Abstract
Background
All-trans retinoic acid (ATRA)/anthracycline chemotherapy is beneficial in newly diagnosed acute promyelocytic leukemia (APL); however, it is important to identify patients with high-risk disease to increase the cure rate. We investigated the outcome of ATRA/anthracycline chemotherapy and clinicobiological correlations of FLT3/ITD and NPM1 mutations in APL patients.
Methods
Induction therapy included oral ATRA (45 mg/m2/day) and idarubicin (12 mg/m2/day, intravenous, on days 2, 4, and 6). Patients achieving complete remission (CR) received 3 courses of ATRA combined with reinforced consolidation therapy. Mutations were analyzed using GeneScan and polymerasae chain reaction assays of bone marrow samples obtained from patients at diagnosis.
Results
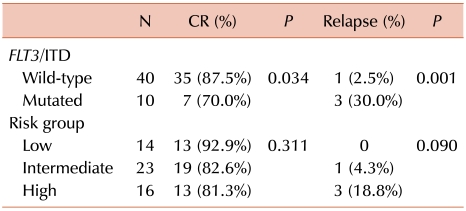
Forty-five (84.9%) of 53 eligible patients achieved CR. The overall relapse rate was 8.9%, and the 3-year overall survival (OS) and leukemia-free survival (LFS) were 84.9±4.9% and 77.5±6.0%, respectively. The NPM1 mutation was not found in any patient, while the FLT3/ITD mutation was found in 10 (20.0%) patients. Of the FLT3/ITD+ patients, 80% belonged to the high-risk group, defined according to the presenting WBC and platelet counts. Among the patients who achieved CR, those who were FLT3/ITD+ had a higher relapse rate than those FLT3/ITD-. FLT3/ITD+ patients also had a significantly lower 3-year LFS than FLT3/ITD- patients. Multivariate analysis of the LFS showed that the FLT3/ITD mutation was independently associated with a shorter overall LFS, after adjusting for pretreatment risk stratification.
Go to : 
Most patients with acute promyelocytic leukemia (APL) are now successfully treated with all-trans retinoic acid (ATRA) and anthracycline-based chemotherapy as first line therapy. A randomized study comparing the simultaneous administration of ATRA and anthracycline chemotherapy with the sequential administration of these therapeutic agents revealed that the former was more effective than the latter [1]. The complete remission (CR) rates were 92% in both study arms, but the relapse rate at 2 years was 6% in the ATRA plus chemotherapy group versus 16% in the sequential group.
While the survival in most APL patients treated with ATRA plus chemotherapy is excellent, relapse or failure to achieve molecular remission is observed in 20-30% patients [2]. Several pretreatment characteristics of APL patients have been identified as having prognostic value [3]. Among them, the presenting white blood cell (WBC) count has the highest impact on the patient outcome [4].
The cooperative group PETHEMA (Programa de Estudio y Tratamiento de las Hemopatías Maligna) reported a risk-adapted treatment strategy of combining ATRA and anthracycline monochemotherapy for both induction and consolidation, followed by maintenance with ATRA and low-dose methotrexate and mercaptopurine [5, 6]. With the previously used treatment regimen, the number of deaths during induction and the relapse rates were higher in patients having an elevated WBC [4]. Therefore, PETHEMA recommended risk stratification based on the WBC and platelet counts at presentation (low-risk group, presenting WBC count of ≤10×109/L and platelet count of >40×109/L; intermediate-risk group, presenting WBC of ≤10×109/L and platelets ≤40×109/L; and high-risk group: presenting WBC count of >10×109/L). Recently, the French APL 2000 and PETHEMA 99 trials showed that a cytarabine-containing regimen resulted in a better CR rate and longer survival in patients with a high WBC count at presentation [7].
FLT3 belongs to the class III receptor tyrosine kinase family. It is expressed in early hematopoietic progenitors, and its dimerization by the FLT3 ligand induces growth-control signals in normal hematopoiesis. The gene encoding FLT3 maps to chromosome band 13q12 [8], and an internal tandem duplication (ITD) of the gene (FLT3/ITD) is detected in 20-30% of young adults with acute myeloid leukemia (AML) [9]. The duplication involves a segment of the juxtamembrane-domain coding sequence, which is always inframe and frequently involves exon 14 and rarely intron 14 or exon 15 [9]. FLT3/ITD from AML patients has been shown to induce autonomous proliferation in cytokine-dependent cell lines; this finding supports the potential role of this mutation in leukemogenesis. AML patients with an isolated FLT3/ITD mutation have poor clinical outcomes, similar to those with poor-risk cytogenetic features [9-11]. Recent reports suggest that quantitative analysis of FLT3/ITD mutation status may be useful to predict the prognosis [10, 12] and assess the minimal residual disease [13] in AML patients.
