Abstract
Background
Invasive pulmonary aspergillosis (IPA) is one of the major complications encountered by patients receiving chemotherapy for hematologic malignancies. The prolonged period of intense immunosuppression following allogeneic hematopoietic stem cell transplantation (HSCT) may increase the risk of IPA recurrence in patients with a history of IPA. We evaluated the impact of a history of IPA on allogeneic HSCT outcome, and examined the incidence of IPA after HSCT.
Methods
This retrospective study included 22 patients with a history of IPA prior to receiving allogeneic HSCT at the Samsung Medical Center from 1995 to 2007. Diagnosis of IPA was defined as proven (N=5), probable (N=0), or possible (N=17).
Results
All 22 patients received amphotericin-based regimens to treat pre-transplant IPA. Secondary antifungal prophylaxis was administered to 10 patients during HSCT. The development of post-transplant IPA was observed in 2 patients. One of the patients died from septic shock within 2 days of the diagnosis of possible IPA. The other patient recovered from IPA, but eventually had a relapse of the primary disease. Of the 22 patients, the overall 2-year survival rate was 63% (95% confidence interval [CI]: 41-85), and the transplant-related mortality rate was 19% (95% CI: 0-38).
Prognosis in hematopoietic stem cell transplantation (HSCT) varies widely depending on disease type, stage, stem cell source, HLA-matched status (for allogeneic HSCT), and conditioning regimen. Transplantation offers the possibility for a cure or a long-term remission if inherent complications such as graft-versus-host disease (GVHD), immunosuppressive treatments, and opportunistic infections can be avoided [1]. Invasive fungal infection (IFI) is a common complication of allogeneic HSCT that most frequently involves the Aspergillus species. In recent years, the number of patients with invasive aspergillosis has increased despite advances in therapy, and the majority of these patients (80-90%) have pulmonary disease [2].
Invasive pulmonary aspergillosis (IPA) is a major complication that causes morbidity and mortality among patients undergoing chemotherapy for hematologic malignancies [3]. The incidence rate of invasive aspergillosis (IA) after allogeneic HSCT exceeds 20%, with mortality rates ranging from 50% to 80% [4]. IPA develops in around 20% of allogeneic HSCT recipients [5], with mortality rate of approximately 60% in patients with chemotherapy-induced neutropenia and sometimes exceeding 90% in patients undergoing HSCT [6]. One retrospective study analyzed the incidence of IA in 166 patients undergoing either allogeneic or autologous HSCT between January 2000 and December 2003 [7]. The results of that study estimated the incidence of IA among allogeneic HSCT recipients at 23% (95% confidence interval [CI]: 16-32), and patients with IA had a significantly lower overall survival rate than patients without IA (8% vs. 56%, P=0.01) due to a higher transplant-related mortality (TRM) rate (63% vs. 31%, P=0.03) [7]. Another study conducted in China reported IFIs in 35 (1 proven; 34 probable diagnoses) of 180 cases (19.5%) of allogeneic HSCT, including 18 cases (51.4%) of aspergillosis and 17 cases (48.6%) of candidiasis. Moreover, a significant difference in 1-year overall survival rates was observed between patients with (34.3%) and without (53.8%) IFI [8].
Due to the prolonged period of intensive immunosuppression that follows allogeneic HSCT, the risk of IPA recurrence after allogeneic HSCT is considered higher among patients with a history of IPA than among those with no history of IPA. Moreover, prior invasive fungal infection increases the patient's risk for TRM due to the possibility of reactivation of the fungal infection. Consequently, a high TRM estimated rate of 60-90% [9] often prevents the patient from undergoing HSCT. According to a 2002 study, the 2 variables that can improve the survival of patients with IPA are neutrophil recovery during therapy and not having undergone allogeneic HSCT [10]. A history of IPA often indicates that the intensity of anti-neoplastic treatment should be reduced. Studies have shown that compared to patients who had received allogeneic HSCT during the same period (100 days earlier), patients with a history of IA had lower overall survival rates (56% vs. 77%; P=0.0001) and higher TRM rates (38% vs. 21%; P=0.0001) that were mainly associated with IA and other pulmonary complications [11].
Nevertheless, successful transplantation without the recurrence of mycotic infection has been reported [12]. Previous reports have suggested that aggressive treatment of IFI followed by adequate antifungal prophylaxis during HSCT can minimize the possibility of IFI recurrence. For instance, a 2005 study reported a low risk of post-HSCT reactivation of previous IFI (11%) [13]. The results of that study demonstrated that the risk of adequately treated fungal infections recurring during HSCT is the same as the risk of developing new fungal infections. However, high-dose chemotherapy should not present a contraindication to HSCT. This is particularly important, as high-dose chemotherapy accompanied by stem cell rescue could be the only chance of a cure for certain malignant conditions. A previous study has shown that pre-transplant treatment of fungal infections followed by antifungal treatment during transplantation may allow HSCT to take place without reactivation of fungal infections in selected patients [14]. Another pediatric study also demonstrated that aggressive therapy of prior fungal infections followed by ongoing anti-fungal prophylaxis might allow bone marrow transplantation in acute leukemia patients without reactivation of the fungal infection [15].
