Abstract
Background
The nationwide statistical analysis of hematologic malignancies in Korea has not been reported yet.
Methods
The Korea Central Cancer Registry and the Korean Society of Hematology jointly investigated domestic incidence rates and prevalence of hematologic malignancies occurred between 1999 and 2008, and analyzed survival rates of patients who were diagnosed between 1993 and 2008. Data of hematologic malignancies from 1993 to 2008 were obtained from the Korean National Cancer Incidence Data base. The crude incidence rates, age-specific incidence rates, age-standardized incidence rates, annual percentage change of incidence, and prevalence from 1999-2008 were calculated. Survival rates for patients diagnosed in 1993-2008 were estimated.
Results
In 2008, a total of 8,006 cases of hematologic malignancies were occurred, which comprised 4.5% of all malignancies. In all genders, non-Hodgkin lymphoma, myeloid leukemia, and multiple myeloma were most frequent diseases. In terms of age, ages between 60 and 69 were most prevalent. From 1999 to 2008, the age-standardized incidence rates increased from 10.2 to 13.7, and the annual percentage change was 3.9%. The 5-year survival rate increased from 38.2% during 1993-1995 to 55.2% during 2004-2008. As of January 2009, number of patients with 10-year prevalence was 33,130, and with 5- to 10-year prevalence was 10,515.
Conclusion
This is the first nationwide statistical report of hematologic malignancies in Korea. It could be used as the basic information to help investigate epidemiologic characteristics, evaluate progress during the past years, and establish future strategies for hematologic malignancies. Periodic statistical analysis of hematologic malignancies in Korea should be continued.
The field of hematologic malignancies has continuously advanced for past 50 years in Korea. However, much less attention was paid for its cancer statistical analysis. There has not been a report that analyzed the incidence rate, prevalence rate, and survival rate of the whole nationwide hematologic malignancies and this is also comparable to other developed countries [1, 2]. There are several reasons for the difficulty of analysis. The classification of hematologic malignancies is constantly changing, and cancer registry in each country has different definitions for the subtypes of hematologic malignancies, which jeopardizes the quality of patient data and all these reasons make it difficult to compare hematologic statistics according to time and region. Since 2005, USA and Europe integrated recent International Classification of Diseases-Oncology (ICD-O) and World Health Organization (WHO) classification and with agreements of experts, they classified statistics on hematologic malignancies that fit the objectives of epidemiology and public health care, and published the statistical reports [3-5].
In an effort to determine the characteristics of domestic hematologic malignancies and analyze past survival rates to establish the barometer for creating strategies for the advancement of domestic hematologic malignancies field, the Korea Central Cancer Registry and the Korean Society of Hematology jointly investigated the domestic prevalence rate and incidence rate of hematologic malignancies occurred between 1999 and 2008, and analyzed survival rate of patients who were diagnosed as hematologic malignancies between 1993 and 2008.
Data of hematologic malignancies from 1993 to 2008 were obtained from the Korean National Cancer Incidence Data base (KNCIDB) [6]. Hematologic malignancies were classified according to the International Classification of Diseases for Oncology 3rd edition (ICD-O-3) and converted to the International Classification of Diseases 10th edition (ICD-10) (Table 1) [7, 8]. For myeloproliferative disorders (MPD) and myelodysplastic syndromes (MDS), official registration employing ICD-O-3 began in 2003 at Korea Central Cancer Registry (KCCR).
Crude incidence rates (CRs) and age-specific incidence rates of each hematologic malignancy were calculated. The CRs per 100,000, an incidence rate based on the frequency of cancer in the entire population, were calculated by dividing the total number of events (N) by the total number of person-year of observation (P) and multiplying the result by 100,000. The age-specific incidence rates per 100,000 within age group i, were calculated by dividing the number of incidence observed in the age group (Ni) by the number of corresponding person-year of observation (Pi) and multiplying the result by 100,000. Age-standardized incidence rates (ASRs), a weighted average of crude age-specific rates, were determined by using the mid-year population in Korea in 2000 as standard population. Changes in the annual ASRs were examined by calculating the annual percentage change (APC) over a time period as (exp(b)-1)×100, where b is the slope of the regression of log(ASR) on a calendar year as the following linear regression equation [9]:
E(log(ASR)|year)=a+b year.
The survival analysis used cases of hematologic malignancies first diagnosed during 1993-2008 from KNCIDB, and the vital status of these patients were followed through December 31, 2010. The survival duration of each case was determined as the time difference between the date of initial diagnosis and the date of death, date of loss to follow up, or closing date for follow-up. Observed survival rates were calculated using a life table method, in which survival times are grouped into intervals [10]. Limited-duration prevalent cases are the number of cancer patients alive on a certain day who had been diagnosed with the disease within the past specified years. For example, 10-year prevalent cases in this report were the patients that were diagnosed between 1999 and 2008 and were alive on January 1, 2009. The limited-duration prevalence, such as 1, 5, and 10-year prevalence was calculated using SEER*Stat software [11].
A total national cancer incident cases in 2008 were 178,816 cases. Stomach cancer (15.7%) was most prevalent, followed by thyroid cancer (15.1%), colorectal cancer (12.7%), lung cancer (10.5%), liver cancer (8.8%), and breast cancer (7.1%). Hematologic malignancies occurred in 8,006 patients, which was 4.5% of all cancers next to breast cancer. It occurred in 4,486 men and 3,520 women, and this relates to 4.8% of all cancers occurred in men, and 4.1% of all cancers occurred in women (Fig. 1). Among all hematologic malignancies, non-Hodgkin lymphoma (NHL) was most frequent, followed by myeloid leukemia, and multiple myeloma regardless of gender. Ages between 60 and 69 were most prevalent followed by ages 70 to 79, and ages 50 to 59 (Fig. 2). Lymphoid leukemia was most prevalent in ages below 15 years in both genders while NHL was most prevalent in ages above 15 years (Table 2).
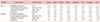
The trends in number of patients, CRs, and ASRs for each hematologic malignancy between 1999 and 2008 are described in Table 3. The overall ASRs of hematologic malignancies increased from 10.2 in 1999 to 13.7 in 2008. The APC was 3.9% between 1999 and 2008 which was higher than 3.3% in all cancers, and APCs were statistically significant in all hematologic malignancies. For age-specific incidence rates in 2008, lymphoid leukemia was the highest in age under 15 years regardless of gender. In both genders, age-specific incidence rates of all hematologic malignancies, except for lymphoid leukemia, increased as age increased; however, age-specific incidence rate decreased after age of 80 in women (Fig. 3).
The survival of all hematologic malignancies continually increased from 1993 to 2008 with 5-year survival rate of 38.2% between 1993 and 1995 to 55.2% between 2004 and 2008, an increase of 17% (Fig. 4). The survival rates increased from 68.5% to 80.9% in Hodgkin lymphoma (HL), from 47.6% to 62.8% in NHL, from 22.9% to 33.2% in multiple myeloma, from 38.9% to 52.4% in lymphoid leukemia, and from 21.9% to 44% in myeloid leukemia. Survival rate of women were slightly higher or similar to men, but in MDS, men had 36.4% of survival rate while women had 50.3%, showing differences.
Survival rate decreased as age increased in most of the hematologic malignancies, and when the age of diagnosis was above 50 years old, the survival rate was even more decreased (Table 4). However, there is a marked difference of survival rate in lymphoid leukemia between groups of diagnostic age of 0-14 years and above 15 years. Five year survival rates according to hematologic malignancies, year, gender and age are described in Table 4.
As of January 2009, the total number of patients with 10 year-prevalence who were diagnosed as hematologic malignancies was 33,130, which comprised 4.6% of total 10 year-prevalence in all cancers. In terms of prevalent cases, the number of patients less than 1 year was 6,548, 1-2 years 5,024, 2-5 years 11,043, and 5-10 years 10,515 (Fig. 5). Patients with more than 5 year-prevalence comprised 32%. NHL was most frequent with 16,142 patients, followed by myeloid leukemia and lymphoid leukemia with 6,068 and 3,066 patients, respectively.
This is the first study to analyze hematologic malignancies, providing a statistical information on all hematologic malignancies in Korea. As with all other cancers, the incidence of hematologic malignancies has been increasing. In comparison with other countries, almost no differences can be seen with Japan and China in the incidences of hematologic malignancies, however, in comparison with western countries including United Kingdom, France, Germany, and Canada, our incidences of HL, NHL, and multiple myeloma were lower, showing distinct differences (Table 5) [12]. This could be regarded as the reflection of differences in race; however, we observed the recent increase of HL, NHL, and multiple myeloma in our country.