The frequency of the FLT3/ITD mutation varies dramatically across cytogenetically and molecularly defined subsets of AML and is particularly prevalent in patients with t(15;17) [14-16]. Although previous studies on APL patients have revealed that the FLT3/ITD mutation is associated with an elevated presenting WBC count, hypogranular variant (M3v) morphology, and the short (bcr3) isoform of PML-RARA, the prognostic significance of FLT3 mutations in APL has not been firmly established [14].
The NPM1 gene frequently acts as a target of chromosomal translocations and causes the cytoplasmic dislocation of proteins in various hematological malignancies, thereby indicating its role in malignant transformation. Mutations in NPM1 exon-12 are found in approximately 35% of adult AML patients, and AML with the NPM1 mutation is preferentially associated with monocytic differentiation, lack of CD34, normal cytogenetics, FLT3 gene mutations, and tendency to a favorable clinical outcome [17]. In previous studies, however, NPM1 mutations were not detected in APL patients [18, 19].
In this study, we assessed the treatment outcome of combined ATRA/anthracycline chemotherapy administered as induction and consolidation chemotherapy in APL patients and investigated a series of uniformly treated APL patients to identify the prognostic relevance of various factors present at diagnosis.
Go to : 
Induction therapy consisted of oral ATRA (45 mg/m2 per day in 2 divided doses), which was maintained for a median 45 days or until complete hematologic remission and idarubicin (12 mg/m2 per day) was administered as an intravenous bolus on days 2, 4, and 6. Unlike the protocol followed in previous studies [5-7], ours did not include administration of idarubicin on day 8; this was to eliminate the risk of severe myelosuppression during the treatment for remission induction. Treatment with ATRA was started as soon as APL was diagnosed on the basis of the morphological criteria. For patients in whom the diagnosis was not confirmed by genetic studies, ATRA treatment was withdrawn, and alternative chemotherapy was administered at the physician's discretion. Patients achieving CR received 3 courses of ATRA (45 mg/m2/d, days 1-15) combined with reinforced consolidation chemotherapy, which consisted of idarubicin (7 mg/m2/d for 4 d), mitoxantrone (10 mg/m2/d for 5 d), and idarubicin (12 mg/m2/d for 2 d). Risk stratification was defined using the WBC and platelet counts at presentation, as described in previous studies [5, 6, 20]. For maintenance therapy, ATRA (45 mg/m2/d, days 1-15) was administered every 3 months for 2 years. As supportive care, platelets were transfused to maintain a platelet count of >30×109/L until resolution of coagulopathy, if any. Once the coagulopathy was under control, platelets were transfused only if the patient had infectious or hemorrhagic manifestations or if the platelet count dropped to below 20×109/L. Patients with active coagulopathy were treated with fresh frozen plasma or cryoprecipitate to maintain the fibrinogen level at >1.5 mg/L and hemostatic levels of coagulation factors.
All patients were confirmed to have t(15;17) or PML-RARA fusion transcript by using conventional cytogenetic techniques or nested reverse transcriptase-polymerase chain reaction (RT-PCR), respectively.
Genomic DNA was extracted from cells, such as cryopreserved mononuclear cells, which were harvested from BM samples by using a QIAamp DNA Blood Mini Kit (QIAGEN, Valencia, CA, USA), according to the manufacturer's protocol. For FLT3/ITD mutational analysis, wild-type FLT3 gene exon 11 and 12 were amplified by genomic PCR using the primers 5'-CAATTTAGGTATGAAAGCC-3' (sense) and 5'-CTTTCAGCATTTTGACGGCAACC-3' (anti-sense). Each reaction contained 2.5 mM dNTP, 2.5 mM MgCl2, 0.5 µM of each primer, and 0.5 U f-Taq polymerase in a total volume of 20 µL. Samples were amplified by initial denaturation at 95℃ for 5 min, followed by 35 cycles of 94℃ for 30 s, 53℃ for 1 min, and 72℃ for 2 min, with a final 10-min extension at 72℃. PCR products (10 µL) were resolved on 6% polyacrylamide gels, stained with ethidium bromide, and photographed under ultraviolet light.
For NPM1 mutational analysis, NPM1 gene exon-12 was amplified by genomic PCR using the primers 5'-TCTGAGTAT AAATTTTCTTGGAGTCA-3' (sense) and 5'-ACCAAGCAAA GGGTGGAGTT-3' (anti-sense). The reaction contained 1.25 pmol of each primer, 50 ng genomic DNA, 250 µM dNTPs, and 0.5 U f-Taq polymerase (SolGent, Daejeon, Korea) in the buffer provided by the manufacturer. Amplification was performed with a PTC 200 thermal cycler (MJ Research, Waltham, MA, USA). The PCR fragments were purified using the GeneAll PCR Purification Kit (General Biosystem, Seoul, Korea). Sequencing reactions were analyzed using an ABI 3100 sequencer and BigDye Terminator kit (Applied Biosystems, Foster City, CA, USA).