Therefore, the current study aimed to evaluate the impact of a history of IPA prior to allogeneic HSCT on transplant outcome, including examining the incidence of IPA after HSCT.
In this retrospective study, we included 22 patients with a history of IPA prior to undergoing allogeneic HSCT from 1995 to 2007 at the Samsung Medical Center, Seoul, Korea.
Cases were defined as proven, probable, and possible IFI based on the European Organization for Research and Treatment of Cancer/Mycoses Study Group (EORTC/MSG) criteria [16]. Proven aspergillosis required culture and identification. Probable IFI required the presence of a host factor, a clinical criterion, and a mycological criterion. Cases that met the clinical and host factor criteria, but not the mycological criteria, were considered possible IFI. Major findings were defined as any of the following infiltrates newly observed through chest computed tomography (CT), including halo sign, air-crescent sign, or presence of a cavity within an area of consolidation. If the IPA at the time of HSCT was improved, it was defined as overall responsive. If the IPA at the time of HSCT was aggravated, it was defined as progressive. Patients on whom chest CT scan was not performed at the time of IPA diagnosis and patients who did not receive antifungal agents for over 1 week were excluded from the study.
Analyses were performed using the SPSS statistical package (version 15.0; SPSS, Inc, Chicago, IL, USA). Categorical variables were compared using the chi square test or Fisher's exact test when appropriate. We performed a retrospective analysis that included: age, sex, radiographic lesions (chest CT findings), cultures, diagnosis, therapy, donor type, stem cell source, primary disease state at HSCT, conditioning regimen, stage of chemotherapy, duration of neutropenia, secondary prophylaxis of IPA, acute and chronic GVHD, and outcome variables.
All 22 patients received amphotericin-based regimens for the treatment of pre-transplant IPA. Patient characteristics are shown in Table 1. The median follow-up period was 577 days (range, 31-2,538 days). Mean age was 37.5 years (range, 15-62 years). Primary diseases included 19 cases of acute leukemia (16 AML [84%] and 3 acute biphenotypic leukemia) and 3 cases of other malignancies (1 case of myelodysplastic syndrome, 1 of chronic myelomonocytic leukemia, and 1 of T-cell lymphoblastic lymphoma). Fourteen of the donors were related and 8 were unrelated. Twenty-one of the cases were HLA-well matched and one was mismatched. Peripheral blood stem cells (N=14), bone marrow (N=7), and umbilical cord blood (N=1) were used as the source of stem cells. Patients were conditioned with high-dose total body irradiation (TBI)-based (N=8) or non-TBI-based (N=9) conventional regimens or with nonmyeloablative regimens (N=5). Disease status at the time of the HSCT consisted of 14 cases in complete remission (CR) and 8 not in CR.
Pre-transplantation IPA characteristics are presented in Table 2. Time from treatment of IPA to HSCT was classified into <60 days (N=6), 60-120 days (N=9), and ≥120 days (N=7); median duration was estimated as 95 days (range, 13-284 days). Diagnosis of IPA was conducted according to the EORTC/MSG criteria, and defined as proven (N=5), probable (N=0), or possible (N=17). Chest CT findings were defined as major findings (N=10) or non-major findings (N=12), and they included ground glass opacity, nodules, or consolidation with or without halo sign. Cavitating infiltrates were observed in 1 case (5%) and pleural effusion was observed in 4 (23%) cases. The Aspergillus antigen test for detecting the galactomannan antigen in serum was performed in 5 cases, and was positive in 2 of these cases (40%). The duration of treatment with antifungal agents before HSCT was classified as <30 days (N=11) or >30 days (N=11), with a median of 64 days (range, 9-242 days). Three patients underwent additional surgical resection. At the time of the HSCT, all cases were in an overall responsive state to the IPA treatment, except for 1 case that was in a progressive state.
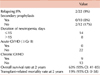
Transplantation outcomes are shown in Table 3. Secondary antifungal prophylaxis was administered to 10 patients during HSCT as follows: itraconazole (N=6), amphotericin B (AmB) (N=3), or caspofungin (N=1). Two of the patients who did not receive secondary prophylaxis relapsed. Duration of neutropenia was classified into ≤15 days (N=14) or >15 days (N=8). No acute GVHD (≥Gr II) was observed. The development of post-transplant IPA was noted in 2 patients at days 61 and 315 following HSCT, respectively. One of these patients died of septic shock within 2 days of the diagnosis of possible IPA. The other patient recovered from IPA but eventually relapsed. Neither case had received anti-fungal prophylaxis during HSCT. The overall 2-year survival rate of the 22 patients was 63% (95% CI: 41-85), with a TRM rate of 19% (95% CI: 0-38).
