Abstract
Background
Radioimmunotherapy agents have a highly significant role in autologous stem cell transplantation as they improve tolerability and increase the efficacy of the conditioning regimen.
Methods
We retrospectively analyzed the efficacy and toxicity of yttrium-90 ibritumomab tiuxetan (Zevalin) combined with intravenous busulfan, cyclophosphamide, and etoposide (Z-BuCyE) compared with those of BuCyE alone followed by autologous stem cell transplantation in patients with relapsed or refractory B-cell non-Hodgkin lymphoma (NHL). The efficacy, toxicity, and engraftment characteristics were compared between 19 patients who received Z-BuCyE and 19 historical controls who received BuCyE.
Results
The 2 treatment groups shared similar baseline characteristics. The median time to platelet engraftment (>20×109/L) and neutrophil engraftment (>0.5×109/L) did not significantly differ between the Z-BuCyE group (12 days and 10 days, respectively) and the BuCyE group (12 days and 10 days, respectively). No significant differences were observed between the groups with respect to toxicities and treatment-related mortality. The median follow-up period was 30.4 months, and median event-free survival was generally better in the Z-BuCyE group (12.5 months) vs. the BuCyE group (6.2 months, P=0.236). No significant difference in overall survival between the groups was noted.
High-dose chemotherapy (HDC) followed by autologous stem cell transplantation (ASCT) is considered standard therapy for patients with chemo-sensitive relapsed aggressive lymphoma. The PARMA trial demonstrated that the 5-year event-free survival rate was superior in patients who received ASCT compared with those undergoing conventional chemotherapy [1]. Other randomized trials have also shown improved event-free survival [2, 3]. However, despite treatment with an intensified chemotherapy regimen combined with ASCT, long-term disease control rates range from only 25-45% in patients with relapsed or refractory aggressive lymphomas [4-6]. Relapses in patients receiving HDC in conjunction with ASCT are primarily caused by cancer cells remaining in the body after ablative chemotherapy [7]. Therefore, approaches involving methods for improving eradication of lymphoma cells and preventing recurrence are urgently needed for improving survival after ASCT.
Investigators have recently incorporated radioimmunotherapies (RIT) with agents such as yttrium-90 ibritumomab tiuxetan (Zevalin), a radiotherapeutic monoclonal antibody directed against B-lymphocyte antigen CD20, into conditioning regimens for treating relapsed lymphoma [8-10]. Studies have shown that the combination of ibritumomab tiuxetan with BEAM (carmustine [BCNU], etoposide, cytosine arabinoside, and melphalan) or Zevalin (Z)-BEAM showed promising results. Particularly, improved survival outcomes associated with ibritumomab tiuxetan in combination with HDC for patients with aggressive lymphomas were noted in comparison with those for historical controls without the use of RIT [9-11]. Several lines of evidence suggested that the inclusion of ibritumomab tiuxetan in Z-BEAM compared with BEAM alone administered prior to ASCT can improve survival outcomes [12, 13].
Busulfan (Bu)-based conditioning regimens, which are commonly used prior to allogenic SCT, have also been used with ASCT for treating lymphoma [14-16]. Comparative analysis showed that busulfan, cyclophosphamide and etoposide (BuCyE) together are an effective conditioning regimen for ASCT, showing similar survival outcomes and toxicity profiles as BEAM [17]. To combine a BuCyE conditioning regimen with RIT, we previously demonstrated the efficacy and safety of ibritumomab tiuxetan combined with BuCyE (Z-BuCyE) followed by ASCT in patients with relapsed or refractory aggressive B-cell non-Hodgkin lymphoma (NHL) [18]. Although the role of ibritumomab tiuxetan in conditioning regimens has been assumed, limited information exists regarding the comparative efficacies and toxicities of this regimen and BuCyE alone. We therefore compared the efficacy and toxicity of the Z-BuCyE and BuCyE regimens in patients with NHL.
Between October 2005 and May 2011, 71 NHL patients underwent HDC using BuCyE (N=52) or Z-BuCyE (N=19), followed by ASCT, at Asan Medical Center (Seoul, Korea). Patients treated with Z-BuCyE had histologically confirmed, relapsed, or refractory CD20 positive B-cell NHL, including follicular, marginal zone B-cell, mantle cell, diffuse large B-cell, and Burkitt lymphomas. Fifteen patients treated in a prospective multicenter trial with Z-BuCyE were included in the analysis and were included in the Z-BuCyE group [18]. Of 52 patients receiving BuCyE, 19 patients presented with B-cell NHL histology. This group of patients comprised the historical controls for the Z-BuCyE group (N=19). Other patients presented with primary central nervous system lymphoma (N=18), natural killer T-cell lymphoma (N=6), and peripheral T-cell NHL (N=9).
Chemotherapy doses were based on body weight as follows. Patients in the Z-BuCyE group received a Z-BuCyE conditioning regimen, which corresponded to rituximab 250 mg/m2 on day -21 and day -14, ibritumomab tiuxetan 0.4 mCi/kg on day -14, busulfan 3.2 mg/kg on days -7 through -5, cyclophosphamide 50 mg/kg on days -3 and -2, and etoposide 400 mg/m2 on days -5 and -4. Patients in the BuCyE group were given the same regimen as above, excluding rituximab and ibritumomab tiuxetan. Hematopoietic SCs were then infused on day 0.