CR was defined as per the criteria recommended previously [21]. Relapse was defined as the reappearance of blasts after CR in peripheral blood or BM. Leukemia-free survival (LFS) end points, measured from the date of documented CR, included relapse, patient death from any cause, and alive in CR at last follow-up (censored). The overall survival (OS) end points, measured from the date of diagnosis, were death from any cause and alive at last follow-up (censored) [21].
For intergroup comparisons, Fisher's exact test (categorical data) and the Mann-Whitney U-test (continuous data) were used. OS and LFS were analyzed using Kaplan-Meier survival curve estimates and log-rank tests to compare the differences between the distributions of survival in the patient groups. Multivariate analysis using forward conditional selection of variables was performed using Cox's proportional-hazards model. A P-value of less than 0.05 was considered to indicate statistical significance. All statistical computations were performed using the SPSS software (ver. 18.0; SPSS, Chicago, IL, USA).
Go to : 
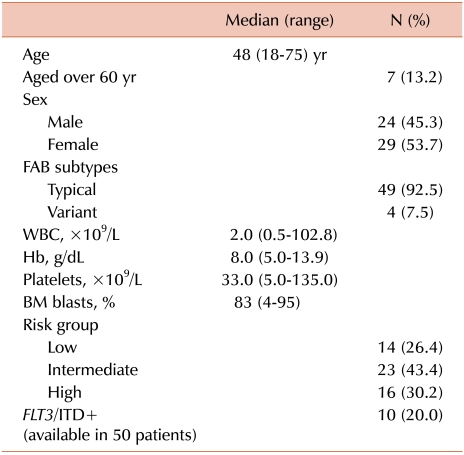
The median age of the 53 APL patients was 48 years (range, 18-75 years), with 7 patients being over 60 years. Low-, intermediate-, and high-risk groups, according to the risk stratification, accounted for 26.4%, 43.4%, and 30.2% of the cases, respectively (Table 1). All patients had received intensive remission-induction chemotherapy. The median follow-up period was 30.8 months (range, 0.2-73.6 months).
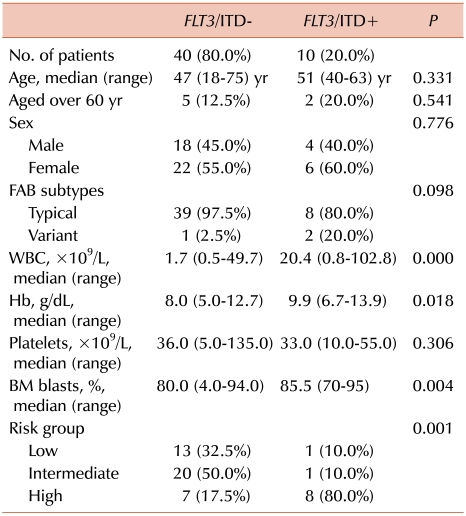
BM samples of 50 patients were evaluated for NPM1 and FLT3/ITD mutations. No NPM1 mutation was found in any patient, while FLT3/ITD mutations were detected in 10 patients (20.0%). Details of the presenting features of FLT3/ITD+ patients are provided in Table 2. The median peripheral WBC count at diagnosis was significantly higher in FLT3/ITD+ patients than in FLT3/ITD- patients (P<0.001). The number of BM blasts was also higher in FLT3/ITD+ patients than in FLT3/ITD- patients (P=0.004). Of the FLT3/ITD+ patients, 80% belonged to the high-risk group (P=0.001; Table 2).
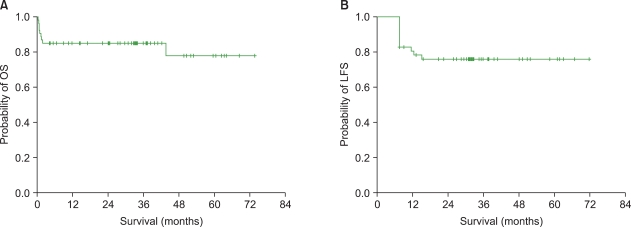
Of the 53 eligible patients, 45 (84.9%) achieved CR. One patient (1.9%) showed resistance to induction chemotherapy, and the remaining 7 (13.2%) died during the induction chemotherapy. Of the 7 early deaths, 3 were due to the differentiation syndrome and 4 due to cerebral or pulmonary hemorrhage. Four (8.9%) patients had clinical relapse 7-15 months after achieving CR. The 3-year Kaplan-Meier estimates of OS and LFS were 84.9±4.9% and 77.5±6.0%, respectively (Fig. 1). Patients with the hypogranular variant subtype did not show a significant difference in the treatment outcomes.
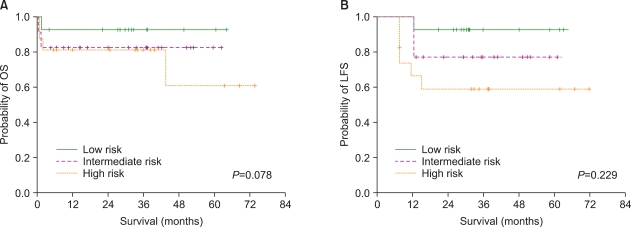
With induction chemotherapy, the high-risk group, defined using the WBC and platelet counts at presentation, had a lower rate of remission compared to the intermediate- and low-risk groups; however, the difference was not statistically significant (81.3% vs. 82.6% vs. 92.9%, respectively; P=0.311; Table 3). Furthermore, a trend to a higher rate of relapse was observed in the high-risk group than in the other risk groups, but the difference was not significant (18.8% vs. 4.3% vs. 0%; P=0.090; Table 3). The high-risk group showed a trend to a lower 3-year LFS (60.0% vs. 77.1% vs. 92.9%; P=0.229) than the intermediate- and low-risk groups (Fig. 2).
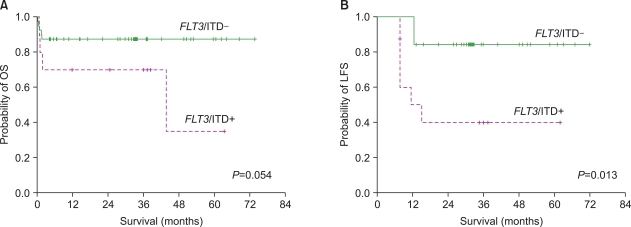
A significant difference was noted between the remission rates achieved by induction chemotherapy in patients with and without FLT3/ITD mutations (70.0% vs. 87.5%; P=0.034; Table 3). Among the patients who achieved CR, the FLT3/ITD+ group had a higher relapse rate than the FLT3/ITD- group (30.0% vs. 2.5%; P=0.001). The former also had a significantly lower 3-year LFS than the latter (44.4%, vs. 84.4%; P=0.013). The FLT3/ITD+ group tended to have a lower 3-year OS than the FLT3/ITD- group (70.0%. vs. 87.5%; P=0.054; Fig. 3), although the difference was not significant.
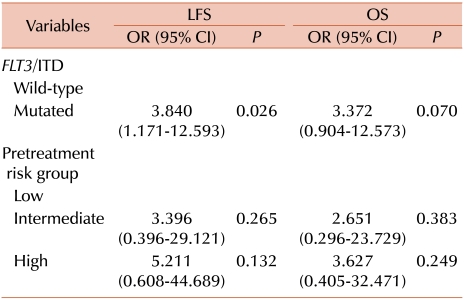
Multivariate analysis of the LFS revealed that the FLT3/ITD mutation was independently associated with a shorter LFS, after adjusting for pretreatment risk stratification (vs. FLT3/ITD-, odds ratio, OR=3.840; P=0.026; Table 4).
Go to : 
Because the use of the induction regimen with combined ATRA and anthracycline chemotherapy resulted in high CR rates and good disease-free survival (DFS), the inclusion of cytarabine in addition to daunorubicin or idarubicin for APL patients is considered to have no impact on the treatment outcome [20]. Thus, since many years, ATRA combined with anthracycline monochemotherapy has been used as a standard treatment for APL. In this study, we assessed the clinical outcome of APL patients treated with ATRA combined with anthracycline chemotherapy.
