Abstract
Background
This study evaluates the effectiveness of immunochemotherapy and radiation therapy in the treatment of patients with primary bone lymphoma (PBL).
Methods
We retrospectively reviewed the medical records of 33 patients with PBL who were treated at 6 medical centers in Korea from 1992 to 2010. Clinicopathological features and treatment outcomes were analyzed.
Results
The median age of the patients participating in our study was 40 years. The most common sites of involvement were the pelvis (12.36%) and femur (11.33%). CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) or CHOP-like regimens were administered to 20 patients (61%), and R-CHOP (rituximab plus CHOP) was administered to the remaining 13 patients (39%). The overall response rate was 89% (complete response, 76%; partial response, 12%). The overall survival (OS) of patients with solitary bone lesions was longer than that of patients with multiple bone lesions (median OS: not reached vs. 166 months, respectively; P=0.089). Addition of rituximab to CHOP did not significantly affect either OS or progression-free survival (P=0.53 and P=0.23, respectively). Combining radiation therapy with chemotherapy also did not improve the OS or progression-free survival of patients with solitary bone lesions.
Conclusion
Conventional cytotoxic chemotherapy remains an effective treatment option for patients with PBL. Additional benefits of supplementing chemotherapy with either rituximab or radiation therapy were not observed in this study. Further investigation is needed to characterize the role of immunochemotherapy in treating patients with PBL.
Primary bone lymphoma (PBL) is a rare disease, accounting for only 7% of primary bone malignancies and approximately 5% of extranodal non-Hodgkin lymphomas (NHLs). PBL represents <2% of all lymphomas in adults [1]. PBL was first described by Oberling in 1928 and was later defined as a separate clinical entity in 1939, following the publication of a 17-case series by Parker and Jackson.
Traditionally, PBL was defined as lymphoma localized to the bone without evidence of soft tissue or nodal involvement. In this study, diagnosis of PBL was based on the 2002 World Health Organization classification of tumors of soft tissue and bone [2]. Hence, positive diagnosis was defined by the presence of either a single bone lesion, with or without regional lymph node (LN) involvement, or a multiple bone lesion, without visceral or LN involvement.
According to the World Health Organization classification, the most common histopathological subtype of PBL is diffuse large B-cell lymphoma (DLBCL) [3]. Initial diagnosis of PBL can be challenging due to nonspecific symptoms and ambiguous radiological results. Furthermore, standard treatment regimens have not yet been established because of the low incidence rates of PBL. Prior to the availability of effective chemotherapeutic drugs, PBL was treated with radiation therapy (RT) or surgery. Since introducing cytotoxic agents as treatment options for PBL, several studies have established that chemotherapy combined with RT is better than RT alone [1, 4]. However, some recently published studies have reported that no differences were observed between the overall survival (OS) of patients treated with chemotherapy alone and those given a combination of chemotherapy and RT, although the number of cases involved in these studies was too low to achieve statistical significance. Other reports have suggested that patients treated with rituximab-based chemotherapy have improved survival rates [5]. Rituximab, a monoclonal antibody directed against the CD20 antigen expressed on lymphocytes, was approved by the US Food and Drug Administration for the treatment of B-cell NHL in 1997. Multiple randomized trials have shown that the addition of rituximab to chemotherapy regimens improves outcomes in patients with aggressive non-osseous NHL [6-9]. One retrospective analysis of PBL showed that the addition of rituximab to chemotherapy improved the progression-free survival (PFS) but not the OS [2]. However, the roles of rituximab and RT in the treatment of patients with PBL have not been established thus far. The present study aimed at examining the clinical characteristics of PBL among Korean patients and assessing the outcomes of different treatment options, including rituximab-based regimens.
We retrospectively included patients who were diagnosed with PBL at 6 medical centers in Korea, between 1992 and 2010. Clinical data retrieved from medical records were analyzed. PBL was defined as lymphoma with solitary bone lesions with or without LN involvement, or multiple bone lesions without LN, visceral, or bone marrow involvement.
Only patients with DLBCL, confirmed by histological examination, were included. Patients with bone marrow involvement or other histological diagnoses such as anaplastic large cell lymphoma, Burkitt lymphoma, Hodgkin lymphoma, and lymphoplasmacytic lymphoma were excluded from this study.