All patients were administered seizure prophylaxis with phenytoin prior to the first dose of busulfan. The uroepithelial prophylaxis for cyclophosphamide administration included hydration and mesna to prevent bleeding from the bladder. All patients received subcutaneous granulocyte colony-stimulating factor (G-CSF) (5 g/kg) beginning on day 1 of ASCT until neutrophil counts were stable at >1.0×109/L for 3 consecutive days. Prophylaxis for opportunistic infections and antimicrobial therapy in the case of febrile episodes were administered according to previously described protocols [17-19].
In this study, indolent lymphoma indicated the presence of follicular and marginal zone B-cell lymphomas, while aggressive lymphoma indicated the presence of mantle cell, diffuse large B-cell, and Burkitt lymphomas. The period of event-free survival (EFS) was defined as the time from the day of ASCT to the time of disease progression, relapse, or death from any cause. Overall survival (OS) was defined as the time from the day of ASCT to the time of death from any cause. Response was evaluated according to the response criteria provided by the International Working Group [20]. The duration of complete response (CR) was defined as the time from the day of ASCT to the time of relapse in patients with continued CR, or from the day of achievement of CR after ASCT to the time of relapse in patients with induced CR. As noted above, the day of SC infusion was defined as day 0. Chemo-sensitive disease was defined as a reduction in measurable disease following salvage chemotherapy prior to ASCT, meeting the criteria of partial response (PR). Patients were considered to have chemo-resistant disease if the reduction in measurable disease did not meet the PR criteria. Time to neutrophil engraftment was defined as the time from the day of ASCT to the first day of the 3 consecutive days when the absolute neutrophil count (ANC) was >0.5×109/L, and the time to platelet engraftment was defined as the time from the day of ASCT to the first day when the platelet count was >20×109/L. Toxicities were assessed and graded according to the National Cancer Institute Common Toxicity Criteria for Adverse Events (NCI CTCAE), version 3.0. Response evaluations were performed every 3 months after ASCT for the first 2 years, every 6 months for the next 3 years, and then annually or as clinically indicated.
Between-group comparisons were conducted using the Mann-Whitney U-test for continuous variables and the chi-square test or Fisher exact test for categorical variables. Differences between Kaplan-Meier curves for EFS, OS, and CR durations were assessed using the log-rank test. Two-tailed P values<0.05 were regarded as significant. All calculations were performed using the Statistical Package for the Social Sciences (SPSS), version 11.0, for Windows (SPSS Inc., Chicago, IL, USA).
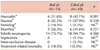
Baseline characteristics of the 38 patients included in this study are summarized in Table 1. The median age was 52 years (range, 29-65) in the BuCyE group and 54 years (range, 27-64) in Z-BuCyE group. Of these patients, 15 patients in the BuCyE group and 17 patients in the Z-BuCyE group had an aggressive histology. The numbers of patients with >2 prior chemotherapy regimens were 6 and 4 in the BuCyE and Z-BuCyE groups, respectively. Most patients (N=36) received the ESHAP regimen (etoposide, carboplating, cytarabine, and methylprednisolone) as pre-ASCT chemotherapy. A higher percentage of patients in the Z-BuCyE group were male. Other characteristics, including performance status, number of previous regimens of chemotherapy, prior radiotherapy, prior use of rituximab, involvement of extranodal sites, International Prognostic Index (IPI), and disease status at the time of salvage, were similar between the 2 groups.
Engraftment data are summarized in Table 2. The median time to neutrophil and platelet engraftment did not differ significantly between the 2 groups. Thrombocytopenia persisted for 103 days after ASCT in one female patient who received Z-BuCyE. Bone marrow examination for this patient showed the presence of hypocellular marrow without lymphoma involvement. However, the patient had enlarged cervical lymph nodes at 9 months, indicating a relapse. The requirement for the transfusion of red blood cells and platelets and the median duration of hospitalization were comparable between the 2 groups.
Table 3 shows that the percentage of patients with mucositis, nausea, and diarrhea of at least grade 2 was generally higher in the Z-BuCyE group than in the BuCyE group, but this result was not statistically significant. Febrile neutropenia occurred in 73.7% and 94.7% of patients conditioned with BuCyE and Z-BuCyE, respectively (P=0.180). One patient in the Z-BuCyE group experienced septicemia caused by Klebsiella pneumoniae, but improved following treatment with antibiotics. Another patient in the Z-BuCyE group and 2 in the BuCyE group died within 100 days after ASCT due to treatment-related complications. One patient died due to veno-occlusive disease (VOD) after Z-BuCyE, and 2 patients died due to bacterial infections accompanied by severe mucositis after BuCyE.
