Abstract
Background
Knowledge of the roles of tacrolimus and minidose methotrexate (MTX) in the prevention of acute graft-versus-host disease (aGVHD) in pediatric allogeneic hematopoietic stem cell transplantation (HSCT) is limited. We retrospectively evaluated the engraftment status, incidence of aGVHD and chronic GVHD (cGVHD), and toxicities of tacrolimus and minidose MTX in aGVHD prophylaxis in children undergoing allogeneic HSCT.
Methods
Seventeen children, who underwent allogeneic HSCT and received tacrolimus and minidose MTX as GVHD prophylaxis from March 2003 to February 2011, were reviewed retrospectively. All the patients received tacrolimus since the day before transplantation at a dose of 0.03 mg/kg/day and MTX at a dose of 5 mg/m2 on days 1, 3, 6, and 11.
Results
Of the 17 patients, 9 received human leukocyte antigen (HLA)-matched related donor transplants, and 8 received HLA-matched, or partially mismatched unrelated donor transplants. The median time for follow-up was 55 months. The incidence of aGVHD in the related and unrelated donor groups was 22.2% and 42.9%, respectively. cGVHD was not observed. To maintain therapeutic blood levels of tacrolimus, the younger group (<8 years of age) required an increased mean dose compared to the older group (≥8 years) (P=0.0075). The adverse events commonly associated with tacrolimus included hypomagnesemia (88%), nephrotoxicity (23%), and hyperglycemia (23%).
Prevention of graft-versus-host disease (GVHD) is a critical factor in transplant-related morbidity and mortality and has been a major target of research in the field of hematopoietic stem cell transplantation (HSCT) [1]. Currently, many transplant centers use cyclosporine (CSP) as a major immunosuppressant, which is combined with various doses and schedules of methotrexate (MTX) and/or methylprednisolone for the prevention of GVHD [2].
Tacrolimus (FK506) is a macrolide lactone immunosuppressant that was identified in 1984 from the fermentation broth of Streptomyces tsukubaensis; it has potent inhibitory effects on T-cell activation and acts by downregulating the expression of IL-2 [3-5]. In vitro, it is capable of 100 times greater inhibition of T cells than CSP [4, 5]. Tacrolimus has been shown to be effective in the prevention of graft rejection following solid organ transplantation [6]. The use of tacrolimus to prevent aGVHD in adult recipients of HSCT has been reported in multiple trials [7, 8]. The combination of tacrolimus and MTX, following unrelated donor marrow transplantation, significantly decreased the risk of aGVHD, compared to the combination of CSP and MTX, with no significant increase in toxicity, infections, or leukemia relapse [7-9]. Minidose MTX does not compromise the efficacy of GVHD prophylaxis; instead, it reduces the risk of severe treatment-related mucositis [7]. In a phase II multicenter trial for tacrolimus for GVHD prophylaxis following unrelated donor transplantation, no differences were found in the risk for GVHD between the groups treated with standard MTX and minidose MTX [10-12].
Currently, data evaluating the efficacy and tolerance of tacrolimus and MTX in GVHD prophylaxis in children is limited [13, 14], with only 2 such studies reported to date [15, 16]. In addition, the pharmacokinetic properties of tacrolimus in children have been shown to be different from those in adults, with 2 studies showing an increased clearance from the blood sream in pediatric patients [14, 15]. We retrospectively evaluated the engraftment status, incidence of aGVHD and cGVHD, toxicities, and mean dose of tacrolimus to maintain therapeutic drug levels in children undergoing allogeneic HSCT using tacrolimus and minidose MTX as GVHD prophylaxis at a single center in Korea.
The study subjects included 17 children who received tacrolimus and minidose MTX for the prevention of GVHD at the Pediatric HSCT Unit at Pusan National University Hospital. Patient records from March 2003 to February 2011 were reviewed retrospectively.
Tacrolimus was administered intravenously since the day before transplantation at 0.03 mg/kg/day via continuous infusion. Following engraftment, once the patient was able to consume oral medications, tacrolimus was administered as an oral dose at a concentration of 4 times the intravenous (IV) dose. The oral dose was administered in 2 doses every 12 h. Tacrolimus levels were monitored every second day, and the dosage was adjusted to maintain trough levels between 5 and 15 ng/mL. In the absence of GVHD, tacrolimus dosage was subsequently tapered by 25% per month and discontinued by day 180. Children with aGVHD continued to receive tacrolimus at the discretion of the physician. Dosage modifications of tacrolimus were also made in patients who developed serum creatinine levels that were >2 times the baseline value. Minidose MTX was administered intravenously on post-transplant days 1, 3, 6, and 11 at a dose of 5 mg/m2. The dose on day 11 was reduced or omitted when the patient was unable to swallow due to severe oral mucositis.
