranes were incubated overnight with antibodies for anti-phospho (p)-Iκ B, anti-Iκ B (Cell Signaling, Danvers, MA, USA), or β-actin (Sigma, St. Louis, MO, USA) at 4℃. After incubating with HRP-conjugated anti-rabbit or anti-mouse IgG (Cell Signaling, Danvers, MA, USA), the immunoreactive proteins were visualized with an ECL detection system (Amersham Biosciences Corp., Piscataway, NJ, USA).
The data were expressed as mean±SD for each group of independent experiments. For the comparison of three or more groups, the data were analyzed using the Student's t-test or one-way ANOVA followed by the Newman-Keuls multiple comparison test. A p-value<0.05 was considered statistically significant. The statistical analyses were carried out using the GraphPad InStat (GraphPad Software, San Diego, CA, USA).
To induce colitis, mice were treated with 3% DSS in their drinking water for 7 days. To evaluate the effect of alloferon, it was injected into mice once a day for 4 days (Fig. 1). The body weight was decreased (Fig. 2A) and the length of the colon from the anus to the ileocecal valve contracted in all mice with DSS treatment (Fig. 2B). To evaluate the severity of the colitis, the stool consistency, gross bleeding, and weight loss were scored and represented the results were expressed as the DAI. DSS administration significantly increased the disease activity (Fig. 2C). Alloferon treatment did not reduce the weight loss caused by DSS treatment (Fig. 2A). However, alloferon effectively decreased the colon contraction, and thereby increased the colon length (Fig. 2B). In addition, the bloody stool and diarrhea were reduced, and these effects collectively decreased the DAI (Fig. 2C). Therefore, it appears that alloferon had a mitigating effect on the DSS-induced colitis.
The colon of the DSS-treated mice showed more severe destruction of the epithelial architecture with a loss of crypts and epithelial integrity, submucosal edema, and intense inflammatory cellular infiltration in all layers than that of the controls did (Fig. 3A). The histological grade indicated the presence of severe inflammation in the DSS-treated mice (Fig. 3B). The alloferon- and DSS-treated mice also showed severe inflammation, which included edema and epithelial erosion. However, the epithelial integrity was less disrupted, and the number of infiltrated cells was reduced more following the alloferon injection than it was without treatment (Fig. 3A). Interleukin (IL-6) is a pro-inflammatory cytokine that is increased by DSS treatment (111213). To evaluate the inflammation, the level of IL-6 was measured in the plasma of mice after DSS or alloferon treatment. The result showed that DSS administration considerably increased the production of IL-6, and this effect was significantly decreased by alloferon (Fig. 3C). In addition, one of the immunoregulatory cytokines, IL-10 (1415) was measured, and the level was increased following DSS treatment and this effects was decreased by alloferon. However, the result was not significant (data not shown). Taken together, the results showed that DSS treatment induced a severe inflammation, which was attenuated by the injection of alloferon.
To determine the possible mechanism underlying the alloferon-induced decrease of the inflammation in colitis, we examined the degradation and phosphorylation of IκB using immunoblotting. It has been reported that DSS-induced murine colitis activates Nuclear factor-kappaB (NF-kB) signaling, which is critical in the pathophysiology of IBD (161718). The key step in NF-κB activation is the release of the NF-κB dimers from their inhibitory proteins, which is mediated via proteolysis of Iκ B (19). Tumor nerosis factor-alpha (TNF-α) is known to initiate signal transduction via NF-κB (1720). TNF-α increases the phosphorylation of Iκ B and activates NF-κB to transcribe numerous inflammatory genes. In Fig. 4, TNF-α treatment was shown to increase the expression of p-Iκ B and decrease that of Iκ B in the Colo205 colon cancer cell line. The increased degradation of IκB was remarkably reduced following alloferon treatment.
Although the exact pathogenesis of IBD remains unclear, recent evidence suggests that IBD results from an inappropriate inflammatory response to intestinal microbes in genetically susceptible individuals (121). The incidence and prevalence of IBD are increasing in different regions of the world, indicating its emergence as a global disease (22). However, there is no ideal therapeutic agent and research focused on developing a more in-depth and integrated understanding of the mechanisms mediating intestinal immune homeostasis and therapy are needed. In the present study, the immunomodulatory peptide alloferon was shown to decreased the DSS-induced inflammation, infiltration of immune cells, and IL-6 production, which eventually reduced the severity of colitis. This effect was evidenced by a decrease in the DAI level and histological grade.