The objective overall response rate was 89.5% (17/19) in the Z-BuCyE group and 78.9% (15/19) in the BuCyE group (P=0.649). CR rates in the Z-BuCyE and BuCyE groups were 78.9% (continued CR, 100% [8/8]; induced CR, 63.6% [7/11]) and 73.7% (continued CR, 83.3% [5/6]; induced CR, 69.2% [9/13]), respectively (P=1.000). Median follow-up duration for survivors was 30.4 months (range, 0.8-68.5 months). There was a trend toward improved EFS in the Z-BuCyE group, with a 3-year EFS rate of 26.8% compared with that of 15.8% in the BuCyE group (P=0.236; Fig. 1A). Median EFS durations were 12.5 months and 6.2 months after Z-BuCyE and BuCyE, respectively. The median duration of CR was 15.9 months after Z-BuCyE and 7.7 months after BuCyE (P=0.170; Fig. 1B). The 3-year OS rate in the Z-BuCyE and the BuCyE groups were 51% and 49%, respectively (P=0.767; Fig. 1C). No statistical difference in EFS and OS was observed with regard to age (>55 years vs. ≤55 years), histology (DLBCL vs. others), disease status at ASCT (CR vs. non-CR), and the number of prior chemotherapy regimens (2 vs. 3).
Relapse and death events are listed in Table 4. In the BuCyE group, 11 of 14 relapsed patients underwent further chemotherapy, whereas in the Z-BuCyE group, 9 of 10 underwent palliative chemotherapy or radiotherapy.
RIT combines the effects of radiotherapy with immunologic targeting of cell-type-specific monoclonal antibodies for treating lymphoma. Our findings suggest that incorporating ibritumomab tiuxetan into treatment with BuCyE compared with BuCyE alone for ASCT is feasible and may provide additional benefits for patients with relapsed or refractory B-cell NHL.
Our EFS findings are consistent with results of previous studies, suggesting a potential benefit of ibritumomab tiuxetan administration for patients receiving BuCyE followed by ASCT. For example, several studies comparing Z-BEAM with BEAM alone have reported improved efficacy for patients with B-cell NHL. Krishnan et al. demonstrated favorable outcomes in 65 patients with aggressive NHL, with 2-year EFS rates of 72% and 67% in the Z-BuCyE and BuCyE groups, respectively [12]. A randomized phase II study reported a trend toward improved EFS at 2 years in the Z-BEAM group (N=22) of 59% versus 37% for the BEAM group (N=21) [13]. In this study, improved EFS in the Z-BuCyE group is likely attributable to the prolonged CR duration after Z-BuCyE conditioning compared with that after BuCyE conditioning (15.9 months versus 7.7 months). As an additive effect of RIT in ASCT, RIT agents such as ibritumomab tiuxetan appear to have advantages based on the emission of β-particles, which can penetrate several millimeters [21, 22]. Hence, RIT with ibritumomab tiuxetan makes it possible to deliver a therapeutic dose of radiation not only to nearby lymphoma cells, but also to neighboring cells that are farther from the tumor surface. This feature may prolong the duration of the response [23, 24].
RIT alone is associated with hematologic toxicities. However, hematologic toxicities observed following RIT can be overcome using SC infusion [25, 26]. In the current study, toxicity profiles of the patients in the Z-BuCyE group were comparable with those of the BuCyE group patients, although 1 patient in the Z-BuCyE group died from VOD. Ibritumomab tiuxetan appears to be safely incorporated into myeloablative regimens, as life-threatening hematologic toxicities associated with RIT and HDC were rescued with ASCT, which was demonstrated by only 1 patient who experienced septicemia. This favorable toxicity profile is encouraging, considering that most patients enrolled in this cohort were middle-aged or elderly.
Till the time of manuscript preparation, no patients in this cohort had developed secondary malignancy. Although there are concerns regarding the development of secondary malignancies following RIT combined with ASCT, secondary malignancies with high-dose Z-BEAM have been observed in only 7% of patients, which is similar to the rate observed with HDC alone [27, 28]. Moreover, adverse events were similar to those seen with BEAM alone [8-12]. Data from a larger number of patients with a longer duration of follow-up are required to properly evaluate the probability of developing secondary malignancies.
Survival outcomes for the cohort appear to be numerically inferior compared with our previous results [16, 17]. Although the CR rates of 78.9% and 73.7% in the Z-BuCyE and BuCyE groups after ASCT were relatively high, EFS and OS data in this study were not promising. This may be due, at least in part, to adverse patient characteristics such as multiple extranodal involvement, as well as extensive previous treatment (chemotherapy and/or radiotherapy) (Table 1) [29, 30].
Nevertheless, because of the similarities between the Z-BuCyE and BuCyE groups in terms of disease-related characteristics affecting prognosis such as histology, disease status at the time of salvage, and the number of prior regimens, our results may provide further information about the role of ibritumomab tiuxetan in conditioning regimens in combination with ASCT.
This study has some limitations. The study was retrospective in nature, included a small number of patients with a relatively short follow-up period, and involved a selected group of patients with relatively poor clinical features. Nevertheless, the patient cohort was derived from patients treated with a uniform treatment protocol in a single center.
In conclusion, our findings suggest that the use of ibritumomab tiuxetan in combination with BuCyE may increase treatment efficacy as well as reduce treatment toxicity and yield an engraftment profile similar to that of BuCyE alone. These observations should be further examined in a randomized study to define the role of RIT for treating lymphoma patients.
Figures and Tables
 | Fig. 1Event-free survival (EFS, A), duration of complete response (CR, B), and overall survival (OS, C) after high-dose chemotherapy (HDC) with Z-BuCyE or BuCyE followed by autologous stem cell transplantation (ASCT). |
Table 1
Patient characteristics.