Neutrophil engraftment was defined as the first of 3 consecutive days when the absolute neutrophil count of peripheral blood (PB) exceeded 0.5×109/L; platelet engraftment was defined as the first day when the platelet count exceeded 20×109/L without the need for platelet transfusions the following week. Toxicity was evaluated using the Common Terminology Criteria for Adverse Events v3.0 from the National Cancer Institute (NCI) [17].
Seventeen patients (age, 17 months-17 years) undergoing allogeneic HSCT received tacrolimus and minidose MTX for the prevention of aGVHD. Fifteen patients had hematological malignancies (8 had acute myeloid leukemia, 7 had acute lymphoblastic leukemia (ALL), 1 had Fanconi anemia, and 1 had severe aplastic anemia) (Table 1). Related and unrelated donor transplants were received by 9, and 8 patients, respectively (Table 2). The degree of HLA matching was as follows: 7 matched sibling bone marrow (BM) or PB donors and 2 matched sibling cord blood (CB) donors had 6/6 HLA matches; 4 unrelated BM or PB donors had 8/8 HLA matches; 2 unrelated PB donors had 7/8 HLA matches; 2 unrelated CB donors had 5/6 HLA matches, 4/6 HLA matches in each. Patients were followed up for a median time of 55 months post-transplantation (range, 1-107 months). Chemotherapy-based conditioning regimens were administered to 16 patients; 8 received busulfan, fludarabine, and/or antithymocyte globulin (ATG); 4 received busulfan, melphalan, and ATG; and 2 received fludarabine, cyclophosphamide, and ATG. Only 1 patient with ALL received total body irradiation as a part of the preparatory conditioning (Table 2).
The median number of total nucleated cells (TNC) infused was 8.6×108/kg (range, 1.8-23.3×108/kg) and that of CD 34+ cells was 7.5×106/kg (range, 1.9-17.2×106/kg) in 13 patients with BM/PB stem cell transplant. The median number of infused TNC was 3.06×107/kg (range, 1.9-5.7×107/kg) and CD 34+ cells was 1.5×105/kg (range, 0.95-3.4×105/kg) for 4 patients who had undergone CB transplantation (CBT). With the exception of 1 patient who received an unrelated CBT, all the patients were successfully engrafted. The median time for neutrophil engraftment was 15 days (range, 9-24 days) post-transplantation, while platelet recovery occurred at a median of 19 days (range, 9-77 days). Three patients died before platelet recovery due to aGVHD, acute respiratory distress syndrome, and veno-occlusive disease (VOD) (Table 3).
aGVHD occurred in 5 (31.3%) of the 16 patients who received grafts. In the related donor group, 2 (22.2%) of a total of 9 patients developed aGVHD; in the unrelated donor group, 3 (42.9%) of a total of 7 patients developed aGVHD. Among the 4 patients who developed grade II aGVHD, 2 had received related transplants, and the rest had received unrelated transplants. Only 1 patient who had received an unrelated transplant developed grade IV aGVHD and died from hepatic failure (Table 3). Grade III-IV aGVHD did not occur in the related donor group. Cases that could be evaluated for cGVHD (engrafted and survived until post-transplantation day 100) were 13/17 transplant recipients. cGVHD was not found to occur in either group (Table 4).
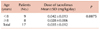
The mean IV dose of administrated tacrolimus was 0.035±0.012 mg/kg/day (range, 0.025-0.050 mg/kg), and the mean blood concentration of tacrolimus was 7.12±0.49 ng/mL (range, 5.13-11.82 ng/mL). To maintain therapeutic levels of tacrolimus in the blood (5-15 ng/mL), an increased mean dose (0.042 mg/kg/day was administered to the younger group (<8 years old), compared to that administered (0.028 mg/kg/day to the older group (≥8 years old), P=0.0075) (Table 5). The mean blood concentration of tacrolimus in the children who did not develop aGVHD was higher (8.11±1.83 ng/mL) than in those who developed aGVHD (6.04±2.54 ng/mL) (P=0.038).
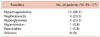
Hypomagnesemia (88.2%) was the most frequent adverse event associated with tacrolimus administration (Table 6), with the median time to peak being post-transplantation day 21 (range, days 4-39). Magnesium supplementation was required in all cases during the administration of tacrolimus. Four patients (23.5%) developed nephrotoxicity but no patient required hemodialysis. Hyperglycemia was observed in 4 patients (23.5%), but no patient required insulin management other than the adjustment of total parenteral nutrition formulation. Hypertension and pancreatitis occurred in 1 patient in each case (5.8%). Neurotoxicity symptoms such as tremor or seizure, hemolytic uremic syndrome (HUS), and thrombotic thrombocytopenic purpura (TTP) were not observed in this study. Oral mucositis was noted in all patients during the first 2 weeks of post-transplantation. Of these, 3 (18%) were grade 1; 5 (29%), grade 2; 8 (47%), grade 3; and 1 (6%) was grade 4.
