Abstract
Macrolides have both immunomodulatory and antibacterial effects. We report 3 cases of primary immune thrombocytopenia (ITP) patients who were successfully treated with macrolides, irrespective of Helicobacter pylori (H. pylori) infection status. Case 1, an 88-year-old woman who was an H. pylori-positive ITP patient, was treated with clarithromycin (CAM). CAM was effective temporarily. As an alternative to CAM, she was successfully treated with erythromycin (EM) for more than 7 months. Case 2, a 61-year-old man who was an H. pylori-negative ITP patient, was unsuccessfully treated with CAM but successfully treated with EM. Case 3, a 75-year-old woman who was a H. pylori-negative ITP patient, was treated with CAM. CAM was effective temporarily. After approximately 6 months, she was treated with EM for a common cold, and her platelet count increased rapidly. Based on these findings, macrolide treatment was effective for ITP. The effectiveness of macrolides might suggest immunomodulatory effects as well as antibacterial effects for H. pylori.
Macrolides have both immunomodulatory effects and antibacterial effects against organisms such as Helicobacter pylori (H. pylori) [1-3]. We have already reported 3 cases of idiopathic thrombocytic purpura (ITP), also known as primary immune thrombocytopenia, which show increased platelet counts following clarithromycin (CAM) treatment, irrespective of H. pylori infection status [4]. ITP is an autoimmune disease induced by autoantibodies against platelets. In our previous report, the fact that platelet count normalized following CAM treatment suggested immunomodulatory effects of macrolides. Erythromycin (EM) was the first macrolide to be developed and showed poor activity against bacteria compared with new macrolides such as CAM, which has been developed to supersede EM [3]. We report 3 cases of ITP that were successfully treated with macrolides. In these cases, EM was considered more effective than CAM.
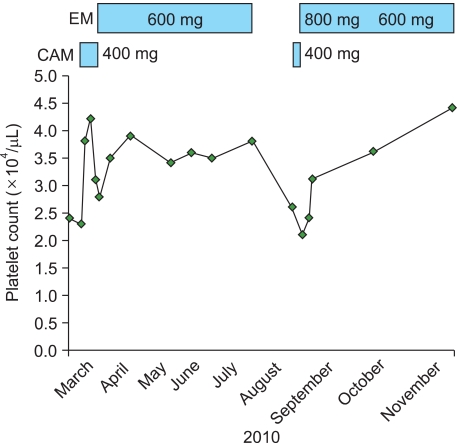
An 88-year-old woman who had been suffering from ITP for several years was admitted for resection of a small tumor of the tongue. Platelet count remained at a level of around 20×109/L. Initial laboratory data showed reduced platelet counts (24×109/L). The patient was referred to our department for management of platelet count, which needed to be increased to about 50×109/L before tumor resection. Although a positive result was obtained for anti-H. pylori IgG antibodies, the patient could not be treated by eradication therapy because of an allergy to penicillins. As the patient was suffering from osteoporosis and refused platelet transfusion, she was treated using CAM without prednisolone (PSL). The clinical course is shown in Fig. 1. CAM was given at 400 mg/day. Platelet count had increased to 42×109/L by 5 days after CAM treatment and then resection was safely performed. Little bleeding was seen during and after resection. After resection, the platelet count had decreased to 28×109/L despite CAM treatment. The patient was treated with EM at a dose of 600 mg/day as an alternative to CAM. The platelet count had increased to 35×109/L by 7 days after starting EM treatment. After the patient was discharged, the platelet count remained at about 34-39×109/L. We tried stopping EM prescriptions for 1 month, but the platelet count decreased to 26×109/L. Re-treatment with CAM did not improve the platelet count, so she was re-treated using EM at a dose of 800 mg/day instead of CAM. After 1 week, platelet count increased from 21×109/L to 31×109/L. The dose of EM was therefore reduced to 600 mg/day. By the end of the observation period, platelet count had increased to 44×109/L.