MDS and MPD have been officially registered in Korea cancer registry since 2003. USA also began their registration of MDS and MPD in central registry in 2001. According to the analysis of MDS registered in the Surveillance, Epidemiology, and End Results (SEER) and North American Association of Cancer Registry between 2001 and 2004, the incidence rate of MDS was reported to have increased during those times, but the active engagement of registration during those times could have played a role behind the increase [13]. The APC for domestic MDS, MPD were also high between 2003 and 2008, but longer observation of changes in incidence should be implemented.
Multiple factors were thought to have played role in the increase of hematologic malignancies in Korea. Age, infection, genetics, and other environmental factors were suggested as causes of hematologic malignancies, but the exact cause would be difficult to explain [14-17]. According to Europe's HAEMACARE project, the incidence of hematologic malignancies in Europe also increased as age increased [3]. The aging of Korean population structure could be one factor for the increase of hematologic malignancies; however, our study showed significant increase of age-adjusted APC in most of the hematologic malignancies, and it cannot be explained solely by aging. Incidences of all hematologic diseases were lower in women than men, similar with results of Europe's HAEMACARE project. For the explanation of this phenomenon, there had been many interpretation including environmental and occupational risk factor, smoking, alcohol consumption, susceptibility to cancer, and hormonal and genetic differences between men and women [18-20].
The survival rates have continuously improved in all hematologic malignancies in Korea. According to recent NORDICAN database published by Nordic countries-Denmark, Finland, Norway, and Sweden, the 5-year survival rates of HL, NHL, multiple myeloma, and leukemia in those 4 countries from 1999 to 2003 were similar to our survival rates, and also the 5-year survival rates of hematologic malignancy patients in Hong Kong from 1996 to 2001 were comparable to our levels [1, 21].
However, our survival rates in most of the hematologic malignancies do not reach the levels that of the USA [22], and this difference in survival rates could be due to the different prevalent disease type as well as other complex factors. There were big differences in survival rates in domestic hematologic malignancies before and after year 2000; however, in comparison of years between 2001-2005 and 2004-2008, the increase of survival rates were less distinct with only 3% and 0.5% increase of survival rates in NHL, and lymphoid leukemia, respectively.
Just like other malignancies, there is an increase of long term survivors in hematologic malignancies. As seen in this study, there were more than 30,000 patients with 10-year prevalence treated for hematologic malignancies, and this is comparable to long term survivors of cervical cancer, liver cancer, and lung cancer [23]. Due to the improvements in treatment, more long term survivors of hematologic malignancies will be observed. The increase of long term survivors after treatment for cancers including hematologic malignancies may lead to various physical, psychological, and social problems after the cure of malignancies [24]. While we should try on improving the survival rate of the patients, further study involving the overall quality of life of long term survivors of hematologic malignancies would be needed.
Statistics for hematologic malignancies increases the understanding of overall hematologic malignancies, and it could be used as the basic information to help investigate epidemiologic characteristics, evaluate progress during the past years, and establish future strategies for hematologic malignancies. For more detailed analysis and international comparison, the hematologic malignancies registration program in Korea should be set up, and continuous effort and feedback between the Korean Society of Hematology and Korea Central Cancer Registry would be needed.
Figures and Tables
 | Fig. 4Five-year survival rate of hematologic malignancies from 1993 to 2008 in Korea. a)Official registration employing ICD-O-3 began in 2003 at KCCR. |
 | Fig. 5Number of prevalent cases of hematologic malignancies by time since diagnosis in January 1, 2009 in Korea. a)Because official registration for MPD and MDS began in 2003, 5-10 year prevalence cases for these cancers are underestimated. |
Table 2
Ranks of age-specific incidence rates of hematologic malignancies by gender and age group in Korea, 2008.