The control of IPA is a critical element for the success of an HSCT. Antifungal therapy should be initiated early on in patients with suspected invasive aspergillosis, and in some cases, concurrently with the diagnostic evaluation [17]. Historically, AmB, which is an ergosterol-binding polyene involved in the disintegration of the fungal membrane, has been the major antifungal drug used in patients with invasive aspergillosis. In our retrospective study, all 22 patients received amphotericin-based regimens for the treatment of pre-transplant IPA. Recent drug development has shown that lipid-bound formulations of AmB exhibit the same microbiological activities and are also well-tolerated. Therefore, voriconazole is currently considered the drug of choice for the treatment of IA [17]. Despite the subsequent profound bone marrow suppression, positive outcomes are increasingly being achieved with the early and aggressive surgical management of IPA [18]. One study examined 6 patients aged 2-15 years old who developed significant fungal infection of the lungs before or after undergoing bone marrow transplant [19]. Survival following bone marrow transplant was achieved for 6 and 11 months in patients who underwent lung resection before the transplant, and for 24, 30, 39, and 60 days in patients who underwent lung resection after the transplant. In our study, 3 patients underwent additional surgical resection before the HSCT, and IPA did not recur after HSCT in these patients.
Antifungal therapy should be continued until all signs and symptoms of infection have remained resolved for at least 2 weeks. Chest radiography, if initially abnormal, should be stabilized, and signs of active infection must have disappeared. For most immunosuppressed patients, antifungal therapy is continued for months. In the present study, the duration of treatment with antifungal agents before HSCT was either less than 30 days (N=11) or more than 30 days (N=11), with a median duration of 64 days (range, 9-242 days). Antifungal therapy was continued for 10 and 33 days for each of the 2 patients who developed post-transplant IPA, respectively.
No previous studies have examined the effectiveness of secondary antifungal prophylaxis in preventing IA relapse. In this study, 10 patients received secondary antifungal prophylaxis during HSCT as follows: itraconazole (N=6), AmB (N=3), or caspofungin (N=1). Due to the high risk of relapse reported in multiple studies, reinitiation of antifungal therapy using voriconazole is usually recommended during chemotherapy and from the onset of the conditioning regimen until transplant engraftment [20]. However, we do not use routine secondary antifungal prophylaxis at our institution. The development of post-transplant IPA was observed in 2 of the patients on day 61 and 315 after HSCT, respectively. One of these patients died of septic shock within 2 days of diagnosis of possible IPA. The other patient recovered from IPA but eventually experienced relapse of the primary disease. It is important to note that neither case had received anti-fungal prophylaxis during HSCT; the risk of IPA was significantly lower in patients who received secondary prophylaxis (P<0.05). This indicates that reinitiation of antifungal therapy during HSCT should be considered.
In this study, the overall 2-year survival rate of the 22 patients was 63% (95% CI: 41-85), and the TRM rate was 19% (95% CI: 0-38). This result suggests that a history of IPA prior to HSCT does not have an adverse impact on transplant outcomes or on IPA recurrence. In 2004, a retrospective study evaluated the outcomes of a first allogeneic HSCT among a large cohort of patients (N=2,319) with and without a known history of IA before transplantation. The probability of developing post-transplant IA and the overall survival rates were not different between patients who received >1 month of antifungal therapy and had radiographic abnormalities, and patients with no history of IA (13% vs. 10%, respectively, P=0.65; 52% vs. 58%, respectively, P=0.47) [11]. Another study involved 13 patients (7 males and 6 females) who had hematologic malignancies with a high risk of relapse or severe aplastic anemia, 11 (73%) of whom underwent 15 HSCTs with active IFIs between September 2003 and April 2007. After a median follow-up period of 306 days (range, 145-680 days), 4 of the 13 (31%) patients with active IFIs were alive and healthy. Therefore, within a sample of HSCT recipients with dismal prognoses without transplantation, performing the procedure despite active IFIs saved a considerable proportion of the patients. This indicated that the presence of active IFIs is not an absolute contraindication to HSCT, particularly among high-risk patients for whom a delay in treatment could be fatal [21]. These results suggest that despite a history of IPA, the rate of fungal infection after HSCT is not higher when prior IPA has been adequately controlled.
However, this study had several limitations. First, this was a single-center, retrospective, and non-randomized study. Second, this study was limited by its small sample size, which is an inherent problem when studying rare diseases such as IPA.
In conclusion, this study demonstrates that a history of IPA prior to HSCT does not have adverse impacts on transplant outcomes (including IPA recurrence) in cases where prior IPA was appropriately controlled. Our results indicate that a history of IA is not an absolute contraindication to allogeneic HSCT, especially if adequate therapies are administered before transplantation. Early and aggressive surgical management of IPA before transplantation should also be considered. Furthermore, reinitiation of antifungal therapy during transplantation should be considered.
Figures and Tables
References
1. Russell N, Bessell E, Stainer C, Haynes A, Das-Gupta E, Byrne J. Allogeneic haemopoietic stem cell transplantation for multiple myeloma or plasma cell leukaemia using fractionated total body radiation and high-dose melphalan conditioning. Acta Oncol. 2000. 39:837–841.