A 61-year-old man was referred with purpura, which had appeared several months before. Initial laboratory data showed a reduced platelet count (14×109/L), so he was admitted for further investigation. Anti-nuclear antibody was positive (titer 1:640, speckled). Testing for anti-dsDNA antibody, anti-SSA antibody, anti-RNP antibody, anti-Sm antibody, and anti-Topo I antibody all yielded negative results, as did testing for anti-H. pylori IgG antibody. A bone marrow specimen revealed hyperplasia of normal megakaryocytes. Neither articular swelling nor skin rash suggestive of collagen disease was present. Based on clinical and laboratory findings, ITP was diagnosed. The clinical course is shown in Fig. 2. PSL was given at 60 mg/day for 4 days, but the platelet count still decreased to 6×109/L. Methylprednisolone pulse therapy was therefore performed and PSL reduced to 30 mg/day because of hyperglycemia. By 1 week after pulse therapy, platelet count had only increased to 20×109/L. The patient was treated with CAM at a dose of 400 mg/day after obtaining informed consent. About 4 weeks after treatment for ITP, platelet count did not increase and remained at 17×109/L. The patient was therefore administered EM at 600 mg/day as an alternative to CAM. After 2 weeks, platelet count increased to 77×109/L and oral PSL could be gradually tapered. By the end of the observation period, platelet count increased to 208×109/L.
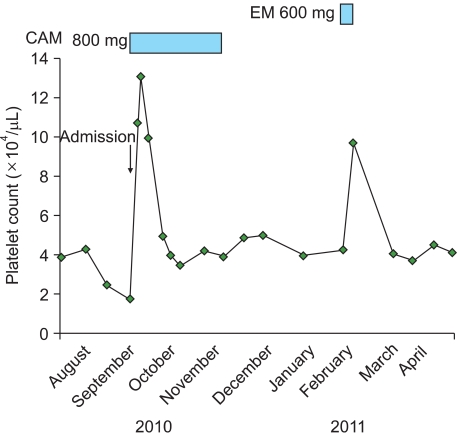
A 75-year-old woman suffering from ITP was admitted with a gradual decrease in platelet count. Prior to admission, platelet count had remained at a level of around 40×109/L. Laboratory data on admission showed reduced platelet counts (18×109/L). Anti-H. pylori IgG antibody and urea breath tests were negative. The clinical course is shown in Fig. 3. CAM was given at 800 mg/day after informed consent was obtained. Platelet count had rapidly increased to 131×109/L by 7 days after CAM treatment. However, after 1 month, platelet count had decreased to 40×109/L despite CAM treatment. Because liver dysfunction occurred, we stopped prescribing CAM. After the patient was discharged, the platelet count remained at about 35-50×109/L without medication. The patient was treated with EM at a dose of 600 mg/day for a common cold. After 1 week, platelet count had increased from 43×109/L to 97×109/L. Because the patient recovered from the cold, EM prescription was stopped. After 1 month, the platelet count had decreased to 41×109/L. By the end of the observation period, platelet count had remained at a level of around 40×109/L without medication.
In Case 1, CAM treatment appeared to be effective temporarily. Re-treatment with CAM proved ineffective. Although the platelet count remained at only about 31-44×109/L with EM treatment, including re-treatment, EM was considered more effective than CAM.
ITP is an autoimmune disease induced by autoantibodies against platelets. Recent studies have suggested that ITP patients infected with H. pylori can be successfully treated by eradication (proton pump inhibitors, amoxicillin, and CAM) [5, 6]. In Case 1, platelet counts might have increased as a result of the antibacterial effects of macrolides against H. pylori. However, the higher effectiveness of EM compared with CAM could not be explained, as CAM generally shows superior activity against H. pylori compared with EM [4]. This effectiveness might suggest the superiority of EM to CAM with regard to immunomodulatory effects independent of infection. Possibly this decrease in platelet count, despite CAM treatment, might suggest side effects of CAM.
In general, platelet count increases within 4 weeks of starting PSL treatment. Similarly, platelet count increases 3-5 days after starting methylprednisolone pulse therapy. Steroid therapy in Case 2 thus appeared largely ineffective.
As CAM treatment only maintained platelet count, CAM was not considered sufficiently effective in Case 2. However, EM was clearly effective, as could be seen by gradual improvements in platelet counts.