Table 3
Number of hematologic malignancies and trend in crude incidence rates and age-standardized incidence rates in Korea from 1999 to 2008.

a)Official registration employing ICD-O-3 began in 2003 at KCCR, b)The annual percent change is statistically significantly different from zero (P<0.05).
Abbreviations: CR, crude incidence rate; ASR, age-standardized incidence rate; APC, annual percentage change; MPD, myeloproliferative disorders; MDS, myelodysplastic syndromes.
Table 4
Five-year relative survival rates of hematologic malignancies by gender and age group in Korea.

ACKNOWLEDGEMENTS
The authors thank the Korea Central Cancer Registry (KCCR)-affiliated Hospitals, non KCCR-affiliated Hospitals, 11 Regional Cancer Registries (Busan, Daegu & Gyeongbuk, Gwangju & Jeonnam, Incheon, Daejeon & Chungnam, Ulsan, Gangwon, Chungbuk, Jeonbuk, Gyeongnam, and Jejudo), the National Health Insurance Corporation, and the National Statistical Office for their contribution to data collection for the nationwide cancer registry.
References
1. Storm HH, Klint A, Tryggvadóttir L, et al. Trends in the survival of patients diagnosed with malignant neoplasms of lymphoid, haematopoietic, and related tissue in the Nordic countries 1964-2003 followed up to the end of 2006. Acta Oncol. 2010. 49:694–712.

2. Pulte D, Gondos A, Brenner H. Trends in survival after diagnosis with hematologic malignancy in adolescence or young adulthood in the United States, 1981-2005. Cancer. 2009. 115:4973–4979.

3. Sant M, Allemani C, Tereanu C, et al. Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood. 2010. 116:3724–3734.

4. Marcos-Gragera R, Allemani C, Tereanu C, et al. Survival of European patients diagnosed with lymphoid neoplasms in 2000-2002: results of the HAEMACARE project. Haematologica. 2011. 96:720–728.

5. Morton LM, Turner JJ, Cerhan JR, et al. Proposed classification of lymphoid neoplasms for epidemiologic research from the Pathology Working Group of the International Lymphoma Epidemiology Consortium (InterLymph). Blood. 2007. 110:695–708.

6. Ministry of Health and Welfare. The Korea central cancer registry. Annual report of cancer statistics in Korea in 2008. 2010. Seoul, Korea: Ministry of Health and Welfare.
7. Fritz A, Percy C, Jack A, editors. International classification of diseases for oncology. 2000. 3rd ed. Geneva, Switzerland: World Health Organization.
8. World Health Organization. International statistical classification of diseases and related health problems (ICD-10) in occupational health. 1999. Geneva, Switzerland: World Health Organization.
9. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000. 19:335–351.

10. Lee ET, Wang JW, editors. Statistical methods for survival data analysis. 2003. 3rd ed. Hoboken, NJ: John Wiley & Sons Inc.
11. SEER*Stat software program, version 7.0.5. National Cancer Institute. 2011. Accessed February 7, 2012. Bethsda, MD: National Cancer Institute;at http://seer.cancer.gov/seerstat/.
12. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008 v1.2. Cancer incidence, mortality and prevalence worldwide in 2008. IARC CancerBase No. 10. 2010. Accessed December 1, 2011. Lyon, France: International Agency for Research on Cancer;at http://globocan.iarc.fr/.
13. Rollison DE, Howlader N, Smith MT, et al. Epidemiology of myelodysplastic syndromes and chronic myeloproliferative disorders in the United States, 2001-2004, using data from the NAACCR and SEER programs. Blood. 2008. 112:45–52.

14. Mester B, Nieters A, Deeg E, Elsner G, Becker N, Seidler A. Occupation and malignant lymphoma: a population based case control study in Germany. Occup Environ Med. 2006. 63:17–26.
17. Bezabeh S, Engel A, Morris CB, Lamm SH. Does benzene cause multiple myeloma? An analysis of the published case-control literature. Environ Health Perspect. 1996. 104:Suppl 6. 1393–1398.

18. Alexander DD, Mink PJ, Adami HO, et al. The non-Hodgkin lymphomas: a review of the epidemiologic literature. Int J Cancer. 2007. 120:Suppl 12. 1–39.

19. Gorini G, Stagnaro E, Fontana V, et al. Alcohol consumption and risk of leukemia: a multicenter case-control study. Leuk Res. 2007. 31:379–386.

20. Cook MB, Dawsey SM, Freedman ND, et al. Sex disparities in cancer incidence by period and age. Cancer Epidemiol Biomarkers Prev. 2009. 18:1174–1182.

21. Sankaranarayanan R, Swaminathan R, Jayant K, Brenner H. An overview of cancer survival in Africa, Asia, the Caribbean and Central America: the case for investment in cancer health services. IARC Sci Publ. 2011. 162:257–291.
22. Howlader N, Noone AM, Krapcho M, et al. SEER cancer statistics review, 1975-2008. 2011. Accessed December 1, 2011. Bethesda, MD: National Cancer Institute;at http://seer.cancer.gov/statfacts/html/all.html.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download