1. Levine RL, Wadleigh M, Cools J, et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell. 2005; 7:387–397. PMID:
15837627.

2. Jones AV, Kreil S, Zoi K, et al. Widespread occurrence of the JAK2 V617F mutation in chronic myeloproliferative disorders. Blood. 2005; 106:2162–2168. PMID:
15920007.

3. Cho BS, Min CK, Eom KS, et al. Feasibility of NIH consensus criteria for chronic graft-versus-host disease. Leukemia. 2009; 23:78–84. PMID:
18830253.

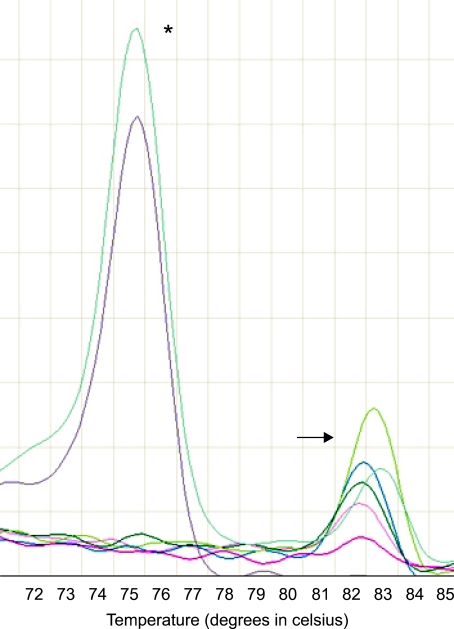
4. Jones AV, Cross NC, White HE, Green AR, Scott LM. Rapid identification of JAK2 exon12 mutations using high resolution melting analysis. Haematologica. 2008; 93:1560–1564. PMID:
18698085.
5. Rapado I, Grande S, Albizua E, et al. High resolution melting analysis for JAK2 Exon 14 and Exon 12 mutations: A diagnostic tool for myeloproliferative neoplasms. J Mol Diagn. 2009; 11:155–161. PMID:
19225136.
6. Swerdlow SH, Campo E, Harris NL, et al. World Health Organization classification of tumors. pathology and genetics of tumours of haematopoietic and lymphoid tissues. 2008. Lyon: IARC Press.
7. Ingram W, Lea NC, Cervera J, et al. The JAK2 V617F mutation identifies a subgroup of MDS patients with isolated deletion 5q and a proliferative bone marrow. Leukemia. 2006; 20:1319–1321. PMID:
16617322.

8. Malcovati L, Porta MG, Pietra D, et al. Molecular and clinical features of refractory anemia with ringed sideroblasts associated with marked thrombocytosis. Blood. 2009; 114:3538–3545. PMID:
19692701.

9. Lee JW, Kim YG, Soung YH, et al. The JAK2 V617F mutation in de novo acute myelogenous leukemias. Oncogene. 2006; 25:1434–1436. PMID:
16247455.

10. Steensma DP, McClure RF, Karp JE, et al. JAK2 V617F is a rare finding in de novo acute myeloid leukemia, but STAT3 activation is common and remains unexplained. Leukemia. 2006; 20:971–978. PMID:
16598306.

11. Vicente C, Vázquez I, Marcotegui N, et al. JAK2-V617F activating mutation in acute myeloid leukemia: Prognostic impact and association with other molecular markers. Leukemia. 2007; 21:2386–2390. PMID:
17581610.

12. Levine RL, Loriaux M, Huntly BJ, et al. The JAK2V617F activating mutation occurs in chronic myelomonocytic leukemia and acute myeloid leukemia, but not in acute lymphoblastic leukemia or chronic lymphocytic leukemia. Blood. 2005; 106:3377–3379. PMID:
16081687.

13. Jelinek J, Oki Y, Gharibyan V, et al. JAK2 mutation 1849>4T is rare in acute leukemias but can be found in CMML, Philadelphia chromosome-negative CML, and megakaryocytic leukemia. Blood. 2005; 106:3370–3373. PMID:
16037387.
14. Döhner K, Du J, Corbacioglu A, Scholl C, Schlenk RF, Döhner H. JAK2V617F mutations as cooperative genetic lesions in t(8;21)-positive acute myeloid leukemia. Haematologica. 2006; 91:1569–1570. PMID:
17043013.
15. Orazi A, Germing U. The myelodysplastic/myeloproliferative neoplasms: myeloproliferaitve diseases with dysplastic features. Leukemia. 2008; 22:1308–1319. PMID:
18480833.
16. Wardrop D, Steensma DP. Is refractory anaemia with ring sideroblasts and thrombocytosis (RARS-T) a necessary or useful diagnostic category? Br J Haematol. 2009; 144:809–817. PMID:
19120370.

17. Boissinot M, Garand R, Hamidou M, Hermouet S. The JAK2-617F mutation and essential thrombocythemia features in a subset of patient with refractory anemia with ring sideroblasts (RARS). Blood. 2006; 108:1781–1782. PMID:
16926301.
18. Schmitt-Graeff AH, Teo SS, Olschewski M, et al. JAK2V617F mutation status identifies subtypes of refractory anemia with ringed sideroblasts associated with marked thrombocytosis. Haematologica. 2008; 93:34–40. PMID:
18166783.

19. Skoda RC. Thrombocytosis. Hematology Am Soc Hematol Educ Program. 2009. p. 159–167.

20. Basquiera AL, Soria NW, Ryser R, et al. Clinical significance of V617F mutation of the JAK2 gene in patients with chronic myeloproliferative disorders. Hematology. 2009; 14:323–330. PMID:
19941738.

21. Raya JM, Arenillas L, Domingo A, et al. Refractory anemia with ringed sideroblasts associated with thrombocytosis: comparative analysis of marked with non-marked thrombocytosis, and relationship with JAK2 V617F mutational status. Int J Hematol. 2008; 88:387–395. PMID:
18820995.

22. Millecker L, Lennon PA, Verstovsek S, et al. Distinct patterns of cytogenetic and clinical progression in chronic myeloproliferative neoplasms with or without JAK2 or MPL mutations. Cancer Genet Cytogenet. 2010; 197:1–7. PMID:
20113830.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download