Previous studies on the use of combined ATRA and chemotherapy without cytarabine for the treatment for newly diagnosed APL showed CR rates ranging from 81 to 95% [1, 20]; the CR rate in this study was 84.9%. Because only 1 patient showed resistance to the induction chemotherapy regimen, the inferior treatment outcome of our study seemed to result from the high rates of early death during the induction chemotherapy due to fatal bleeding or differentiation syndrome; this suggests that early awareness and management of such complications are important.
This study also demonstrated that the patients in the high-risk group, based on the WBC and platelet counts at presentation, tended to have poorer clinical outcomes, such as lower CR rates, higher relapse rates, and shorter LFS, as compared to those in the low- or intermediate-risk groups; however, the difference between the groups was not statistically significant.
In this series of APL patients, we evaluated the prevalence and clinical impact of NPM1 and FLT3/ITD mutations. As was the case in previous studies [18, 19], none of the 50 patients evaluated in this study harbored the NPM1 mutation, while 20% exhibited FLT3/ITD mutations. The reported frequency of FLT3/ITD mutations varies among studies, from 12 to 38% [22-25]. In comparison with the data from Western countries, the reported incidence of FLT3/ITD mutations in APL patients is lower in Asian countries such as in Japan and Taiwan (20 and 21%) [24, 25]. For Korea, one study on the prevalence of FLT3/ITD mutations in APL patients reported a prevalence of 12% [22]; the results obtained in this study were similar to those reported from other Asian countries. The striking differences in the relative incidence of FLT3/ITD between APL patients in Europe/North America and Asia are noteworthy, and the significantly varying propensity for the disease to develop in different ethnic groups [23] suggests that genetic and/or environmental influences play a role in the pathogenesis of APL.
While the prognostic implications of the FLT3/ITD mutation status in cytogenetically normal AML are well described [9-11], the prognostic relevance of this mutation in APL patients is less clear. The current literature on the effect of FLT3 mutations on the outcome in APL is conflicting. Some studies found that the FLT3 status did not result in any apparent difference in DFS [14], whereas others reported that FLT3/ITD mutations were associated with a tendency towards [26, 27] or significantly inferior [28] LFS. In our study, an association between the FLT3/ITD mutation and elevated presenting WBC and BM blast counts was noted in APL patients. A previous study indicated that FLT3 alterations in APL are associated with more aggressive clinical features and suggested that these lesions may not play a major role in leukemia progression [26]. However, in vitro studies of small-molecule FLT3 inhibitors have shown that they can suppress the survival and proliferation of FLT3/ITD+ AML blast cells [29, 30]. In our study, patients carrying this mutation had a lower CR rate, higher rate of relapse, and shorter LFS and OS than those without this mutation. Although the FLT3/ITD mutation was associated with high WBC and BM blast counts at presentation, multivariate analysis showed that this mutation was an independent predictor of LFS in APL patients.
In summary, our study examined the clinical outcome of combined ATRA and anthracycline chemotherapy in newly diagnosed APL patients. Patients with FLT3/ITD mutations showed more aggressive clinical features. Further, the FLT3/ITD mutation at diagnosis characterizes a small subgroup of patients with extremely poor prognosis. Thus, to increase the cure rates, it would be helpful to identify patients with high-risk disease, such as those carrying FLT3/ITD mutations, who could benefit from treatment modification, including the addition of cytarabine or FLT3 inhibitors.
Go to : 
Notes
This work was supported by a research grant from the Korea Health 21 R&D Project, Ministry of Health and Welfare, Republic of Korea (A010385) and the Research Institute of Medical Sciences, Chonnam National University (2007-CURIMS-DR007).
Go to : 
References
1. Fenaux P, Chastang C, Chevret S, et al. A randomized comparison of all transretinoic acid (ATRA) followed by chemotherapy and ATRA plus chemotherapy and the role of maintenance therapy in newly diagnosed acute promyelocytic leukemia. Blood. 1999; 94:1192–1200. PMID: 10438706.