With a median follow-up of 55 months (range, 1-107 months), the survival rates at 100 days post-transplantation and 1 year were 82% and 70%, respectively. Among the 15 patients who received transplants for leukemia, 3 patients experienced a relapse. Although 2 patients died from disease progression following the relapse, the third patient is alive and in remission at 100 months after chemotherapy. The causes of death of 6 patients included leukemic relapse, aGVHD, ARDS, VOD, and secondary engraftment failure (Table 3).
Cyclosporine and MTX have been the standard therapy for GVHD prophylaxis [1, 2]. Recently, many studies have demonstrated the advantage of using tacrolimus and MTX for GVHD prophylaxis in adult patients [6-9]. In addition, it has also been shown that minidose MTX does not compromise the efficacy of GVHD prophylaxis, and it simultaneously reduces the risk of severe treatment-related mucositis [7]. The use of tacrolimus and minidose MTX in the prevention of aGVHD has been extensively evaluated in adults undergoing allogeneic HSCT [7, 10-12, 20]; however, studies on their activity in pediatric patients are limited [13-16]. The results from our study demonstrate that the use of tacrolimus and minidose MTX in aGVHD prophylaxis is safe and effective in pediatric patients.
Przepiorka et al. [13] reported the cases of 10 pediatric patients who underwent mismatched CB transplants. In their study, the incidence of grade II aGVHD was 77% with no grade III-IV aGVHD, and cGVHD was found in 22% cases and limited to the skin. Yanik et al. [14] reported the cases of 41 pediatric patients who received tacrolimus and standard doses of MTX for GVHD prophylaxis during HSCT from related and unrelated donors. In their study, the incidence of grades II-IV and III-IV aGVHD was 55% and 30%, respectively, in unrelated transplant recipients; 19% of related transplant recipients developed grade III-IV aGVHD, while 43% developed cGVHD. In a study involving 24 pediatric patients who had undergone 26 HSCT procedures reported by Sabapathy et al. [15], the incidence of grade II-IV aGVHD was 17%, with 4% of the patients developing grade III aGVHD and 5% developing extensive cGVHD; there was no incidence of grade IV aGVHD.
In our study, grade II-IV aGVHD occurred in 5 patients (31%). Only 1 patient who received an unrelated BM transplant developed grade III-IV aGVHD (6.2%). The incidence of aGVHD was 22.2% in the related donor group, and 42.8% in the unrelated donor group. Grade III-IV aGVHD was not found to occur in the related donor group. There was no incidence of cGVHD in our study. Our results show that the frequency and severity of aGVHD are similar to those reported in previous pediatric studies; however, the frequency of cGVHD is lower than that reported earlier. It was not possible to accurately assess the risk of GVHD in our study due to the small study cohort, the variety of the sources of stem cells used, and the degree of the HLA matching.
The assessment of the tolerance of the drug regimen, especially in pediatric patients, was one of the principal aims of our study. The major adverse events associated with tacrolimus in adult allogeneic HSCT include nephrotoxicity (32-93%), neurotoxicity, hyperglycemia, and hypertension [3]. In contrast to adult trials, hypomagnesemia was the most common adverse event observed in our study, occurring in 88.2% of pediatric patients. Nephrotoxicity and hyperglycemia occurred in 23.5% of the patients, but did not require hemodialysis or insulin medication. Hypertension occurred in 5.8% of our patients, which was lower than that observed in the adult trials. Unlike earlier adult studies, neurotoxicity and HUS/TTP were not significant in pediatric patients.
For tacrolimus, optimal efficacy with minimal toxicity is maintained by careful monitoring to ensure levels between 5 and 15 ng/mL. Results of pharmacokinetic studies in children undergoing solid organ transplantation suggest that clearance of tacrolimus was increased, and hence, the dosage required for children might be different from that required for adults [21]. Additional data has shown that pediatric patients undergoing HSCT have a higher clearance of tacrolimus than that of adults [22, 23]. Our results show that an increased mean dose of tacrolimus was required to maintain therapeutic blood levels in the younger group (<8 years old) compared to the older group (≥8 years of age).
In summary, tacrolimus and minidose MTX in pediatric patients undergoing allogeneic HSCT were well tolerated and may be considered an effective therapy for the prevention of aGVHD. In addition, young children (<8 years old) undergoing HSCT may need to receive a higher initial dose of tacrolimus in order to maintain therapeutic levels. However, the limitations in our study for assessing the efficacy of tacrolimus and minidose MTX in children could arise from the small study cohort, the variety of stem cell sources used, and the degree of the HLA matching. Further evaluation consisting of prospective large, controlled studies to assess effective GVHD prophylactic regimens in pediatric patients is warranted.
Figures and Tables
Table 3
GVHD and clinical outcomes.

