Abstract
Chronic graft versus host disease (GVHD) is a frequent complication after allogeneic hematopoietic stem cell transplantation (HSCT), but simultaneous small bowel obstruction is rare. Here, we report a child with acute myeloid leukemia who received an allogeneic HSCT from an unrelated matched donor. After HSCT, the patient developed severe chronic GVHD involving the small intestine, leading to obstruction of the terminal ileum. Small bowel resection was performed, and the symptoms improved without severe complications. Bowel obstruction should be considered as a possible complication of chronic GVHD; surgery may be a valuable corrective measure.
Chronic graft versus host disease (GVHD) is a serious long-term complication of allogeneic hematopoietic stem cell transplantation (HSCT). Chronic GVHD can occur any time after allogeneic HSCT but is most common within the first 3 years. It shares features common to both autoimmune and immunodeficiency disorders [1]. Chronic GVHD is usually treated with immunosuppressive agents, such as cyclosporine, corticosteroids, and tacrolimus/mycophenolate mofetil (MMF) [2]. Nevertheless, the prognosis of chronic GVHD is poor, and the 10-year survival rate was estimated to be 42% (95% confidence interval [Cl], 29-54%) [3].
Common clinical findings of chronic GVHD include skin changes, abnormal liver biochemistry, oral mucositis, oral and ocular sicca, esophagitis, and polyserositis. Although extremely rare, small bowel obstruction caused by severe chronic intestinal GVHD has also been reported [4-6].
In this case, the patient had sustained abdominal pain and ileus while exhibiting general improvement in other organs. A gastrointestinal contrast study indicated small bowel obstruction, and surgery was performed. Successful symptom relief occurred after resection of the obstructed bowel.
The study was performed after the approval by the SNUH institutional review board (IRB; No. E-1108-106-375). A 22-month-old girl was diagnosed with acute myeloid leukemia. She received induction chemotherapy with enocitabine (300 mg/m2 by intravenous [IV] administration for 10 days), idarubicin (10 mg/m2 by IV administration for 3 days), cytarabine (30 mg by intrathecal injection for 1 day), and 6-thioguanine (100 mg/m2 orally for 10 days) [6]. She achieved complete remission, and after 3 cycles of consolidation chemotherapy, she received an allogeneic peripheral stem cell transplantation from a sex-mismatched but fully HLA-matched unrelated donor. The mean dose of cells infused was 34.7×108/kg for total nucleated cells, 29.8×108/kg for mononuclear cells, and 33.6×106/kg for CD34+ cells. The conditioning regimen comprised busulfan (0.8 mg/kg by IV administration for 4 days), fludarabine (40 mg/m2 by IV administration for 6 days), and anti-thymocyte globulin (ATG) (2.5 mg/kg by IV administration for 3 days). Tacrolimus and short-course methotrexate were administered for GVHD prophylaxis. Tacrolimus was started 2 days before stem cell infusion (continuous IV infusions at 0.03 mg/kg/day), and MTX was started 1 day after stem cell infusion (IV administration at 15 mg/m2). On day 12 of transplantation, the absolute neutrophil count (ANC) rose above 1.0×109/L (3.8×109/L), and the platelet count was 121×109/L. The patient was discharged on day 19 without any symptoms or signs of acute GVHD.
On day 138, the patient was admitted to the hospital for persistent cough for more than 1 week. Chest computed tomography (CT) showed diffuse interstitial infiltration (Fig. 1). Piperacillin/tazobactam, ganciclovir, and sulfamethoxazole/trimethoprim were administered for the treatment of pneumonia. Laboratory examination revealed elevated levels of liver enzymes (AST, 206 IU/L; ALT, 243 IU/L). Blood culture, urine culture, blood Epstein-Barr virus (EBV) antibody, blood cytomegalovirus (CMV) antigen, and nasopharyngeal aspiration respiratory viral study were all negative. After admission, the patient's cough subsided, and the findings on chest radiograph improved, but the patient developed a fever on day 145 followed by a skin rash on the whole body and hematochezia on day 147. The liver enzyme levels showed persistent elevation, and the total bilirubin level also began to rise, peaking at 2.9 mg/dL on day 146. A skin biopsy was performed; pathological examination revealed interface vacuolar change with several dyskeratotic cells consistent with chronic GVHD. Liver biopsy revealed lymphocytic/eosinophilic infiltration in the portal triad with diffuse bile duct damage, and focal crypt atrophy was shown on colon biopsy specimens, which are consistent with chronic GVHD. Treatment for chronic GVHD with prednisolone (Pd) and cyclosporine A (CsA) was started on day 163.
A CMV antigenemia assay performed on day 175 was positive, indicating CMV infection. Therefore, ganciclovir therapy was initiated. The colon biopsy specimen tested negative for CMV infection.
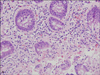
Because of persistent diarrhea and hyperbilirubinemia (total bilirubin, 11.1 mg/dL; direct bilirubin, 5.9 mg/dL), a salvage regimen for chronic GVHD with tacrolimus/MMF and Pd was started on day 182. Hematochezia increased; therefore, a bleeding scan was performed on day 214. However, no bleeding focus was identified. Hematochezia subsided, and the total bilirubin level returned to near normal by day 260, but abdominal pain and ileus persisted. Therefore, an upper gastrointestinal and small bowel contrast study was performed. The result showed narrowing and partial obstruction of the proximal-to-distal small bowel (Fig. 2), and small bowel resection was performed on day 270. During laparotomy, diffuse constriction was observed in the terminal ileum (Fig. 3). The results of pathological examination were consistent with chronic GVHD, showing severe loss of mucosal epithelium, many basal single cell apoptotic bodies, crypt dropout, and submucosal/subserosal fibrosis (Fig. 4).
Following laparotomy, abdominal pain and diarrhea subsided. Oral feeding was initiated on day 276 (postoperative day 6), and the patient's oral intake increased successfully. Liver enzymes, total normalized bilirubin, and chest radiograph findings also improved. The patient was discharged on day 290. The patient continued MMF therapy until day 378 and tacrolimus therapy until day 638. She has been disease-free for 4 years after HSCT. She is not taking medications other than vitamin B12 and does not have gastrointestinal problems.
Here, we reported a rare case of severe chronic intestinal GVHD that caused small bowel obstruction despite aggressive immunosuppression. This case demonstrates that surgery can successfully treat such conditions.
Gastrointestinal complications are common after HSCT. Other common post-transplant gastrointestinal complications include mucositis (90%), vomiting (85%), and abdominal pain (71%) [8]. The incidence of acute intestinal GVHD was 33% in a cohort of 89 patients undergoing allogeneic bone marrow transplantation [9]. Acute intestinal GVHD usually manifests as abdominal pain and diarrhea and rarely leads to intestinal stricture [10]. Damage to the intestinal mucosa may stimulate an inflammatory response that can induce or amplify the cytokine cascade involved in acute intestinal GVHD [9].
Gastrointestinal complications are common in chronic GVHD. If esophageal web or stricture/stenosis is present in the upper to middle third of the esophagus, a diagnosis of chronic GVHD is appropriate. Common gastrointestinal symptoms of chronic GVHD include anorexia, nausea, vomiting, diarrhea, weight loss, and failure to thrive [11].
Although extremely rare, cases of bowel obstruction resulting from chronic GVHD have been reported. Evans et al. [6] reported a 35-year-old man who underwent small bowel resection and multiple strictureplasties for chronic intestinal GVHD and remained asymptomatic for 24 months after surgery. Herr et al. [4] reported 2 patients who underwent surgery for chronic intestinal GVHD because of persistent obstructive symptoms; one patient remained asymptomatic for 32 months after transplant, and the other developed leakage of stricturoplasty and peritonitis. For pediatric cases, Spencer et al. [5] reported the case of a 12-year-old child with aplastic anemia who underwent small bowel resection 207 days after HSCT and later died of cardiac arrest on postoperative day 1. No other pediatric cases of chronic GVHD with small bowel obstruction have been reported previously, and our patient is the youngest case reported.
In conclusion, bowel obstruction should be considered a possible complication related to chronic GVHD in patients with persistent abdominal pain and ileus despite general symptomatic improvement. Furthermore, surgery should be considered for complications of intestinal GVHD those do not respond to medical therapy. Since the outcome of surgical treatment is uncertain, it should be performed with caution and consideration of both the associated benefits and risks.
Figures and Tables
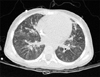 | Fig. 1Chest CT image obtained on day 138 shows multifocal subsegmental atelectasis and increased interstitial marking. |
 | Fig. 2Ten hours after upper GI contrast study on day 264. Luminal narrowing of the small bowel with dilatation of the proximal bowel can be seen. |
References
1. Toubai T, Sun Y, Reddy P. GVHD pathophysiology: is acute different from chronic? Best Pract Res Clin Haematol. 2008. 21:101–117.

