Abstract
Background
Primary central nervous system lymphoma (PCNSL) rarely relapses in extracranial sites, and no specialized guidelines for follow-up evaluation have been proposed.
Methods
We analyzed 65 patients with newly diagnosed PNCSL to evaluate the pattern of relapse and prognostic factors.
Results
Of the 65 patients analyzed, 55 had only parenchymal brain disease, and 10 had both intracranial and extracranial lesions. As a first-line treatment, 29 patients received chemotherapy only (CTx), 13 received chemotherapy followed by whole brain radiotherapy (CTx-WBRT), 18 received chemotherapy followed by autologous stem cell transplantation (CTx-ASCT), 2 received palliative WBRT, and 3 received best supportive care. The overall response rate to the initial treatment was 75.8%, with specific response rates of 62.1% to CTx, 84.6% to CTx-WBRT, and 100% to CTx-ASCT. The complete response (CR) rate was higher with CTx-ASCT than in the absence of ASCT (77.8% vs. 43.2%; P=0.025). After a median follow-up of 18.8 months, the median failure-free survival (FFS) and overall survival (OS) were 13.0 and 36.1 months, respectively. No systemic relapse without a CNS lesion was noted. Multivariate analysis showed that ASCT was predictive of better FFS but not of OS. Age and the Memorial-Sloan Kettering Cancer Center prognostic score were predictive of survival.
Primary central nervous system lymphoma (PCNSL) is a rare B-cell variant of non-Hodgkin lymphoma that is confined to the brain, leptomeninges, spinal cord, and eyes. Although PCNLS is sensitive to corticosteroids, chemotherapy, and radiotherapy, outcomes for patients with PCNSL are substantially worse than for patients at similar stages of systemic non-Hodgkin lymphoma. High-dose methotrexate (HD-MTX)-based chemotherapy or high-dose chemotherapy (HDC) followed by autologous stem cell transplantation (ASCT) are emerging as alternative strategies for patients with PCNSL [1-4]. Despite these advances in treatment, up to half of patients relapse after initial remission, and 10-15% of patients are primarily refractory to treatment [5]. PCNSL rarely relapses in extracranial sites, but a systematic approach to reevaluating disease status at relapse has not been utilized in these patients [5]. Furthermore, no specific guidelines have been proposed for follow-up evaluation of patients treated for PCNSL.
Prognostic models such as the International Extranodal Lymphoma Study group (IELSG) scoring system and the Memorial-Sloan Kettering Cancer Center (MSKCC) prognostic score based on age, performance status (PS), and extent of disease have been proposed to assess the prognosis of patients with PCNSL and to allow appropriate therapeutic decision making [6, 7]. However, prognostic factors have not been assessed fully in patients with PCNSL treated with HD-MTX-based chemotherapy or HDC followed by ASCT. We therefore evaluated patterns of relapse and investigated prognostic factors for PCNSL in a single-center cohort.
The study population included 65 patients newly diagnosed with PCNSL at Asan Medical Center, Seoul, Korea, between November 1995 and August 2010. Patient characteristics including age, Eastern Cooperative Oncology Group (ECOG) PS, international prognostic index (IPI), and treatment information were collected from the ASCT data registry at our center.
Staging evaluations for each patient involved a physical examination, including slit-lamp assessment by an ophthalmologist; contrast-enhanced magnetic resonance imaging (MRI) of the brain; computed tomography (CT) of the thorax, abdomen, and pelvis; lumbar puncture and cerebrospinal fluid (CSF) cytology; bilateral bone marrow (BM) aspiration and biopsy; serology test for HIV; complete blood cell count with differential count; liver and kidney function tests; and serum lactate dehydrogenase (LD) level measurements. Lumbar puncture was not performed in patients suspected of having increased intracranial pressure.
Responses to treatment were assessed according to the criteria of the International Group for PCNSL [8]. Routine follow-up imaging analysis (MRI of the brain and CT) and ophthalmologic exams were performed every 3 months or whenever clinically indicated.
Patient characteristics were described using summary statistics, as medians and ranges, or as proportions. Overall survival (OS) was calculated from the date of diagnosis, to the date of death from any cause or the date of last follow-up for surviving patients. Failure-free survival (FFS) was calculated from the date of diagnosis to date of relapse, progression of disease, death from any cause, or last follow-up. OS and FFS were estimated using the Kaplan-Meier method and compared using the log-rank test. Two-tailed P-values<0.05 were regarded as statistically significant.
The IELSG prognostic scoring system is composed of 5 prognostic variables: age more than 60 years, ECOG score more than 1 (Karnofsky performance status [KPS] <70%), elevated serum LD level, high CSF protein concentration, and involvement of the deep regions of the brain (periventricular regions, basal ganglia, brainstem, and/or cerebellum) [7]. Due to the retrospective nature of this study, resulting in incomplete data, we assessed only the prognostic significance of patient age, ECOG PS, and serum LD level.
The MSKCC prognostic score is a simplified index, including age and KPS [6], with 3 distinct prognostic classes: class 1 (age<50 years), class 2 (age≥50 years or KPS≥70%), and class 3 (age≥50 years and KPS<70%). This scoring system was also used for prognostic analysis.
The clinical characteristics of the 65 patients are summarized in Table 1. Their median age was 55 years (range, 26-77 years). Of these, 63 tumors were histologically diagnosed as diffuse large B-cell lymphoma and 2 as T-cell lymphomas (T-lymphoblastic lymphoma and peripheral T-cell lymphoma). All patients had parenchymal brain disease, and 10 patients (15.4%) had extracranial involvement including 7 with positive CSF cytology, 2 with ocular involvement, and 1 with a spinal cord lesion. Twenty-nine (44.3%) patients received chemotherapy alone (CTx) as first-line treatment, while 13 (20.0%) received CTx followed by whole brain radiotherapy (WBRT) and 18 (27.7%) received CTx followed by ASCT. Two patients with HIV infection received only palliative WBRT, and 3 received best supportive care without any chemotherapy or radiation therapy because of poor PS. No difference in patient characteristics was observed between those treated with and without ASCT (data not shown).