2. Wang ZY, Chen Z. Acute promyelocytic leukemia: from highly fatal to highly curable. Blood. 2008; 111:2505–2515. PMID: 18299451.

3. Mistry AR, Pedersen EW, Solomon E, Grimwade D. The molecular pathogenesis of acute promyelocytic leukaemia: implications for the clinical management of the disease. Blood Rev. 2003; 17:71–97. PMID: 12642121.

4. Burnett AK, Grimwade D, Solomon E, Wheatley K, Goldstone AH. Presenting white blood cell count and kinetics of molecular remission predict prognosis in acute promyelocytic leukemia treated with all-trans retinoic acid: result of the randomized MRC trial. Blood. 1999; 93:4131–4143. PMID: 10361110.

5. Sanz MA, Lo Coco F, Martín G, et al. Definition of relapse risk and role of nonanthracycline drugs for consolidation in patients with acute promyelocytic leukemia: a joint study of the PETHEMA and GIMEMA cooperative groups. Blood. 2000; 96:1247–1253. PMID: 10942364.
6. Sanz MA, Martín G, González M, et al. Risk-adapted treatment of acute promyelocytic leukemia with all-trans-retinoic acid and anthracycline monochemotherapy: a multicenter study by the PETHEMA group. Blood. 2004; 103:1237–1243. PMID: 14576047.

