Abstract
Purpose
The incidence of endobronchial tuberculosis in children is unknown, due to the inconsistent implementation of bronchoscopy in pediatric patients with pulmonary tuberculosis. In this study, our aim was to determine the incidence and clinical course of endobronchial tuberculosis in children.
Methods
We performed a retrospective chart review of patients less than 18 years of age, who was diagnosed with endobronchial tuberculosis via fiberoptic bronchoscopy.
Results
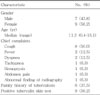
Out of the 101 patients with pulmonary tuberculosis, 16 patients had endobronchial tuberculosis. The median age at diagnosis was 11.2 years (range, 5 months to 16.1 years). Tuberculin skin test was positive in 9 cases (56.2%), and 6 patients (37.5%) had a history of household contact with tuberculosis. Consolidation lesion was common in the simple chest radiographs of patients with endobronchial tuberculosis. According to the bronchoscopic finding, actively caseating type was most common (43.8%). Nine of the 16 patients of endobronchial tuberculosis progressed to bronchial obstruction and 4 patients underwent pneumonectomy or lobectomy. Fibrostenotic and tumorous type tend to progress to endobronchial obstruction compared with actively caseating type.
Figures and Tables
 | Fig. 1Outcome of the patients with endobronchial tuberculosis according to the types of endobronchial tuberculosis (A) and treatment modalities (B). antiTB, antituberculosis medication. |
References
1. World Health Organization. Global tuberculosis control: WHO report 2011. 2011. Geneva: World Health Organization.
2. Nelson LJ, Wells CD. Global epidemiology of childhood tuberculosis. Int J Tuberc Lung Dis. 2004. 8:636–647.
3. Korea Center for Disease Control and Prevention, Korean institute of tuberculosis. Annual report on the notified tuberculosis patients in Korea 2010. 2011. Seoul: Korea Center for Disease Control and Prevention.
4. Daly JF, Brown DS, Lincoln EM, Wilking VN. Endobronchial tuberculosis in children. Dis Chest. 1952. 22:380–398.

5. Park IW, Choi BW, Hue SH. Prospective study of corticosteroid as an adjunct in the treatment of endobronchial tuberculosis in adults. Respirology. 1997. 2:275–281.

6. Matthews JI, Matarese SL, Carpenter JL. Endobronchial tuberculosis simulating lung cancer. Chest. 1984. 86:642–644.

7. Caglayan S, Coteli I, Acar U, Erkin S. Endobronchial tuberculosis simulating foreign body aspiration. Chest. 1989. 95:1164.

8. Lee JH, Park SS, Lee DH, Shin DH, Yang SC, Yoo BM. Endobronchial tuberculosis. Clinical and bronchoscopic features in 121 cases. Chest. 1992. 102:990–994.
9. de Blic J, Azevedo I, Burren CP, Le Bourgeois M, Lallemand D, Scheinmann P. The value of flexible bronchoscopy in childhood pulmonary tuberculosis. Chest. 1991. 100:688–692.

10. Chan S, Abadco DL, Steiner P. Role of flexible fiberoptic bronchoscopy in the diagnosis of childhood endobronchial tuberculosis. Pediatr Infect Dis J. 1994. 13:506–509.

11. Cakir E, Uyan ZS, Oktem S, Karakoc F, Ersu R, Karadag B, et al. Flexible bronchoscopy for diagnosis and follow up of childhood endobronchial tuberculosis. Pediatr Infect Dis J. 2008. 27:783–787.

12. Chung HS, Lee JH, Han SK, Shim YS, Kim KY, Han YC, et al. Classification of endobronchial tuberculosis by the bronchoscopic fratures. Tuberc Respir Dis. 1991. 38:108–115.

13. Chung HS, Lee JH. Bronchoscopic assessment of the evolution of endobronchial tuberculosis. Chest. 2000. 117:385–392.

14. An JY, Lee JE, Park HW, Lee JH, Yang SA, Jung SS, et al. Clinical and bronchoscopic features in endobronchial tuberculosis. Tuberc Respir Dis. 2006. 60:532–539.

15. Kim HJ, Kim HS, Ma JE, Lee SJ, Ham HS, Cho YJ, et al. Clinical characteristics of endobronchial tuberculosis that develops in patients over 70 years of age. Tuberc Respir Dis. 2007. 63:412–416.

16. Toppet M, Malfroot A, Derde MP, Toppet V, Spehl M, Dab I. Corticosteroids in primary tuberculosis with bronchial obstruction. Arch Dis Child. 1990. 65:1222–1226.

17. Chan HS, Pang JA. Effect of corticosteroids on deterioration of endobronchial tuberculosis during chemotherapy. Chest. 1989. 96:1195–1196.

18. Williams DJ, York EL, Nobert EJ, Sproule BJ. Endobronchial tuberculosis presenting as asthma. Chest. 1988. 93:836–838.

19. Chan HS, Sun A, Hoheisel GB. Endobronchial tuberculosis--is corticosteroid treatment useful? A report of 8 cases and review of the literature. Postgrad Med J. 1990. 66:822–826.

20. Brown M, Varia H, Bassett P, Davidson RN, Wall R, Pasvol G. Prospective study of sputum induction, gastric washing, and bronchoalveolar lavage for the diagnosis of pulmonary tuberculosis in patients who are unable to expectorate. Clin Infect Dis. 2007. 44:1415–1420.

21. Singh M, Moosa NV, Kumar L, Sharma M. Role of gastric lavage and broncho-alveolar lavage in the bacteriological diagnosis of childhood pulmonary tuberculosis. Indian Pediatr. 2000. 37:947–951.
22. Anderson C, Inhaber N, Menzies D. Comparison of sputum induction with fiber-optic bronchoscopy in the diagnosis of tuberculosis. Am J Respir Crit Care Med. 1995. 152(5 Pt 1):1570–1574.

23. Abadco DL, Steiner P. Gastric lavage is better than bronchoalveolar lavage for isolation of Mycobacterium tuberculosis in childhood pulmonary tuberculosis. Pediatr Infect Dis J. 1992. 11:735–738.

24. Somu N, Swaminathan S, Paramasivan CN, Vijayasekaran D, Chandrabhooshanam A, Vijayan VK, et al. Value of bronchoalveolar lavage and gastric lavage in the diagnosis of pulmonary tuberculosis in children. Tuber Lung Dis. 1995. 76:295–299.

25. Liam CK, Chen YC, Yap SF, Srinivas P, Poi PJ. Detection of Mycobacterium tuberculosis in bronchoalveolar lavage from patients with sputum smear-negative pulmonary tuberculosis using a polymerase chain reaction assay. Respirology. 1998. 3:125–129.

26. Tueller C, Chhajed PN, Buitrago-Tellez C, Frei R, Frey M, Tamm M. Value of smear and PCR in bronchoalveolar lavage fluid in culture positive pulmonary tuberculosis. Eur Respir J. 2005. 26:767–772.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download