INTRODUCTION
Korean National Health Insurance (NHI) was introduced in 1963 and became a nationwide health insurance after several law reforms in 1988. As a result of nationalization, coverage has expanded, and its service level has greatly improved since 1998 [1]. However, several diagnostic and therapeutic modalities for rare, incurable diseases such as malignant hematologic diseases are excluded from the reimbursement criteria, and this often complicates physicians' decision making in terms of evidence-based guidelines. The diagnosis and treatment of hematologic diseases have been rapidly advancing in recent years. However, NHI policy limitations hinder the addition of these advances to standard practice guidelines. Furthermore, the system's current principle of basic equal sharing regardless of disease severity will inevitably lead to a budget deficit. In this article, we aim to illuminate the insurance problems that arise in the treatment of hematologic diseases under the current NHI and propose solutions to these problems.
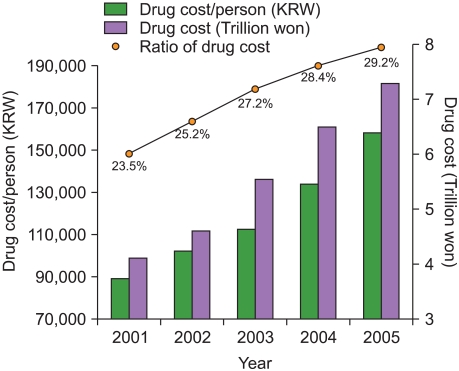
INSURANCE POLICY FOR NEW HIGH-PRICED DRUGS
The percentage of NHI-reimbursed health and medical fees that is used on pharmaceutical expenditure has been increasing since 2000 (Fig. 1), and expenditure has increased by 14% since 2001 [2]. Moreover, the development of new drugs, such as molecular-targeted agents, is expected to further increase expenditure. Currently, a "selective registration system" based on the cost-efficiency of new drugs is used to determine insurance reimbursement. Therefore, a product with poor cost-effectiveness will be designated as a product that will not be reimbursed by health insurance. This policy is more strictly applied to new high-priced drugs. Although this system has the advantage of reducing the proposed price of new drugs to an appropriate level, it has the disadvantage of delaying their introduction into clinical practice. It is essential to maintain reasonable control of drug costs to both adequately provide high-quality medicine that is critical for disease treatment and stabilize the insurance budget. Therefore, when estimating the price of new drugs, the establishment of a pharmaceutical policy based on Korea's purchasing power is crucial to secure price equality among nations. An expanded drug cost re-evaluation policy to adjust the price of a new drug according to its usage is also needed. In addition, once a drug patent has expired, the price should decrease, and a continuous control system for registered reimbursement drugs should be implemented to prevent unnecessary budget spending.
INSURANCE POLICY FOR PATIENTS WITH RARE, INCURABLE HEMATOLOGIC DISEASES
Although NHI generally does not cover rare, incurable diseases because of their rarity, there are approximately 320,000 patients suffering from 132 rare diseases in Korea. Many of these patients suffer from rare hematologic diseases such as hemophilia. The government is trying to enroll low-income individuals into the Medical Aid Program (MAP) to increase support for those with rare, incurable diseases and ease the burden for NHI member patients by reducing medical payments to 10%. However, these systematic supports are limited to NHI reimbursement services, since the patient pays fees for non-reimbursement services. Because of their uniqueness, the study and treatment of rare, incurable diseases need support from the entire nation. We need to better understand these diseases and the economic burden they place on a patient. Society should show an interest in these patients and continuously support them with donations and sponsorships.
INSURANCE POLICY FOR GERIATRIC PATIENTS WITH HEMATOLOGIC DISEASES
According to the 2008 Geriatric Population Investigation Report published by the Korean National Statistics Office, 10.3% (5 million) of the population was 65 years of age or older (www.kosis.kr). Since most malignant hematologic diseases occur at an older age, as the elderly population increases, a sharp increase in both the number of patients with hematologic diseases and medical spending on their treatment is expected [3]. According to September 2008 data from the Health Insurance Review and Assessment Service (HIRAS; 2007 Health Insurance Statistics Annual Report), in 2007, 4.4 million (9.2%) NHI members were aged over 65 years, whereas 486,000 (26.2%) medical reimbursement recipients were age 65 years or older. NHI reimbursements for geriatric medical fees was 9.8 trillion in 2007, which is a 22.8% increase from 2006, and this comprised 28.2% of all medical expenses, up from 25.9% in 2006 [4]. Therefore, the government needs to prepare for these ever-increasing medical fees by securing sufficient funds to cover them. Efforts should be made by medical professionals to evaluate the accompanying diseases and prognosis of geriatric patients in order to administer high-priced drugs to only those who could benefit from them. Furthermore, clinical studies should be implemented to determine the proper doses and methods of administration for drugs in the geriatric population.