Alloferon was first isolated from the bacterial- challenged larvae of the blowfly C. vicina based on the fact that insects can rapidly eliminate microbes or fungi by producing a variety of anti-bacterial and anti-fungal substances (6). The pharmaceutical value of the peptide has been mainly related to its ability to not only stimulate NK cytotoxicity and IFN production in animal and human models, but to also enhance anti-viral and anti-tumor activities in mice (789). The antiviral and immunomodulatory effects of alloferon have also been clinically proved in patients infected with herpes simplex virus (HSV) and the human papillomavirus (HPV) (2324). We recently reported that alloferon decreased the production of UVB-induced pro-inflammatory cytokines such as IL-1α, IL-1β, IL-6, and IL-18 by the inhibition of p38 mitogen-activated protein kinase (MAPK) inactivation (10). The present study also verified the anti-inflammatory effect of alloferon in a murine colitis model using DSS (Fig. 2 and 3).
In IBD, the levels of various pro-inflammatory cytokines such as IL-1, IL-6, TNF-α, and IFN-γ are known to be increased. NF-κB activation stimulates the expression of IL-1, IL-6, IL-8, and TNF-α (25). Among these cytokines, the level of IL-6 was investigated following DSS and alloferon treatment (Fig. 3C). IL-6 plays an important role in enhancing T-cell survival and apoptosis resistance in the lamina propria at the site of inflammation (26). In addition, it promotes the survival of intestinal epithelial cells (2728). The concentration of IL-6 was increased by DSS treatment, and this effect was decreased following alloferon treatment (Fig. 3C). This suggests that alloferon efficaciously decreased the inflammation and severity of colitis. Because IL-6 activates Signal transducer and activator of transcription 3 (STAT3) for epithelial survival, the changes in STAT3 signaling and IL-6 production in the inflamed colonic tissue need to be further studied.
Patients with chronic UC and CD have an increased risk of developing colorectal cancer (29). Therefore, we also examined the effect of alloferon on colon cancer cells. Alloferon is known to activate NF-κB signaling by downregulating antioxidant proteins and Iκ Bα (30). However, alloferon treatment decreased the degradation and phosphorylation of Iκ B in colon cancer cells (Fig. 4), indicating the inactivation of NF-κB signaling. NF-κB activation by alloferon was reported to stimulate the synthesis of IFN, thereby inducing anti-viral function in human Burkitt's lymphoma cells containing HPV (30). There has been no report determining the signaling mechanism induced by alloferon in any tumor cells. Therefore, the effect of alloferon including its dephosphorylation of Iκ B in tumor cells should be further investigated. Furthermore, the immunoregulatory effects of alloferon should be investigated intensely in a cancer model as a research subject because alloferon enhances NK cell activity, which play a critical role in host immunity against cancer (31).
In summary, alloferon, a peptide consisting of 13 amino acids showed anti-inflammatory effects in an inflamed colon. Further studies are warranted to elucidate the underlying mechanisms and to intensively evaluate its therapeutic potential in colitis and colon cancer treatment.
Figures and Tables
 | Figure 1Experimental design of dextran sulfate sodium (DSS) and alloferon treatment. Mice were treated with 3% DSS administered in drinking water for 7 days. Alloferon (50 µg/mouse, i.p.) was daily injected to mice four times from day 4 of DSS treatment. |
 | Figure 2Alloferon decreased the severity of dextran sulfate sodium (DSS)-induced colitis. (A) Body weight was monitored for 7 days following 3% DSS and alloferon (50 µg/mouse) treatment. (B) After DSS and alloferon treatment for 7 days, colon length of each experimental group was measured (n=three, *p<0.05, **p<0.01). (C) Body weight loss, stool consistency, and bloody stool were presented as DAI according to the criteria described in the Materials and Methods. DAI calculated as, (stool consistency+gross bleeding+weight loss)/3, *p<0.05, ***p<0.001. DAI, disease activity index; ctl, control; Allo, alloferon. |
 | Figure 3Alloferon decreased inflammation and IL-6 production in dextran sulfate sodium (DSS)-induced colitis. (A) Colons were longitudinally sectioned and stained with H&E. Scale bar, 200 and 100 µm (upper and lower panels, respectively). (B) Cross-sectioned colons were stained with H&E and severity was scored according to criteria described in Materials and Methods (n=three, **p<0.01. (C) After DSS and alloferon treatment, the blood was collected in heparinized capillaries. After centrifugation, the plasma concentration of IL-6 was measured using ELISA, *p<0.05; ctl, control; Allo, alloferon. |
 | Figure 4Alloferon inhibited Iκ B degradation. Colo205 cells (1×106) were treated with TNF-α (10 ng/ml) for 10 min after alloferon pre-treatment (1 µg) for 24 h. The expression of IκB and phospho-(p)-IκB was determined using immunoblotting. β-actin was used as a loading control. |
Table I
Disease activity index (DAI)
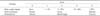
| Category | Score | ||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |
| Body weight change | None | 1~5% | 5~10% | 10~20% | >20% |
| Stool consistency | Normal | Loose | Diarrhea | ||
| Hematochezia | Absence | Blood tinged | Presence | ||
Table II
Histological grade