Abbreviations: ASCT, autologous stem cell transplantation; NHL, non-Hodgkin's lymphoma; MZL, marginal zone B-cell lymphoma; FL, follicular lymphoma; MCL, mantle cell lymphoma; DLBCL, diffuse large B-cell lymphoma; BL, Burkitt lymphoma; IPI, international prognostic index; CR, complete response; Z-BuCyE, ibritumomab tiuxetan, busulfan, cyclophosphamide and etoposide.
ACKNOWLEDGEMENTS
We thank Bayer Korea Ltd. (Seoul, Korea), which provided the 90Y-ibritumomab tiuxetan to some patients enrolled in a trial. This study was presented in part at the 53rd ASH annual meeting and exposition, December 10-13, 2011.
References
1. Philip T, Guglielmi C, Hagenbeek A, et al. Autologous bone marrow transplantation as compared with salvage chemotherapy in relapses of chemotherapy-sensitive non-Hodgkin's lymphoma. N Engl J Med. 1995. 333:1540–1545.

2. Schouten HC, Qian W, Kvaloy S, et al. High-dose therapy improves progression-free survival and survival in relapsed follicular non-Hodgkin's lymphoma: results from the randomized European CUP trial. J Clin Oncol. 2003. 21:3918–3927.

3. Dreyling M, Lenz G, Hoster E, et al. Early consolidation by myeloablative radiochemotherapy followed by autologous stem cell transplantation in first remission significantly prolongs progression-free survival in mantle-cell lymphoma: results of a prospective randomized trial of the European MCL Network. Blood. 2005. 105:2677–2684.