7. Adés L, Sanz MA, Chevret S, et al. Treatment of newly diagnosed acute promyelocytic leukemia (APL): a comparison of French-Belgian-Swiss and PETHEMA results. Blood. 2008; 111:1078–1084. PMID: 17975017.
8. Rosnet O, Schiff C, Pébusque MJ, et al. Human FLT3/FLK2 gene: cDNA cloning and expression in hematopoietic cells. Blood. 1993; 82:1110–1119. PMID: 8394751.

9. Kottaridis PD, Gale RE, Frew ME, et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood. 2001; 98:1752–1759. PMID: 11535508.

10. Gale RE, Green C, Allen C, et al. The impact of FLT3 internal tandem duplication mutant level, number, size, and interaction with NPM1 mutations in a large cohort of young adult patients with acute myeloid leukemia. Blood. 2008; 111:2776–2784. PMID: 17957027.

11. Colovic N, Tosic N, Aveic S, et al. Importance of early detection and follow-up of FLT3 mutations in patients with acute myeloid leukemia. Ann Hematol. 2007; 86:741–747. PMID: 17579862.

12. Kang HJ, Lee JW, Kho SH, et al. High transcript level of FLT3 associated with high risk of relapse in pediatric acute myeloid leukemia. J Korean Med Sci. 2010; 25:841–845. PMID: 20514303.

13. Chou WC, Hou HA, Liu CY, et al. Sensitive measurement of quantity dynamics of FLT3 internal tandem duplication at early time points provides prognostic information. Ann Oncol. 2011; 22:696–704. PMID: 20693296.

14. Kainz B, Heintel D, Marculescu R, et al. Variable prognostic value of FLT3 internal tandem duplications in patients with de novo AML and a normal karyotype, t(15;17), t(8;21) or inv(16). Hematol J. 2002; 3:283–289. PMID: 12522450.