ACKNOWLEDGEMENTS
This work is supported by the grants (04-2011-1030) from Seoul National University Hospital to Jong Pil Im.
References
1. Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007; 448:427–434.

2. Baumgart DC, Sandborn WJ. Inflammatory bowel disease: clinical aspects and established and evolving therapies. Lancet. 2007; 369:1641–1657.

3. Thia KT, Loftus EV Jr, Sandborn WJ, Yang SK. An update on the epidemiology of inflammatory bowel disease in Asia. Am J Gastroenterol. 2008; 103:3167–3182.

4. Yang SK, Yun S, Kim JH, Park JY, Kim HY, Kim YH, Chang DK, Kim JS, Song IS, Park JB, Park ER, Kim KJ, Moon G, Yang SH. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 814:542–549.

5. Kraus TA, Toy L, Chan L, Childs J, Cheifetz A, Mayer L. Failure to induce oral tolerance in Crohn's and ulcerative colitis patients: possible genetic risk. Ann N Y Acad Sci. 2004; 1029:225–238.

6. Chernysh S, Kim SI, Bekker G, Pleskach VA, Filatova NA, Anikin VB, Platonov VG, Bulet P. Antiviral and antitumor peptides from insects. Proc Natl Acad Sci U S A. 2002; 99:12628–12632.

7. Chernysh S, Irina K, Irina A. Anti-tumor activity of immunomodulatory peptide alloferon-1 in mouse tumor transplantation model. Int Immunopharmacol. 2012; 12:312–314.

8. Lee N, Bae S, Kim H, Kong JM, Kim HR, Cho BJ, Kim SJ, Seok SH, Hwang YI, Kim S, Kang JS, Lee WJ. Inhibition of lytic reactivation of Kaposi's sarcoma-associated herpesvirus by alloferon. Antivir Ther. 2011; 16:17–26.

9. Bae S, Oh K, Kim H, Kim Y, Kim HR, Hwang YI, Lee DS, Kang JS, Lee WJ. The effect of alloferon on the enhancement of NK cell cytotoxicity against cancer via the up-regulation of perforin/granzyme B secretion. Immunobiology. 2013; 218:1026–1033.

10. Kim Y, Lee SK, Bae S, Kim H, Park Y, Chu NK, Kim SG, Kim HR, Hwang YI, Kang JS, Lee WJ. The anti-inflammatory effect of alloferon on UVB-induced skin inflammation through the down-regulation of pro-inflammatory cytokines. Immunol Lett. 2013; 149:110–118.

11. Lee MJ, Lee JK, Choi JW, Lee CS, Sim JH, Cho CH, Lee KH, Cho IH, Chung MH, Kim HR, Ye SK. Interleukin-6 induces S100A9 expression in colonic epithelial cells through STAT3 activation in experimental ulcerative colitis. PLoS One. 2012; 7:e38801.

12. Sander LE, Obermeier F, Dierssen U, Kroy DC, Singh AK, Seidler U, Streetz KL, Lutz HH, Müller W, Tacke F, Trautwein C. Gp130 signaling promotes development of acute experimental colitis by facilitating early neutrophil/macrophage recruitment and activation. J Immunol. 2008; 181:3586–3594.

