Abstract
Purpose
In the present study, we investigated the clinical characteristics of tuberculosis in school-age children and adolescents, which is important as a reservoir for future disease burden.
Methods
Ninety patients, aged from 6 to 18 years, who were diagnosed and treated with tuberculosis during the period from January 2005 to July 2011, were enrolled. We retrospectively analyzed the medical records and investigated clinical characteristics of the patients.
Results
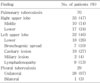
Eight patients were 6 to 12 (9%) and 82 were over 13 years of age (91%). There was a significantly higher percentage of males than females in the latter age group (P<0.01). Route of infection was not confirmed in 74 patients, and 16 patients were diagnosed through the school or military medical examinations with no clinical symptoms. Seventy patients (78%) were presented with pulmonary tuberculosis. Chronic persistent coughing was the most common presenting symptom, and both upper lobes were most frequently involved. Nineteen patients over 13 years of age had adult-type cavitary tuberculosis. The positive results for acid-fast smears or cultures were not high, and the rate of positive tuberculin skin test was 88%. The most frequent adverse effects of anti-tuberculosis treatment were hepatotoxicity, hyperuricemia, and gastrointestinal disorders. The duration of the treatment was much prolonged in 8 patients who had drug-resistant tuberculosis.
Conclusion
Our study showed that pulmonary tuberculosis should be suspected in the adolescents who have prolonged respiratory symptoms. It also indicates that pulmonary tuberculosis in adolescents has similar characteristics to tuberculosis in adults, which suggests the potential important role of adolescent tuberculosis in community disease transmission.
Figures and Tables
References
1. Choi KM, Kim NH, Kim DH, Kim YJ, Kim JH, Oh SH, et al. Korean Guidelines for Diagnosis and Treatment of Tuberculosis in Children and Adolescents. Korean J Pediatr Infect Dis. 2011. 18:1–14.

2. Eun BW. Characteristics of tuberculosis in children and adolescents. Korean J Pediatr. 2009. 52:513–518.

3. Donald PR, Marais BJ, Barry CE 3rd. Age and the epidemiology and pathogenesis of tuberculosis. Lancet. 2010. 375:1852–1854.

4. Marais BJ, Schaaf HS. Childhood tuberculosis: an emerging and previously neglected problem. Infect Dis Clin North Am. 2010. 24:727–749.

7. Marais BJ, Gie RP, Schaaf HS, Beyers N, Donald PR, Starke JR. Childhood pulmonary tuberculosis: old wisdom and new challenges. Am J Respir Crit Care Med. 2006. 173:1078–1090.
9. Marais BJ, Gie RP, Schaaf HS, Hesseling AC, Obihara CC, Starke JJ, et al. The natural history of childhood intra-thoracic tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis. 2004. 8:392–402.
10. Marais BJ, Gie RP, Hesseling AH, Beyers N. Adult-type pulmonary tuberculosis in children 10-14 years of age. Pediatr Infect Dis J. 2005. 24:743–744.

11. Curtis AB, Ridzon R, Vogel R, McDonough S, Hargreaves J, Ferry J, et al. Extensive transmission of Mycobacterium tuberculosis from a child. N Engl J Med. 1999. 341:1491–1495.

12. Marais BJ, Obihara CC, Warren RM, Schaaf HS, Gie RP, Donald PR. The burden of childhood tuberculosis: a public health perspective. Int J Tuberc Lung Dis. 2005. 9:1305–1313.
13. Verver S, Warren RM, Munch Z, Richardson M, van der Spuy GD, Borgdorff MW, et al. Proportion of tuberculosis transmission that takes place in households in a high-incidence area. Lancet. 2004. 363:212–214.

14. Menzies D, Pai M, Comstock G. Meta-analysis: new tests for the diagnosis of latent tuberculosis infection: areas of uncertainty and recommendations for research. Ann Intern Med. 2007. 146:340–354.

15. Machado A Jr, Emodi K, Takenami I, Finkmoore BC, Barbosa T, Carvalho J, et al. Analysis of discordance between the tuberculin skin test and the interferon-gamma release assay. Int J Tuberc Lung Dis. 2009. 13:446–453.
16. Farhat M, Greenaway C, Pai M, Menzies D. False-positive tuberculin skin tests: what is the absolute effect of BCG and non-tuberculous mycobacteria? Int J Tuberc Lung Dis. 2006. 10:1192–1204.
17. Goodwin RA, Des Prez RM. Apical localization of pulmonary tuberculosis, chronic pulmonary histoplasmosis, and progressive massive fibrosis of the lung. Chest. 1983. 83:801–805.

18. Leung AN, Müller NL, Pineda PR, FitzGerald JM. Primary tuberculosis in childhood: radio-graphic manifestations. Radiology. 1992. 182:87–91.

19. Andronikou S, Joseph E, Lucas S, Brachmeyer S, Du Toit G, Zar H, et al. CT scanning for the detection of tuberculous mediastinal and hilar lymphadenopathy in children. Pediatr Radiol. 2004. 34:232–236.

20. Donald P, Maher D, Maritz S, Qazi SA. World Health Organization. Ethambutol efficacy and toxicity: Literature review and recommendation for daily and intermittent dosage in children (WHO/HTM/TB/2006.365). 2006. Geneva, Switzerland:




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download