All participating patients' medical records were reviewed, and the treatment outcomes were noted, including response to treatment and survival. Clinicopathological features were also analyzed, including age at diagnosis, sex, stage, International Prognostic Index (IPI), Eastern Cooperative Oncology Group (ECOG) performance status, histological diagnosis, site of disease, number of bone sites involved (solitary vs. multiple bone involvements), type of treatment, and dates of the last follow-up visit and of the patient's death. Clinical staging was determined according to the Ann Arbor Staging System [10], using contrast-enhanced computed tomographic scans of the neck, chest, abdomen, and pelvis and, in most cases, using magnetic resonance imaging (MRI) results of the affected area. Stage I and II were defined by the presence of a single skeletal tumor without or with regional LN involvement (IE or IIE, respectively), and stage IV was defined by the presence of multiple bone lesions without visceral, LN, or bone marrow involvement. Stage I or II PBLs were described as IE or IIE to indicate the involvement of an extralymphatic organ, referring to primary bone involvement.
Treatment response was assessed using the International Working Group response criteria [11] or the revised response criteria [12], for pre-positron emission tomography and post-positron emission tomography data, respectively. In addition, criteria proposed by a Miami University group were applied to clarify any ambiguity in the results obtained using imaging techniques [5]. OS was defined as the period extending from the date of PBL diagnosis to the date of the last follow-up visit, or the date of death from any cause. PFS was defined as the period extending from the date of treatment initiation to the date of documented disease progression, or the date of death caused by the disease itself or by treatment toxicity.
Statistical analysis of the data was performed using SPSS version 14.0 for Windows (SPSS, Chicago, IL). The χ2 test was used to compare frequencies between the 2 subgroups subjected to different treatment modalities. Survival curves were constructed based on the Kaplan and Meier method and compared using the log-rank test. The Cox proportional hazard model was used to identify the prognostic factors associated with OS and PFS. A 2-sided P<0.05 was considered statistically significant.
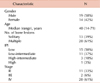
This study included a total of 33 patients with primary DLBCL of the bone; the participating patients' demographic characteristics are presented in Table 1. The median age was 40 years (range, 14-71 years). Nineteen patients (58%) were men, and 14 (42%) were women. The most common sites of involvement were the pelvis (13.39%), femur (11.33%), and ribs (8.24%) (Table 2). At the time of presentation, 13 patients (39%) had tumors involving a single bone, and 20 patients (61%) had multisite lesions. Clinical stage varied among patients, such that 11 patients (33%) were at stage IE, 2 (6%) at stage IIE, and 20 at stage IV (61%) of the disease.
Of the 33 patients, 16 (48%) were initially treated with chemotherapy alone, and 17 (52%) with chemotherapy and RT. No patients in our study were treated with RT alone. While the majority of patients with solitary bone lesions underwent combined modality treatment (70%), patients with multiple bone lesions were predominantly treated with chemotherapy alone (60%). All patients received anthracycline-containing regimens such as CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), with or without rituximab, and the median number of chemotherapy cycles was 6 (range, 2-8). R-CHOP (rituximab plus CHOP) was administered to 4 patients (31%) with solitary bone lesions, and to 9 patients (45%) with multiple bone lesions. Combined modality treatment was administered to 17 patients (52%), and consisted of chemotherapy that was followed by RT in most cases (15 patients). The median radiation dose was 4,500 cGy (range, 3,000-5,600 cGy) (Table 3).
Of the 33 patients who were treated with chemotherapy, with or without radiation, 24 (76%) achieved complete response (CR) and 4 (12%) achieved partial response (PR). The overall response rate (ORR) following treatment was 88% (95% confidence interval [CI]: 73-97). Eight of the 24 patients who had achieved CR experienced relapse during the follow-up period. The relapse rate was 34%, and the median time to relapse was 87 months (95% CI: 61-114). No differences in ORR and CR rates were observed between patients who had received R-CHOP and those who had received CHOP (85% and 77% vs. 90% and 75%, respectively; P=0.64).
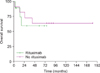
The median OS was 166 months (95% CI: 0-339). The Kaplan-Meier curve of OS of patients with PBL exhibited a downward-sloping curve for a 4-year period, before reaching a plateau (Fig. 1). Longer OS was generally observed among patients with solitary bone lesions than that among those with multiple bone lesions (median OS: not reached vs. 166 months, respectively; P=0.089; Fig. 2). No significant difference in OS was observed between patients treated with chemotherapy alone and those treated with chemotherapy followed by RT (median OS: 87 months vs. not reached, respectively; P=0.69). Addition of rituximab to CHOP did not result in significant improvement to OS and PFS (P=0.53 and P=0.237, respectively). Supplementing chemotherapy with RT also did not affect OS and PFS in patients with multiple bone lesions (data not shown) and patients with solitary bone lesions (Fig. 3). Moreover, OS and PFS were not significantly affected by the addition of rituximab to the treatment regimens in patients with advanced PBL (Fig. 4) and patients with limited disease (data not shown).
PBL is a rare subtype of NHL. Therefore, owing to its low incidence rates, specific therapeutic guidelines for PBL treatment have not yet been established. Therapeutic options include surgery, RT, chemotherapy, or chemoradiation. Prior to the use of chemotherapy as treatment, PBL was treated using radiation or surgery. However, the role of surgery in PBL should be limited to biopsies, bone fracture repair, or disease control in selected patients with low-grade lymphomas who cannot tolerate additional therapeutic interventions because of other medical conditions.