13. Lin Y, Yang X, Yue W, Xu X, Li B, Zou L, He R. Chemerin aggravates DSS-induced colitis by suppressing M2 macrophage polarization. Cell Mol Immunol. 2014; 11:355–366.

14. Li B, Alli R, Vogel P, Geiger TL. IL-10 modulates DSS-induced colitis through a macrophage-ROS-NO axis. Mucosal Immunol. 2014; 7:869–878.

15. Jarry A, Bossard C, Bou-Hanna C, Masson D, Espaze E, Denis MG, Laboisse CL. Mucosal IL-10 and TGF-beta play crucial roles in preventing LPS-driven, IFN-gamma-mediated epithelial damage in human colon explants. J Clin Invest. 2008; 118:1132–1142.
16. Marrero JA, Matkowskyj KA, Yung K, Hecht G, Benya RV. Dextran sulfate sodium-induced murine colitis activates NF-kappaB and increases galanin-1 receptor expression. Am J Physiol Gastrointest Liver Physiol. 2000; 278:G797–G804.
17. Andresen L, Jørgensen VL, Perner A, Hansen A, Eugen-Olsen J, Rask-Madsen J. Activation of nuclear factor kappaB in colonic mucosa from patients with collagenous and ulcerative colitis. Gut. 2005; 54:503–509.

18. Rogler G, Brand K, Vogl D, Page S, Hofmeister R, Andus T, Knuechel R, Baeuerle PA, Schölmerich J, Gross V. Nuclear factor kappaB is activated in macrophages and epithelial cells of inflamed intestinal mucosa. Gastroenterology. 1998; 115:357–369.

19. Kanarek N, London N, Schueler-Furman O, Ben-Neriah Y. Ubiquitination and degradation of the inhibitors of NF-kappaB. Cold Spring Harb Perspect Biol. 2010; 2:a000166.
20. Chandel NS, Trzyna WC, McClintock DS, Schumacker PT. Role of oxidants in NF-kappa B activation and TNF-alpha gene transcription induced by hypoxia and endotoxin. J Immunol. 2000; 165:1013–1021.

21. Hanauer SB. Inflammatory bowel disease: epidemiology, pathogenesis, and therapeutic opportunities. Inflamm Bowel Dis. 2006; 12:Suppl 1. S3–S9.

22. Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema HW, Kaplan GG. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012; 142:46–54.

23. Ershov F, Kubanova A, Pinegin B, Shulzhenko A, Bekker G, Chernysh S. Allokine-α effect on the course of chronic genital herpes relapses. Materia Medica. 2003; 40:103–111.
24. Chernysh S, Gordja N. The immune system of maggots of the blow fly (Calliphora vicina) as a source of medicinal drugs. J Evol Biochem Physiol. 2011; 47:524–533.

25. Taylor BS, de Vera ME, Ganster RW, Wang Q, Shapiro RA, Morris SM Jr, Billiar TR, Geller DA. Multiple NF-kappaB enhancer elements regulate cytokine induction of the human inducible nitric oxide synthase gene. J Biol Chem. 1998; 273:15148–15156.

26. Neurath MF, Finotto S, Fuss I, Boirivant M, Galle PR, Strober W. Regulation of T-cell apoptosis in inflammatory bowel disease: to die or not to die, that is the mucosal question. Trends Immunol. 2001; 22:21–26.

27. Grivennikov S, Karin E, Terzic J, Mucida D, Yu GY, Vallabhapurapu S, Scheller J, Rose-John S, Cheroutre H, Eckmann L, Karin M. IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell. 2009; 15:103–113.

28. Jin X, Zimmers TA, Zhang Z, Pierce RH, Koniaris LG. Interleukin-6 is an important in vivo inhibitor of intestinal epithelial cell death in mice. Gut. 2010; 59:186–196.

29. Triantafillidis JK, Nasioulas G, Kosmidis PA. Colorectal cancer and inflammatory bowel disease: epidemiology, risk factors, mechanisms of carcinogenesis and prevention strategies. Anticancer Res. 2009; 29:2727–2737.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download