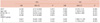
As shown in Table 2, 62 of the 65 patients received first-line treatment with curative intent. The overall response rates (ORR) in patients receiving CTx alone, and CTx followed by WBRT, were 62.1% and 84.6%, respectively. All patients who received chemotherapy followed by ASCT achieved clinical response; of these 77.8% showed complete response (CR) and 12.2% showed partial response (PR). Among the 18 patients treated with CTx followed by ASCT, 5 patients showed PR after CTx, but finally achieved CR after ASCT. The ORR (P=0.031) and CR rate (P=0.025) were significantly higher in patients treated with chemotherapy followed by ASCT than in those treated without ASCT (Table 2).
After a median follow-up duration of 18.8 months (range, 1.1-138.0 months), 31 of the 65 patients had died including 21 from progression or relapse of PCNSL. The median FFS was 13.0 months (95% confidence interval [CI], 3.5-22.8 months) and the median OS was 36.1 months (95% CI, 20.5-51.7 months). The 2-year FFS and OS rates were 42.0% and 66.5%, respectively (Fig. 1). Four treatment-related deaths occurred in patients who received HD-MTX chemotherapy.
The 3 patients who received best supportive care without other treatment showed progression of intracranial lesions, with 1 patient dying from severe pneumonia. Following first-line treatment, 6 patients (9.2%) experienced progression of disease, and 25 (38.5%) experienced relapse of disease, including 21 with brain parenchymal lesions, 1 with an ocular lesion, and 3 with positive CSF cytology (Table 3). No systemic relapse was observed without a CNS lesion.
Following failure of first-line treatment, 33 patients received salvage treatment, including 15 who received salvage CTx, 4 who received salvage CTx followed by ASCT, 11 who received WBRT, and 3 who received best supportive care alone.
FFS was not related to patient age, ECOG PS, serum LD level, or MSKCC prognostic score. Age less than 60 years (P=0.001), ECOG PS ≤1 (P=0.019), and lower MSKCC prognostic score (P=0.001) were related to prolonged OS (Table 4 and Fig. 2). However, patients who received HDC followed by ASCT showed significantly better FFS (58.6 months vs. 9.1 months; P=0.006) and OS (58.6 months vs. 33.3 months; P=0.034) than those who did not (Fig. 3).
Multivariate analysis showed that ASCT was an independent predictive factor for better FFS (hazard ratio [HR], 0.348; 95% CI, 0.151-0.084), but not for OS (Table 5). Age equal to or more than 60 years was the only independent prognostic factor for OS (HR, 2.968; 95% CI, 1.269-6.939). The MSKCC prognostic score was also predictive of patient survival in multivariate analysis.
All of the patients with PCNSL in this study were systematically evaluated at the initial staging and at follow-up, by methods including CTs of the thorax, abdomen and pelvis, lumbar puncture, and positron emission tomography (PET). Analysis of the relapse pattern of PCNSL showed that no patient experienced a systemic relapse without a CNS lesion, in accordance with earlier studies showing that most patients with PCNSL relapsed in the CNS, whereas systemic relapse and simultaneous CNS and systemic relapse were infrequent [5, 9-12]. These studies, however, may have underestimated the frequency of relapse without a CNS lesion, due to the lack of systematic follow-up staging evaluation.
In one of the largest series evaluating the characteristics of patients with relapsed PCNSL, only 6 of 143 patients had isolated systemic relapses [5]. However, not all patients underwent systematic reevaluation of disease status, including CSF analysis and eye examinations, at relapse. In another study, 10 of 209 patients (4.8%) experienced extracerebral relapse without CNS progression [13]. The data of patients in that study, however, was collected retrospectively from several databases, suggesting that systematic evaluation of disease progression might not have been performed using the same methods. In accordance with the findings of these previous studies, we found that isolated systemic relapse without a CNS lesion was extremely rare, even with regular systematic evaluation by brain MRI, CTs of chest, abdomen, and pelvis, and eye examinations, as none of our patients showed isolated systemic relapse. These findings suggest that complete systematic evaluation may be unnecessary, and brain imaging alone may be sufficient for follow-up of patients with PCNSL.
The IELSG prognostic score model is not readily applicable in patients with PCNSL, due to its complexity [7], whereas the MSKCC prognostic score, based on age and PS, is simpler and has higher applicability [6]. Data on prognostic factors are limited in patients treated with HD-MTX-based chemotherapy or HDC followed by ASCT. We therefore analyzed several prognostic factors in 65 patients with PCNSL, including 18 who had been treated with HD-MTX-based chemotherapy followed by ASCT. In accordance with the IELSG and MSKCC prognostic models, we found that age and PS were associated with OS irrespective of treatment. However, due to a lack of information regarding CSF protein levels and the depth of brain lesions in some patients, the IELSG prognostic score was not applicable in this population. In contrast, the MSKCC prognostic score was useful in predicting OS in our patients.
HD-MTX-based chemotherapy followed by ASCT may improve outcomes in selected patients with PCNSL [2, 4]. ASCT may significantly improve both the CR rate and FFS. However, due to the retrospective nature of this study and the small number of patients, our findings require validation in other, larger retrospective and prospective trials.
In conclusion, the observed absence of systemic involvement without a CNS lesion in patients with relapsed PCNSL suggests that regular systematic evaluation to investigate extracranial relapse may not be always necessary in patients with PCNSL. Age was a prognostic factor for OS, irrespective of treatment scheme, and ASCT may improve the CR rate and FFS.
Figures and Tables
Fig. 2
Failure free survival and overall survival according to age (A, B), Eastern Cooperative Oncology Group performance status (ECOG PS) (C, D), serum lactate dehydrogenase (LD) level (E, F), and MSKCC, Memorial-Sloan Kettering Cancer Center (MSKCC) prognostic group (G, H).

