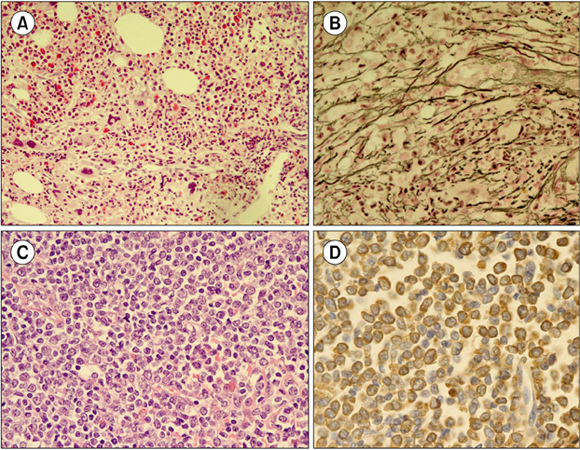
A 54-year-old man was referred to our hospital with right flank pain. Three years ago, he was diagnosed with gastric mucosa-associated lymphoid tissue (MALT) lymphoma and successfully treated with radiotherapy. CBC showed a WBC count of 24.12×109/L (70% neutrophil, 14% lymphocyte, 4% monocyte, 2% eosinophil, 1% basophil, 4% metamyelocyte, 5% myelocyte, and 1/100 WBCs normoblast); Hb level, 10.2 g/dL; and platelet count, 416×109/L. Bone marrow (BM) examination showed granulocytic and megakaryocytic proliferation with moderate dysplastic megakaryopoiesis (A; H&E stain, ×200), and diffuse reticulin fibrosis (B; reticulin stain, ×400). Primary myelofibrosis was the first diagnostic consideration after BM study. Chromosomal analysis, however, showed t(9;22)(q34;q11.2), indicating CML. Concurrent abdomen computerized tomography revealed enlarged inguinal lymph nodes. Inguinal lymph node biopsy showed diffuse infiltration of immature cells (C; H&E stain, ×400), which were positive for myeloperoxidase (D). BCR/ABL1 rearrangement was demonstrated by fluorescence in-situ hybridization analysis, and a diagnosis of granulocytic sarcoma (GS) was made. Accompanying extramedullary myeloid tumor, CML was classified as blastic phase. Secondary CML with a simultaneous manifestation of GS is rare. Combining morphological and molecular-cytogenetic approaches can help detect the coexistence of both neoplasms, especially in CML cases with fewer typical morphologic features.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download