3. Marr KA, Carter RA, Boeckh M, Martin P, Corey L. Invasive aspergillosis in allogeneic stem cell transplant recipients: changes in epidemiology and risk factors. Blood. 2002. 100:4358–4366.

4. Lin SJ, Schranz J, Teutsch SM. Aspergillosis case-fatality rate: systematic review of the literature. Clin Infect Dis. 2001. 32:358–366.

5. Nicod LP, Pache JC, Howarth N. Fungal infections in transplant recipients. Eur Respir J. 2001. 17:133–140.

6. Wald A, Leisenring W, van Burik JA, Bowden RA. Epidemiology of Aspergillus infections in a large cohort of patients undergoing bone marrow transplantation. J Infect Dis. 1997. 175:1459–1466.

7. Post MJ, Lass-Floerl C, Gastl G, Nachbaur D. Invasive fungal infections in allogeneic and autologous stem cell transplant recipients: a single-center study of 166 transplanted patients. Transpl Infect Dis. 2007. 9:189–195.

8. Wang ZY, Jiang EL, Zhang P, et al. Invasive fungal infections after allogeneic hematopoietic stem cell transplantation and related risk factors. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2008. 16:618–622.
9. Hovi L, Saarinen-Pihkala UM, Vettenranta K, Saxen H. Invasive fungal infections in pediatric bone marrow transplant recipients: single center experience of 10 years. Bone Marrow Transplant. 2000. 26:999–1004.

10. Subirà M, Martino R, Franquet T, et al. Invasive pulmonary aspergillosis in patients with hematologic malignancies: survival and prognostic factors. Haematologica. 2002. 87:528–534.
11. Fukuda T, Boeckh M, Guthrie KA, et al. Invasive aspergillosis before allogeneic hematopoietic stem cell transplantation: 10-year experience at a single transplant center. Biol Blood Marrow Transplant. 2004. 10:494–503.

12. Richard C, Romón I, Baro J, et al. Invasive pulmonary aspergillosis prior to BMT in acute leukemia patients does not predict a poor outcome. Bone Marrow Transplant. 1993. 12:237–241.
13. Vaidya SJ, Ortín M, López-Duarte M, et al. Haemopoietic progenitor cell transplantation in patients with previous history of invasive fungal infection. Leuk Lymphoma. 2005. 46:1143–1150.

14. Avivi I, Oren I, Haddad N, Rowe JM, Dann EJ. Stem cell transplantation post invasive fungal infection is a feasible task. Am J Hematol. 2004. 75:6–11.

15. Hoover M, Morgan ER, Kletzel M. Prior fungal infection is not a contraindication to bone marrow transplant in patients with acute leukemia. Med Pediatr Oncol. 1997. 28:268–273.

16. De Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008. 46:1813–1821.

17. Walsh TJ, Anaissie EJ, Denning DW, et al. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008. 46:327–360.

18. Salerno CT, Ouyang DW, Pederson TS, et al. Surgical therapy for pulmonary aspergillosis in immunocompromised patients. Ann Thorac Surg. 1998. 65:1415–1419.

19. Lupinetti FM, Behrendt DM, Giller RH, Trigg ME, de Alarcon P. Pulmonary resection for fungal infection in children undergoing bone marrow transplantation. J Thorac Cardiovasc Surg. 1992. 104:684–687.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download