1. Weatherall DJ. Hoffbrand AV, Lewis SM, Tuddenham EG, editors. Genetic disorders of haemoglobin. Postgrauate haematology. 1999. 4th ed. Oxford, UK: Butterworth-Heinemann;p. 91–119.
2. Wood WG. Increased HbF in adult life. Baillieres Clin Haematol. 1993; 6:177–213. PMID:
7688998.
3. Kan YW, Holland JP, Dozy AM, Charache S, Kazazian HH. Deletion of the beta-globin structure gene in hereditary persistence of foetal haemoglobin. Nature. 1975; 258:162–163. PMID:
1186896.
4. Kotila TR, Fawole OI, Shokunbi WA. Haemoglobin F and clinical severity of sickle cell anaemia among Nigerian adults. Afr J Med Med Sci. 2000; 29:229–231. PMID:
11713996.
5. Harmening DM, Lasky L, Latchaw P. Harmening DM, editor. Blood preservation: historical perspectives, review of metabolism and current trends. Modern blood banking and transfusion practices. 1999. 4th ed. Philadelphia, PA: F.A. Davis co..
6. Cheesbrough M, editor. District laboratory practice in Tropical Countries, Part 1. 2006. 2nd ed. Cambridge, UK: Cambridge University press;p. 268–285.
7. Kleihauer E, Braun H, Betke K. Dacie JV, Lewis SM, editors. Erythrocyte and leukocyte cytochemistry-leukaemia classification. Practical haematology. 2001. 9th ed. London, UK: Curchill Livingstone;p. 269–295.
8. Hoffbrand AV, Pettit JE, Moss PAH. Essential haematology. 2001. 4th ed. Oxford, UK: Blackwell Science;p. 71–90.
9. Bunn HF. Stamatoyannopoulos G, Nienhuis AW, Majerus PW, Varmus H, editors. Sickle hemoglobin and other hemoglobin mutants. The molecular basis of blood diseases. 1994. 2nd ed. Philadelphia, PA: W.B. Saunders;p. 207–256.
10. Corda M, De Rosa MC, Pellegrini MG, et al. Adult and fetal haemoglobin J-Sardegna [alpha50(CE8)His→Asp]: functional and molecular modelling studies. Biochem J. 2000; 346:193–199. PMID:
10657257.
11. Patrinos GP, Giardine B, Riemer C, et al. Improvements in the HbVar database of human hemoglobin variants and thalassemia mutations for population and sequence variation studies. Nucleic Acids Res. 2004; 32:D537–D541. PMID:
14681476.

12. De Rosa MC, Alinovi CC, Schinina ME, et al. Hb Santa Clara (beta 97His→Asn), a human haemoglobin variant: functional characterization and structure modelling. Biochim Biophys Acta. 2007; 1774:1299–1306. PMID:
17881306.
13. Cheesbrough M, editor. ICSH: International Committee for Standardization in Haematology. Haematological Tests. District laboratory practice in Tropical Countries, Part 1. 1988. Cambridge, UK: Cambridge University press;p. 282–298.
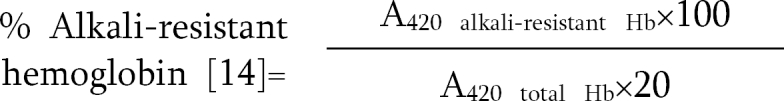
14. Betke K, Mati HR, Schlicht L. Dacie JV, Lewis SM, editors. Investigation of abnormal haemoglobins and thalassaemia. Practical haematology. 2001. 9th ed. London, UK: Curchill Livingstone;p. 231–268.
15. Falusi AG, Esan GJ. Foetal haemoglobin levels in sickle cell anaemia in Nigerians. Afr J Med Med Sci. 1989; 18:145–149. PMID:
2474239.
16. Uko EK, Useh MF, Gwanmesia FN. Frequency of foetal haemoglobin and haemoglobin values in various haemoglobin genotypes in Calabar, Nigeria. East Afr Med J. 1997; 74:809–811. PMID:
9557428.
17. Uda M, Galanello R, Sanna S, et al. Genome-wide association study shows BCL11A associated with persistent fetal hemoglobin and amelioration of the phenotype of beta-thalassemia. Proc Natl Acad Sci U S A. 2008; 105:1620–1625. PMID:
18245381.
18. Sankaran VG, Menne TF, Xu J, et al. Human fetal hemoglobin expression is regulated by the developmental stage-specific repressor BCL11A. Science. 2008; 322:1839–1842. PMID:
19056937.

19. Mason KP, Grandison Y, Hayes RJ, et al. Post-natal decline of fetal haemoglobin in homozygous sickle cell disease: relationship to parenteral Hb F levels. Br J Haematol. 1982; 52:455–463. PMID:
6181802.
20. Maude GH, Hayes RJ, Serjeant G. The haematology of steady state homozygous sickle cell disease: interrelationships between haematological indices. Br J Haematol. 1987; 66:549–558. PMID:
2444245.