In the 1960s, RT was established as the standard PBL treatment method, with reported cure rates ranging from 44% to 63% [13-15]. However, despite relatively high CR rates following RT alone, relapse in regions outside the radiation field was commonly observed. Therefore, although radiation provides excellent local control, systemic therapy is needed to prevent recurrence outside the radiation portal [13-15].
While some studies have established that combined modality treatment consisting of chemotherapy and RT provides a superior outcome to RT alone [16], other studies have failed to demonstrate such a significant advantage of combined modality over RT alone [1]. Recently, clinical outcomes of patients treated with immunochemotherapy such as rituximab have been reported [5]. However, no study has yet reported the detailed treatment response characteristics of PBL patients treated with rituximab-containing regimens in Korea. In the present study, we observed that most PBL cases characteristically exhibited male predominance and had a younger median age (40 years) than nodal DLBCL cases [17], which is consistent with previously published studies. On the other hand, previous reports had established that the most common site of involvement was the femur, followed by the pelvis, fibular or tibia, humerus, and spine, in descending order of frequency. However, according to our study, the pelvic bone was the most common involvement site [1, 18].
It is difficult to diagnose PBL and monitor response to treatment using simple imaging techniques such as radiography. Indeed, initial radiographs of patients with PBL may sometimes appear normal, while subsequent examination using bone scans or MRI would detect abnormalities. Therefore, conventional radiography has limited value in the diagnosis of PBL. Moreover, gallium scans, MRI, and positron emission tomography may falsely indicate activity following therapy due to bone remodeling [4], which further complicates the assessment of treatment response. Previous studies have associated certain factors with the survival rates of patients with PBL. The number of bones involved (single vs. multiple) has been established as the main prognostic factor and was demonstrated as such in a large-scale study (422 patients) conducted by Ostrowski et al. [19] In addition, Ramadan et al. and Catlett et al. [2, 20] demonstrated the association of high IPI scores with significantly worse patient outcomes. In the present study, our results confirm that the number of bones involved significantly affects the OS rates (P=0.089, Fig. 2), which is consistent with previous observations.
The effects of different treatment modalities on patients with PBL have not been determined. However, several studies have established that chemotherapy is essential for successful treatment of PBL [21-23]. Moreover, Alencar et al. suggested that the addition of rituximab to chemotherapy regimens has a beneficial effect on the survival of patients with PBL [5]. However, our results showed that the addition of rituximab to the treatment regimen did not significantly affect the OS of patients who underwent chemotherapy alone or the OS of patients who were given a combined modality treatment of chemotherapy and RT. Furthermore, our results demonstrated that the Ann Arbor stage, ECOG performance status, and IPI score were not associated with patient outcomes, which is consistent with the Miami University report [5].
Our study has several limitations. First, the small number of patients included in the study made it difficult to achieve statistically significant results. Second, the retrospective nature of our analysis compromised the analysis of different clinical outcomes between the subgroups. This study faced the inherent challenges of studying such a rare disease. Nevertheless, to our knowledge, this is the first study that investigates the role of immunochemotherapy in the treatment of PBL patients in Korea. Moreover, it is among the largest case series studies on PBL that have ever been conducted. While this study failed to demonstrate the beneficial effects of supplementing standard chemotherapy regimens with either RT or rituximab, it confirmed that conventional cytotoxic chemotherapy is a successful treatment option for patients with PBL. Further investigation is required to characterize the role of immunochemotherapy in treating patients with PBL.
Figures and Tables
 | Fig. 1Overall survival of all participating patients with primary bone lymphoma (median overall survival: 166 months, 95% CI: 0-339). |
 | Fig. 2Survival by number of bones involved. (A) Overall survival (OS) of patients with solitary bone lesions compared to that of patients with multiple bone lesions (median OS: not reached vs. 166 months, P=0.089) and (B) Progression-free survival (PFS) of patients with solitary bone lesions compared to that of patients with multiple bone lesions (median PFS: 74 months vs. 74 months, P=0.99). |
 | Fig. 3Progression-free survival of patients with solitary bone lesions treated with radiation therapy (Median progression-free survival: 74 months vs. 87 months, P=0.78). Abbreviation: RT, radiation therapy. |
References
1. Dubey P, Ha CS, Besa PC, et al. Localized primary malignant lymphoma of bone. Int J Radiat Oncol Biol Phys. 1997. 37:1087–1093.