2. Takatsuka H, Iwasaki T, Okamoto T, Kakishita E. Intestinal graft-versus-host disease: mechanisms and management. Drugs. 2003. 63:1–15.
3. Wingard JR, Piantadosi S, Vogelsang GB, et al. Predictors of death from chronic graft-versus-host disease after bone marrow transplantation. Blood. 1989. 74:1428–1435.

4. Herr AL, Latulippe JF, Carignan S, Mitchell A, Belanger R, Roy J. Is severe intestinal chronic graft-versus-host disease an indication for surgery? A report of two cases. Transplantation. 2004. 77:1617–1620.

5. Spencer GD, Shulman HM, Myerson D, Thomas ED, McDonald GB. Diffuse intestinal ulceration after marrow transplantation: a clinicopathologic study of 13 patients. Hum Pathol. 1986. 17:621–633.

6. Evans J, Percy J, Eckstein R, Ma D, Schnitzler M. Surgery for intestinal graft-versus-host disease: report of two cases. Dis Colon Rectum. 1998. 41:1573–1576.
7. Park HS, Kim DW, Kim CC, et al. Induction chemotherapy with idarubicin plus N4-behenoyl-1-beta-D-arabinofuranosylcytosine in acute myelogenous leukemia: a newly designed induction regimen-a prospective, cooperative multicenter study. Semin Hematol. 1996. 33:4 Suppl 3. 24–29.
8. Barker CC, Anderson RA, Sauve RS, Butzner JD. GI complications in pediatric patients post-BMT. Bone Marrow Transplant. 2005. 36:51–58.

9. McGregor GI, Shepherd JD, Phillips GL. Acute graft-versus-host disease of the intestine. A surgical perspective. Am J Surg. 1988. 155:680–682.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download