In Case 2, EM treatment was effective for an H. pylori-negative ITP patient. The pathogenesis of H. pylori-negative ITP is thought to involve autoimmunity derived from EM-sensitive bacteria other than H. pylori, or immunological dysregulation independent of infection.
In Case 3, CAM treatment appeared to be effective temporarily. The cause of the decrease in platelet count, despite CAM treatment, might suggest that CAM has side effects, as in Case 1.
The fact that EM treatment for a common cold increased the platelet count also suggests the effectiveness of EM for ITP.
In our previous report and in this report, the fact that platelet count increased following macrolide treatment suggests immunomodulatory effects of macrolides.
Immunomodulatory effects from macrolide antibiotics might be obtained by the eradication of bacteria or by modulation of the immune system involving the mucosa on which commensal bacteria reside [7]. Alternatively, these effects might be pharmacological functions of the macrolide itself, independent of antibiotic effects.
Apart from antibacterial effects, macrolides have effects on neutrophil function (decreased oxidant production, apoptosis) and on the production of cytokines involved in the inflammation cascade (decreased production of IL-1, IL-6, IL-8, and TNF and increased production of IL-10 and, possibly, IL-4) [1]. With regard to T lymphocytes, EM and its derivatives inhibit T lymphocyte proliferation and induce T lymphocyte apoptosis [2].
Apart from these immunomodulatory effects, macrolides have steroid-sparing effects via their influence on corticosteroid metabolism [8]. In Case 2, steroid-sparing effects might increase the platelet count.
EM was the first macrolide to be developed. New macrolides such as CAM and azithromycin have since been developed to supersede EM. CAM is a semisynthetic macrolide antibiotic, chemically identified as 6-0-methylerythromycin A [9]. A close analogy exists between CAM and EM. However, in the present report, although only 3 cases were studied, macrolides proved effective for ITP, as in our previous report, and EM was considered more effective than CAM.
As a slight structural change is thought to be advantageous to CAM in terms of antibacterial effects, similarly, a slight change may be advantageous to EM for providing immunomodulatory effects.
For the purpose of clarifying which macrolide is more effective, crossover tests between EM and CAM are needed in the future.
References
1. Labro MT. Anti-inflammatory activity of macrolides: a new therapeutic potential? J Antimicrob Chemother. 1998; 41(Suppl B):37–46. PMID: 9579711.

2. Wu L, Zhang W, Tian L, Bao K, Li P, Lin J. Immunomodulatory effects of erythromycin and its derivatives on human T-lymphocyte in vitro. Immunopharmacol Immunotoxicol. 2007; 29:587–596. PMID: 18075867.
3. Blondeau JM, DeCarolis E, Metzler KL, Hansen GT. The macrolides. Expert Opin Investig Drugs. 2002; 11:189–215.
4. Ohe M, Kohno M. Three cases of idiopathic thrombocytopenic purpura showing an increase in the platelet count following clarithromycin treatment. Rinsho Ketsueki. 2003; 44:1044–1046. PMID: 14639954.
5. Gasbarrini A, Franceschi F, Tartaglione R, Landolfi R, Pola P, Gasbarrini G. Regression of autoimmune thrombocytopenia after eiradication of Helicobacter pylori. Lancet. 1998; 352:878. PMID: 9742983.
6. Hashino S, Mori A, Suzuki S, et al. Platelet recovery in patients with idiopathic thrombocytopenic purpura after eradication of Helicobacter pylori. Int J Hematol. 2003; 77:188–191. PMID: 12627857.

7. Tlaskalova-Hogenova H, Stepankova R, Hudcovic T, et al. Commensal bacteria (normal microflora), mucosal immunity and chronic inflammatory and autoimmune diseases. Immunol Lett. 2004; 93:97–108. PMID: 15158604.
8. Rubin BK, Henke MO. Immunomodulatory activity and effectiveness of macrolides in chronic airway disease. Chest. 2004; 125(Suppl 2):S70–S85.

9. Iwasaki H, Sugawara Y, Adachi T, Morimoto S, Watanabe Y. Structure of 6-0-methylerythromycin A (clarithromycin). Acta Cryst. 1993; C49:1227–1230.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download