2. Ramadan KM, Shenkier T, Sehn LH, Gascoyne RD, Connors JM. A clinicopathological retrospective study of 131 patients with primary bone lymphoma: a population-based study of successively treated cohorts from the British Columbia Cancer Agency. Ann Oncol. 2007. 18:129–135.

3. Jaffe ES. The 2008 WHO classification of lymphomas: implications for clinical practice and translational research. Hematology Am Soc Hematol Educ Program. 2009. 523–531.

4. Baar J, Burkes RL, Gospodarowicz M. Primary non-Hodgkin's lymphoma of bone. Semin Oncol. 1999. 26:270–275.
5. Alencar A, Pitcher D, Byrne G, Lossos IS. Primary bone lymphoma-the University of Miami experience. Leuk Lymphoma. 2010. 51:39–49.
6. Coiffier B, Lepage E, Briere J, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med. 2002. 346:235–242.

7. Feugier P, Van Hoof A, Sebban C, et al. Long-term results of the R-CHOP study in the treatment of elderly patients with diffuse large B-cell lymphoma: a study by the Groupe d'Etude des Lymphomes de l'Adulte. J Clin Oncol. 2005. 23:4117–4126.

8. Sehn LH, Donaldson J, Chhanabhai M, et al. Introduction of combined CHOP plus rituximab therapy dramatically improved outcome of diffuse large B-cell lymphoma in British Columbia. J Clin Oncol. 2005. 23:5027–5033.

9. Pfreundschuh M, Trümper L, Osterborg A, et al. CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good-prognosis diffuse large-B-cell lymphoma: a randomised controlled trial by the MabThera International Trial (MInT) Group. Lancet Oncol. 2006. 7:379–391.
10. Carbone PP, Kaplan HS, Musshoff K, Smithers DW, Tubiana M. Report of the committee on Hodgkin's disease staging classification. Cancer Res. 1971. 31:1860–1861.
11. Cheson BD, Horning SJ, Coiffier B, et al. NCI Sponsored International Working Group. Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. J Clin Oncol. 1999. 17:1244.

12. Cheson BD, Pfistner B, Juweid ME, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007. 25:579–586.

13. Fidias P, Spiro I, Sobczak ML, et al. Long-term results of combined modality therapy in primary bone lymphomas. Int J Radiat Oncol Biol Phys. 1999. 45:1213–1218.

14. Fairbanks RK, Bonner JA, Inwards CY, et al. Treatment of stage IE primary lymphoma of bone. Int J Radiat Oncol Biol Phys. 1994. 28:363–372.

15. Marshall DT, Amdur RJ, Scarborough MT, Mendenhall NP, Virkus WW. Stage IE primary non-Hodgkin's lymphoma of bone. Clin Orthop Relat Res. 2002. 405:216–222.

16. Fidias P, Spiro I, Sobczak ML, et al. Long-term results of combined modality therapy in primary bone lymphomas. Int J Radiat Oncol Biol Phys. 1999. 45:1213–1218.

17. López-Guillermo A, Colomo L, Jiménez M, et al. Diffuse large B-cell lymphoma: clinical and biological characterization and outcome according to the nodal or extranodal primary origin. J Clin Oncol. 2005. 23:2797–2804.

18. Heyning FH, Hogendoorn PC, Kramer MH, et al. Primary non-Hodgkin's lymphoma of bone: a clinicopathological investigation of 60 cases. Leukemia. 1999. 13:2094–2098.

20. Catlett JP, Williams SA, O'Connor SC, Krishnan J, Malkovska V. Primary lymphoma of bone: an institutional experience. Leuk Lymphoma. 2008. 49:2125–2132.

21. Nissen NI, Ersbøll J, Hansen HS, et al. A randomized study of radiotherapy versus radiotherapy plus chemotherapy in stage I-II non-Hodgkin's lymphomas. Cancer. 1983. 52:1–7.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download