Fig. 3
Failure free survival (A) and overall survival (B) in patients treated with and without autologous stem cell transplantation.

Table 2
Responses to first-line treatment (N=62).

a)P-value indicates comparison between non-ASCT and CTx-ASCT groups.
Abbreviations: CR, complete response; PR, partial response; ORR, overall response rate (CR+PR); SD, stable disease; PD, progressive disease; NE, not evaluable; CTx, chemotherapy; WBRT, whole brain radiotherapy; ASCT, autologous stem cell transplantation.
References
1. Milpied N, Deconinck E, Gaillard F, et al. Initial treatment of aggressive lymphoma with high-dose chemotherapy and autologous stem-cell support. N Engl J Med. 2004. 350:1287–1295.

2. Ferreri AJ, Crocchiolo R, Assanelli A, Govi S, Reni M. High-dose chemotherapy supported by autologous stem cell transplantation in patients with primary central nervous system lymphoma: facts and opinions. Leuk Lymphoma. 2008. 49:2042–2047.

3. Morris PG, Abrey LE. Therapeutic challenges in primary CNS lymphoma. Lancet Neurol. 2009. 8:581–592.

4. Yoon DH, Lee DH, Choi DR, et al. Feasibility of BU, CY and etoposide (BUCYE), and auto-SCT in patients with newly diagnosed primary CNS lymphoma: a single-center experience. Bone Marrow Transplant. 2011. 46:105–109.

5. Jahnke K, Thiel E, Martus P, et al. Relapse of primary central nervous system lymphoma: clinical features, outcome and prognostic factors. J Neurooncol. 2006. 80:159–165.

6. Abrey LE, Ben-Porat L, Panageas KS, et al. Primary central nervous system lymphoma: the Memorial Sloan-Kettering Cancer Center prognostic model. J Clin Oncol. 2006. 24:5711–5715.

7. Ferreri AJ, Blay JY, Reni M, et al. Prognostic scoring system for primary CNS lymphomas: the International Extranodal Lymphoma Study Group experience. J Clin Oncol. 2003. 21:266–272.

8. Abrey LE, Batchelor TT, Ferreri AJ, et al. Report of an international workshop to standardize baseline evaluation and response criteria for primary CNS lymphoma. J Clin Oncol. 2005. 23:5034–5043.

9. Blay JY, Conroy T, Chevreau C, et al. High-dose methotrexate for the treatment of primary cerebral lymphomas: analysis of survival and late neurologic toxicity in a retrospective series. J Clin Oncol. 1998. 16:864–871.

10. Abrey LE, Moskowitz CH, Mason WP, et al. Intensive methotrexate and cytarabine followed by high-dose chemotherapy with autologous stem-cell rescue in patients with newly diagnosed primary CNS lymphoma: an intent-to-treat analysis. J Clin Oncol. 2003. 21:4151–4156.

11. Batchelor T, Carson K, O'Neill A, et al. Treatment of primary CNS lymphoma with methotrexate and deferred radiotherapy: a report of NABTT 96-07. J Clin Oncol. 2003. 21:1044–1049.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download