4. Kewalramani T, Zelenetz AD, Hedrick EE, et al. High-dose chemoradiotherapy and autologous stem cell transplantation for patients with primary refractory aggressive non-Hodgkin lymphoma: an intention-to-treat analysis. Blood. 2000. 96:2399–2404.

5. Vose JM, Zhang MJ, Rowlings PA, et al. Autologous transplantation for diffuse aggressive non-Hodgkin's lymphoma in patients never achieving remission: a report from the Autologous Blood and Marrow Transplant Registry. J Clin Oncol. 2001. 19:406–413.

6. Josting A, Sieniawski M, Glossmann JP, et al. High-dose sequential chemotherapy followed by autologous stem cell transplantation in relapsed and refractory aggressive non-Hodgkin's lymphoma: results of a multicenter phase II study. Ann Oncol. 2005. 16:1359–1365.

7. Gianni AM, Berinstein NL, Evans PA, López-Guillermo A, Solano C. Stem-cell transplantation in non-Hodgkin's lymphoma: improving outcome. Anticancer Drugs. 2002. 13:Suppl 2. S35–S42.

8. Gisselbrecht C, Bethge W, Duarte RF, et al. Current status and future perspectives for yttrium-90 ((90)Y)-ibritumomab tiuxetan in stem cell transplantation for non-Hodgkin's lymphoma. Bone Marrow Transplant. 2007. 40:1007–1017.

9. Shimoni A, Zwas ST, Oksman Y, et al. Yttrium-90-ibritumomab tiuxetan (Zevalin) combined with high-dose BEAM chemotherapy and autologous stem cell transplantation for chemo-refractory aggressive non-Hodgkin's lymphoma. Exp Hematol. 2007. 35:534–540.

10. Krishnan A, Nademanee A, Fung HC, et al. Phase II trial of a transplantation regimen of yttrium-90 ibritumomab tiuxetan and high-dose chemotherapy in patients with non-Hodgkin's lymphoma. J Clin Oncol. 2008. 26:90–95.

11. Khouri IF, Saliba RM, Hosing C, et al. Efficacy and safety of yttrium 90 (90Y) ibritumomab tiuxetan in autologous and nonmyeloablative stem cell transplantation (NST) for relapsed non-Hodgkin's lymphoma (NHL). Blood. 2006. 108:Abst 315.

12. Krishnan AY, Nademanee A, Raubitschek A, et al. A comparison of Beam and yttrium 90 ibritumomab tiuxetan (Zevalin(R)) in addition to Beam (Z-BEAM) in older patients undergoing autologous stem cell transplant (ASCT) for B-cell lymphomas: Impact of radioimmunotherapy on transplant outcomes. Blood. 2006. 108:Abst 3043.
13. Shimoni A, Avivi I, Rowe JM, et al. A randomized study comparing yttrium-90 ibritumomab tiuxetan (Zevalin) and high-dose BEAM chemotherapy versus BEAM alone as the conditioning regimen before autologous stem cell transplantation in patients with aggressive lymphoma. Cancer. 2012. [Epub ahead of print].

14. Copelan EA, Penza SL, Pohlman B, et al. Autotransplantation following busulfan, etoposide and cyclophosphamide in patients with non-Hodgkin's lymphoma. Bone Marrow Transplant. 2000. 25:1243–1248.