a)CMV colitis, b)Bone marrow relapse at 40 months post-transplantation, c)Bone marrow relapse at 10 months post-transplantation, d)Granulocytic sarcoma at 7 months post-transplantation.
Abbreviations: No., patient number; aGVHD, acute graft-versus-host disease; cGVHD, chronic GVHD; CMV, cytomegalovirus; CR, complete remission; DOD, died of disease; TRD, transplantation-related death; PD, progression of disease after relapse; NA, not applicable; ARDS, acute respiratory distress syndrome; VOD, hepatic veno-occlusive disease; EF2, secondary engraftment failure.
References
2. Nash RA, Pepe MS, Storb R, et al. Acute graft-versus-host disease: analysis of risk factors after allogeneic marrow transplantation and prophylaxis with cyclosporine and methotrexate. Blood. 1992. 80:1838–1845.

3. Jacobson P, Uberti J, Davis W, Ratanatharathorn V. Tacrolimus: a new agent for the prevention of graft-versus-host disease in hematopoietic stem cell transplantation. Bone Marrow Transplant. 1998. 22:217–225.

4. Klintmalm GB. FK 506: an update. Clin Transplant. 1994. 8:207–210.
5. Kino T, Hatanaka H, Hashimoto M, et al. FK-506, a novel immunosuppressant isolated from a Streptomyces. I. Fermentation, isolation, and physico-chemical and biological characteristics. J Antibiot (Tokyo). 1987. 40:1249–1255.