15. Moreno I, Martín G, Bolufer P, et al. Incidence and prognostic value of FLT3 internal tandem duplication and D835 mutations in acute myeloid leukemia. Haematologica. 2003; 88:19–24. PMID: 12551822.
16. Chillón MC, Fernández C, García-Sanz R, et al. FLT3-activating mutations are associated with poor prognostic features in AML at diagnosis but they are not an independent prognostic factor. Hematol J. 2004; 5:239–246. PMID: 15167911.

17. Falini B, Mecucci C, Tiacci E, et al. Cytoplasmic nucleophosmin in acute myelogenous leukemia with a normal karyotype. N Engl J Med. 2005; 352:254–266. PMID: 15659725.

18. Chen W, Rassidakis GZ, Medeiros LJ. Nucleophosmin gene mutations in acute myeloid leukemia. Arch Pathol Lab Med. 2006; 130:1687–1692. PMID: 17076533.

19. Thiede C, Koch S, Creutzig E, et al. Prevalence and prognostic impact of NPM1 mutations in 1485 adult patients with acute myeloid leukemia (AML). Blood. 2006; 107:4011–4020. PMID: 16455956.

20. Sanz MA, Martín G, Rayón C, et al. A modified AIDA protocol with anthracycline-based consolidation results in high antileukemic efficacy and reduced toxicity in newly diagnosed PML/RARalpha-positive acute promyelocytic leukemia. Blood. 1999; 94:3015–3021. PMID: 10556184.
21. Cheson BD, Bennett JM, Kopecky KJ, et al. Revised recommendations of the International Working Group for diagnosis, standardization of response criteria, treatment outcomes, and reporting standards for therapeutic trials in acute myeloid leukemia. J Clin Oncol. 2003; 21:4642–4649. PMID: 14673054.

22. Yoo SJ, Park CJ, Jang S, Seo EJ, Lee KH, Chi HS. Inferior prognostic outcome in acute promyelocytic leukemia with alterations of FLT3 gene. Leuk Lymphoma. 2006; 47:1788–1793. PMID: 17064989.
23. Beitinjaneh A, Jang S, Roukoz H, Majhail NS. Prognostic significance of FLT3 internal tandem duplication and tyrosine kinase domain mutations in acute promyelocytic leukemia: a systematic review. Leuk Res. 2010; 34:831–836. PMID: 20096459.

24. Kiyoi H, Naoe T, Yokota S, et al. Internal tandem duplication of FLT3 associated with leukocytosis in acute promyelocytic leukemia. Leukemia. 1997; 11:1447–1452. PMID: 9305596.

25. Shih LY, Kuo MC, Liang DC, et al. Internal tandem duplication and Asp835 mutations of the FMS-like tyrosine kinase 3 (FLT3) gene in acute promyelocytic leukemia. Cancer. 2003; 98:1206–1216. PMID: 12973844.
26. Noguera NI, Breccia M, Divona M, et al. Alterations of the FLT3 gene in acute promyelocytic leukemia: association with diagnostic characteristics and analysis of clinical outcome in patients treated with the Italian AIDA protocol. Leukemia. 2002; 16:2185–2189. PMID: 12399960.

27. Au WY, Fung A, Chim CS, et al. FLT-3 aberrations in acute promyelocytic leukaemia: clinicopathological associations and prognostic impact. Br J Haematol. 2004; 125:463–469. PMID: 15142116.

28. Callens C, Chevret S, Cayuela JM, et al. Prognostic implication of FLT3 and Ras gene mutations in patients with acute promyelocytic leukemia (APL): a retrospective study from the European APL Group. Leukemia. 2005; 19:1153–1160. PMID: 15889156.

29. Yee KW, Schittenhelm M, O'Farrell AM, et al. Synergistic effect of SU11248 with cytarabine or daunorubicin on FLT3 ITD-positive leukemic cells. Blood. 2004; 104:4202–4209. PMID: 15304385.

30. Gale RE, Hills R, Pizzey AR, et al. Relationship between FLT3 mutation status, biologic characteristics, and response to targeted therapy in acute promyelocytic leukemia. Blood. 2005; 106:3768–3776. PMID: 16105978.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download