INSURANCE POLICY FOR PEDIATRIC PATIENTS WITH HEMATOLOGIC DISEASES
Nowadays, insurance reimbursement seems to be moving in the direction of rational decision making partly based on evidence-based medicine. However, gathering enough data for evidence-based decision making in the treatment of pediatric hematologic diseases is a long and difficult process, since every year only 1,200 children under 15 years of age become pediatric cancer patients in Korea. From the point of view of pharmaceutical companies, the number of pediatric patients is relatively small compared to that of adult patients; thus, studies on pediatric subjects are difficult because pediatric patients are excluded from clinical research in most pharmaceutical companies. Therefore, there are relative disadvantages in terms of insurance reimbursement for pediatric hematologic patients. Recently, financial support plans have been drawn up for the treatment of rare pediatric diseases, and in the National Assembly, a bill was proposed that called for full financial support of medical fees for the treatment of pediatric neoplasms and rare diseases. However, even with this support, the medical fees paid by the patient's family will increase as the number of non-reimbursement drugs increases. This could lead physicians to either illegally administer drugs against a patient's will or to stop treatment. To ensure that pediatric patients with hematologic diseases grow into healthy members of our society, the NHI needs a new policy that expands reimbursement for drugs needed to treat pediatric patients with these diseases.
PRIVATE HEALTH INSURANCE POLICY FOR PATIENTS WITH HEMATOLOGIC DISEASES
According to the "Report of Korea Health Panel Survey 2008" by the Korea Institute for Health and Social Affairs (KIHASA) and the NHI Corporation, 76.1% of 7,866 households surveyed (24,616 people) had private health insurance. The number of signed contracts per household (mean, 3.13 persons per household) was 0.74 for single-person households, 1.58 for 2-person households, 3.32 for 3-person households, and 4.99 for 4-person households [5]. Despite the fact that Korean NHI is more accessible than that of other Organisation for Economic Co-operation and Development (OECD) nations and that the benefits from Korean NHI are increasing, 76.1% still chose to have private insurance. The reason for this could be insufficient support from public health insurance against financial losses due to diseases. However, it is also important to note that support for incurable diseases, including hematologic neoplasms, is being increased and that the high-cost treatments currently supported by private health insurance might no longer be standard treatments. Therefore, future financial support based on current standard guidelines could inevitably cause a gap between the effectiveness of private health insurance and an individual's expectations. To curtail the role of private health insurance, the current social welfare system needs to be supplemented financially, and public insurance must play the major role in reimbursement, whereas private health insurance should play a supplemental role and pay for any fees not covered by public insurance.
INSURANCE POLICY FOR LABORATORY TESTS
With the advancement in molecular and immunological diagnostic techniques for hematologic diseases, particularly malignant hematologic diseases, these techniques are becoming more routinely used. In fact, the operation of a cellular genetics laboratory within a clinical laboratory is now mandatory for the WHO classification, and the use of flexible and creative immunophenotyping techniques for the precise diagnosis of equivocal cases is increasing. Reimbursement policy should be flexible to allow for the determination of complex and overlapping immunophenotypes of various cancers. This flexibility could be achieved through expanded reimbursement and the rationalization of medical fees. Although the quality, sensitivity, and specificity of clonality analysis of immunoreceptor gene rearrangements in lymphoma and leukemia have greatly improved since the GeneScan method was introduced, reimbursement for diagnosis remains at the same level as when the Southern blot test was the methodology of choice. Because of this cost restriction, there is very limited use of newly developed tests in clinical practice. However, as future research on the detection of minimal residual disease in lymphoblastic leukemia/lymphoma and the analysis of immunoreceptors extends the understanding of the importance of newly developed methodology, an improved reimbursement policy is expected. Expanded discussions on the fees for rapid subtype analysis of leukemia and fluorescent in situ hybridization for cytogenetic analysis of lymphoma or myeloma cells are needed. Furthermore, when deciding the appropriate laboratory test fees, various factors such as establishing, maintaining, and analyzing test results must be considered.
THE REALITY AND PROSPECTS OF AN ARBITRARY NON-REIMBURSEMENT POLICY
On November 11, 2010, the Seoul High Court dismissed charges brought forward by the Korean Ministry of Health and Welfare and the NHI Corporation against Youido St. Mary's Hospital, The Catholic University of Korea. The judges in the decision emphasized that "If cases of additional charges to the patient under agreement with the patient are restricted, this would be seen as a violation of the patient's right to receive treatment, right to his own will, and the freedom of professional practice by physicians." In the current NHI system, only publicly notified cases are considered for reimbursement or non-reimbursement, and insurance is only applied for patients included in these cases. This limits rapid adaptation to advanced therapeutic modalities. Furthermore, patients' expectations for the latest treatment often causes controversy with physicians who are stuck in the non-reimbursement system, and this can seriously damage the trust between physicians and patients. The government should realize that problems with non-reimbursement cause irrational issues and should put forth the effort to rapidly resolve these problems.
CONCLUSION
The benefit of NHI for patients is that it affords high-quality medical services without a heavy financial burden. However, a breakdown of the medical referral system, which occurs because patients are free to use the medical institution of their choice, leads to increased medical costs and limits preservation of the current reimbursement system. The government is implementing various measures to lower costs to overcome such obstacles; however, as was demonstrated in the non-reimbursement charge case involving Youido St. Mary's Hospital, there are limits to what such measures can do. To provide effective reimbursement benefits with limited resources, the policy of "mere kindness" should be discouraged, and support for the treatment of diseases requiring high-level and high-cost treatments should be expanded. As in developed countries, medical experts must have a pivotal role in determining reimbursement for these diseases. To promote better health for the people, efforts such as appealing to professional opinion should be encouraged. In summary, we believe that the NHI system should be improved to provide increased benefits to patients with severe diseases that currently result in them incurring huge financial burdens because of non-reimbursement.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download