6. Shapiro R. Tacrolimus in pediatric renal transplantation: a review. Pediatr Transplant. 1998. 2:270–276.
7. Przepiorka D, Ippoliti C, Khouri I, et al. Tacrolimus and minidose methotrexate for prevention of acute graft-versus-host disease after matched unrelated donor marrow transplantation. Blood. 1996. 88:4383–4389.

8. Nash RA, Antin JH, Karanes C, et al. Phase 3 study comparing methotrexate and tacrolimus with methotrexate and cyclosporine for prophylaxis of acute graft-versus-host disease after marrow transplantation from unrelated donors. Blood. 2000. 96:2062–2068.
9. Hiraoka A, Ohashi Y, Okamoto S, et al. Phase III study comparing tacrolimus (FK506) with cyclosporine for graft-versus-host disease prophylaxis after allogeneic bone marrow transplantation. Bone Marrow Transplant. 2001. 28:181–185.

10. Fay JW, Nash RA, Wingard JR, et al. FK 506-based immunosuppression for prevention of graft versus host disease after unrelated donor marrow transplantation. Transplant Proc. 1995. 27:1374.
11. Przepiorka D, Khouri I, Ippoliti C, et al. Tacrolimus and minidose methotrexate for prevention of acute graft-versus-host disease after HLA-mismatched marrow or blood stem cell transplantation. Bone Marrow Transplant. 1999. 24:763–768.

12. Uberti JP, Ayash L, Braun T, Reynolds C, Silver S, Ratanatharathorn V. Tacrolimus as monotherapy or combined with minidose methotrexate for graft-versus-host disease prophylaxis after allogeneic peripheral blood stem cell transplantation: long-term outcomes. Bone Marrow Transplant. 2004. 34:425–431.

13. Przepiorka D, Petropoulos D, Mullen CA, Danielson M, Mattewada V, Chan KW. Tacrolimus for prevention of graft-versus-host disease after mismatched unrelated donor cord blood transplantation. Bone Marrow Transplant. 1999. 23:1291–1295.

14. Yanik G, Levine JE, Ratanatharathorn V, Dunn R, Ferrara J, Hutchinson RJ. Tacrolimus (FK506) and methotrexate as prophylaxis for acute graft-versus-host disease in pediatric allogeneic stem cell transplantation. Bone Marrow Transplant. 2000. 26:161–167.

15. Sabapathy C, Gourde JA, Khan SP, Rodriguez V. Tacrolimus with mini-methotrexate as prophylaxis for graft-versus-host disease in pediatric patients after allogeneic peripheral blood stem cell transplant or bone marrow transplant. J Pediatr Hematol Oncol. 2008. 30:945–949.

16. Kelly SS, Kelly P, Hunger SP, Wingard JR. Tacrolimus and "mini" methotrexate is an effective regimen for prevention of graftversus-host-disease in children undergoing umbilical cord blood transplant. Biol Blood Marrow Transplant. 2009. 15:Suppl 1. 81. (abst 220).

17. Common Terminology Criteria for Adverse Events (CTCAE) v3.0. Cancer Therapy Evaluation Program. 2006. Accessed March 23, 2012. Rockville, MD: National Cancer Institute;at http://ctep.cancer.gov/protocolDevelopment/electronic_applications/.
18. Glucksberg H, Storb R, Fefer A, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974. 18:295–304.

19. Shulman HM, Sullivan KM, Weiden PL, et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med. 1980. 69:204–217.
20. Devine SM, Geller RB, Lin LB, et al. The outcome of unrelated donor bone marrow transplantation in patients with hematologic malignancies using tacrolimus (FK506) and low dose methotrexate for graft-versus-host disease prophylaxis. Biol Blood Marrow Transplant. 1997. 3:25–33.
21. McDiarmid SV, Colonna JO 2nd, Shaked A, Vargas J, Ament ME, Busuttil RW. Differences in oral FK506 dose requirements between adult and pediatric liver transplant patients. Transplantation. 1993. 55:1328–1332.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download