1. Pereira MS, Mulloy B, Mourão PA. Structure and anticoagulant activity of sulfated fucans. Comparison between the regular, repetitive, and linear fucans from echinoderms with the more heterogeneous and branched polymers from brown algae. J Biol Chem. 1999; 274:7656–7667. PMID:
10075653.
2. Cumashi A, Ushakova NA, Preobrazhenskaya ME, et al. A comparative study of the anti-inflammatory, anticoagulant, antiangiogenic, and antiadhesive activities of nine different fucoidans from brown seaweeds. Glycobiology. 2007; 17:541–552. PMID:
17296677.

3. Pereira MS, Melo FR, Mourão PA. Is there a correlation between structure and anticoagulant action of sulfated galactans and sulfated fucans? Glycobiology. 2002; 12:573–580. PMID:
12244069.

4. Smorenburg SM, Van Noordan CJ. The complex effects of heparins on cancer progression and metastasis in experimental studies. Pharmacol Rev. 2001; 53:93–105. PMID:
11171940.
5. San Antonio JD, Verrecchio A, Pukac LA. Heparin sensitive and resistant vascular smooth muscle cells: biology and role in restenosis. Connect Tissue Res. 1998; 37:87–103. PMID:
9643650.

6. Matsunaga M, Ohtaki H, Takaki A, et al. Nucleoprotamine diet derived from salmon soft roe protects mouse hippocampal neurons from delayed cell death after transient forebrain ischemia. Neurosci Res. 2003; 47:269–276. PMID:
14568108.

7. Lange RA, Hillis LD. Antiplatelet therapy for ischemic heart disease. N Engl J Med. 2004; 350:277–280. PMID:
14724308.

8. Hirsh J. Hyperactive platelets and complications of coronary artery disease. N Engl J Med. 1987; 316:1543–1544. PMID:
3587283.
9. Casscells W. Migration of smooth muscle and endothelial cells: Critical events in restenosis. Circulation. 1992; 86:723–729. PMID:
1516183.

10. Post MJ, Borst C, Kuntz RE. The relative importance of arterial remodeling compared with intimal hyperplasia in lumen renarrowing after balloon angioplasty. A study in the normal rabbit and the hypercholesterolemic Yucatan micropig. Circulation. 1994; 89:2816–2821. PMID:
8205696.

11. Farrehi PM, Ozaki CK, Carmeliet P, Fay WP. Regulation of arterial thrombolysis by plasminogen activator inhibitor-1 in mice. Circulation. 1998; 97:1002–1008. PMID:
9529269.

12. Mourão PA. Use of sulfated fucans as anticoagulant and antithrombotic agents: future perspectives. Curr Pharm Des. 2004; 10:967–981. PMID:
15078127.
13. Cumashi A, Ushakova NA, Preobrazhenskaya ME, et al. A comparative study of the anti-inflammatory, anticoagulant, antiangiogenic, and antiadhesive activities of nine different fucoidans from brown seaweeds. Glycobiology. 2007; 17:541–552. PMID:
17296677.

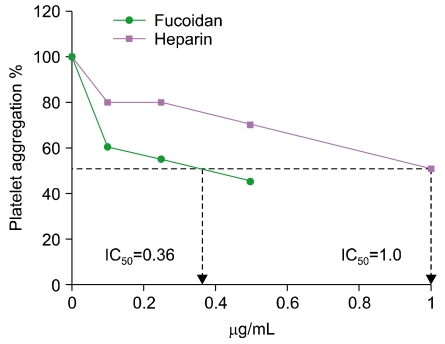
14. Dürig J, Bruhn T, Zurborn KH, Gutensohn K, Bruhn HD, Béress L. Anticoagulant fucoidan fractions from Fucus vesiculosus induce platelet activation in vitro. Thromb Res. 1997; 85:479–491. PMID:
9101640.

15. Alwayn IP, Appel JZ, Goepfert C, Buhler L, Cooper DK, Robson SC. Inhibition of platelet aggregation in baboons: therapeutic implications for xenotransplantation. Xenotransplantation. 2000; 7:247–257. PMID:
11081759.

16. Church FC, Meade JB, Treanor RE, Whinna HC. Antithrombin activity of fucoidan. The interaction of fucoidan with heparin cofactor II, antithrombin III, and thrombin. J Biol Chem. 1989; 264:3618–3623. PMID:
2914965.
17. Nishino T, Nagumo T. Anticoagulant and antithrombin activities of oversulfated fucans. Carbohydr Res. 1992; 229:355–362. PMID:
1394292.

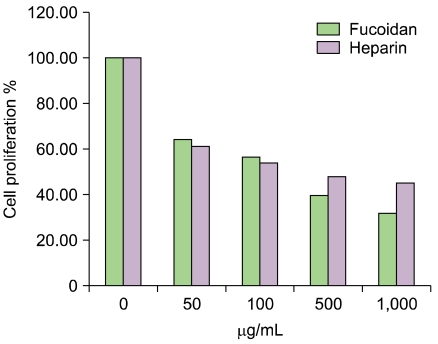
18. Patel MK, Mulloy B, Gallagher KL, O'Brien L, Hughes AD. The antimitogenic action of the sulphated polysaccharide fucoidan differs from heparin in human vascular smooth muscle cells. Thromb Haemost. 2002; 87:149–154. PMID:
11848445.

19. Religa P, Kazi M, Thyberg J, Gaciong Z, Swedenborg J, Hedin U. Fucoidan inhibits smooth muscle cell proliferation and reduces mitogen-activated protein kinase activity. Eur J Vasc Endovasc Surg. 2000; 20:419–426. PMID:
11112459.

20. duPont NC, Wang K, Wadhwa PD, Culhane JF, Nelson EL. Validation and comparison of luminex multiplex cytokine analysis kits with ELISA: determinations of a panel of nine cytokines in clinical sample culture supernatants. J Reprod Immunol. 2005; 66:175–191. PMID:
16029895.

21. Ramsden L, Rider CC. Selective and differential binding of interleukin (IL)-1 alpha, IL-1 beta, IL-2 and IL-6 to glycosaminoglycans. Eur J Immunol. 1992; 22:3027–3031. PMID:
1425926.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download