15. Hänel M, Kröger N, Sonnenberg S, et al. Busulfan, cyclophosphamide, and etoposide as high-dose conditioning regimen in patients with malignant lymphoma. Ann Hematol. 2002. 81:96–102.

16. Kim JG, Sohn SK, Chae YS, et al. Multicenter study of intravenous busulfan, cyclophosphamide, and etoposide (i.v. Bu/Cy/E) as conditioning regimen for autologous stem cell transplantation in patients with non-Hodgkin's lymphoma. Bone Marrow Transplant. 2007. 40:919–924.

17. Kim JE, Lee DH, Yoo C, et al. BEAM or BuCyE high-dose chemotherapy followed by autologous stem cell transplantation in non-Hodgkin's lymphoma patients: a single center comparative analysis of efficacy and toxicity. Leuk Res. 2011. 35:183–187.

18. Kang BW, Kim WS, Kim C, et al. Yttrium-90-ibritumomab tiuxetan in combination with intravenous busulfan, cyclophosphamide, and etoposide followed by autologous stem cell transplantation in patients with relapsed or refractory B-cell non-Hodgkin's lymphoma. Invest New Drugs. 2010. 28:516–522.

19. Jo JC, Kang BW, Jang G, et al. BEAC or BEAM high-dose chemotherapy followed by autologous stem cell transplantation in non-Hodgkin's lymphoma patients: comparative analysis of efficacy and toxicity. Ann Hematol. 2008. 87:43–48.

20. Cheson BD, Horning SJ, Coiffier B, et al. NCI Sponsored International Working Group. Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. J Clin Oncol. 1999. 17:1244.

22. Krishnan A, Palmer JM, Tsai NC, et al. Matched-cohort analysis of autologous hematopoietic cell transplantation with radioimmunotherapy versus total body irradiation-based conditioning for poor-risk diffuse large cell lymphoma. Biol Blood Marrow Transplant. 2011. 18:441–450.

23. Hagenbeek A, Lewington V. Report of a European consensus workshop to develop recommendations for the optimal use of (90)Y-ibritumomab tiuxetan (Zevalin) in lymphoma. Ann Oncol. 2005. 16:786–792.

24. Weigert O, Illidge T, Hiddemann W, Dreyling M. Recommendations for the use of yttrium-90 ibritumomab tiuxetan in malignant lymphoma. Cancer. 2006. 107:686–695.

25. Schilder R, Molina A, Bartlett N, et al. Follow-up results of a phase II study of ibritumomab tiuxetan radioimmunotherapy in patients with relapsed or refractory low-grade, follicular, or transformed B-cell non-Hodgkin's lymphoma and mild thrombocytopenia. Cancer Biother Radiopharm. 2004. 19:478–481.

26. Morschhauser F, Illidge T, Huglo D, et al. Efficacy and safety of yttrium-90 ibritumomab tiuxetan in patients with relapsed or refractory diffuse large B-cell lymphoma not appropriate for autologous stem-cell transplantation. Blood. 2007. 110:54–58.

27. Krishnan A, Bhatia S, Slovak ML, et al. Predictors of therapy-related leukemia and myelodysplasia following autologous transplantation for lymphoma: an assessment of risk factors. Blood. 2000. 95:1588–1593.

28. Seshadri T, Pintilie M, Tsang R, et al. Second cancers after autologous hematopoietic stem cell transplantation (ASCT) for relapsed/refractory aggressive non-Hodgkin's lymphoma (NHL). Blood. 2007. 110:Abst 1673.

29. Voso MT, Martin S, Hohaus S, et al. Prognostic factors for the clinical outcome of patients with follicular lymphoma following high-dose therapy and peripheral blood stem cell transplantation (PBSCT). Bone Marrow Transplant. 2000. 25:957–964.

30. de Kreuk M, Ossenkoppele GJ, Meijer CJ, Huijgens PC. Prognostic factors for survival of non-Hodgkin's lymphoma patients treated with high-dose chemotherapy and autologous bone marrow transplantation. Bone Marrow Transplant. 1996. 17:963–971.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download