Abstract
Background
An early diagnosis of disseminated intravascular coagulation (DIC) before its progression to an overt stage is necessary for early treatment and positive outcomes. In 2001, the Scientific and Standardization Committee (SCC) of the International Society on Thrombosis and Hemostasis (ISTH) proposed new criteria for the preclinical diagnosis of overt and non-overt DICs. We investigated the clinical usefulness of the modified ISTH criteria for non-overt DIC diagnosis.
Methods
We enrolled 296 DIC patients (170 males and 126 females) admitted and evaluated at the Gangnam Severance Hospital, Seoul, Korea, between March 2006 and April 2007. Hemostatic tests, including platelet counts, prothrombin time (PT), D-dimer levels with antithrombin, and protein-C levels, were evaluated by excluding negative scores with clinical signs, in which more than 5 points of interest denoted non-overt DIC. Mortality rates were also evaluated.
Results
There were 289 patients with increased D-dimer levels and significant parametric changes suggesting DIC progression. Protein C and antithrombin levels were lower (99.2% each) and appeared earlier in patients with non-overt DIC than in patients with overt DIC. In all, 125 (43.3%) patients had non-overt DIC and, of which 27 died (mortality rate, 21.6%). The sensitivity and specificity for mortality were 73.0% and 55.9%, respectively, which were same as those for the original ISTH criteria.
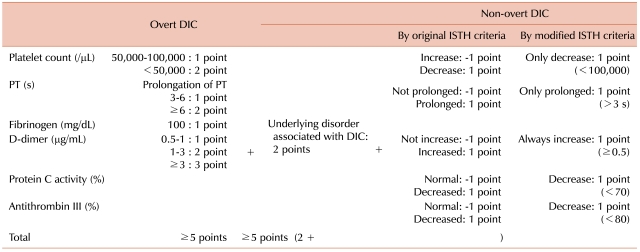
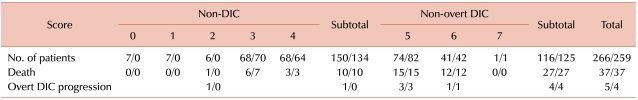
In 2001, the Scientific and Standardization Subcommittee (SSC) on disseminated intravascular coagulation (DIC) of the International Society of Thrombosis and Hemostasis (ISTH) proposed the current working definitions of overt and non-overt DIC [1]. Non-overt (early) DIC is a subtle hemostatic dysfunction that has not yet reached the decompensation stage, as in overt DIC. The ISTH SSC proposed a scoring system for the diagnosis of non-overt DIC on the basis of the clinical conditions and abnormal results of global hemostatic tests such as the platelet count, prothrombin time (PT), D-dimer, antithrombin (AT), and protein C (PC) levels; this system is similar to the defined scoring system for overt DIC. However, its clinical application is limited for scoring negative values. We investigated the usefulness of the ISTH criteria with minor modifications in diagnosing non-overt DIC (Table 1).
We enrolled 296 patients who were consecutively admitted for the treatment of various conditions associated with DIC at the Gangnam Severance Hospital, Seoul, Korea, between March 2006 and April 2007. There were 170 males and 126 females, with a median age of 64 years. Known clinical signs associated with DIC were used to confirm diagnoses.
Hemostatic tests, including platelet counts (Beckman Coulter Counter, Brea, CA, USA) and prothrombin time (STA NEOPLASTINE CI PLUS; Diagnostica, France), were evaluated at admission, daily during hospital stay, and at all follow-up visits. Serum fibrinogen (STA FIBRINOGEN; Diagnosica, France) and D-dimer (STA LIATEST D-dimer; Immunoturbidimetric assay, Diagnostia, France) levels with antithrombin (STA-STACHROM AT; Colorimetric assay, Diagnostica, France) and protein C (STA-STACHROM PROTEIN C; Colorimetric assay, Diagnostica, France) activities were evaluated at admission, during hospital stay biweekly or weekly, and at all follow-up visits.
D-dimer levels higher than 0.5 µg/mL were considered as elevated. Antithrombin and protein C activities less than 80% (normal, 88-134%) and 70% (normal, 70-130%) of normal, respectively, were considered as reduced.
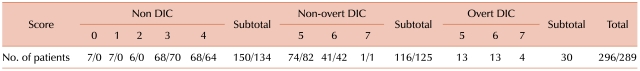
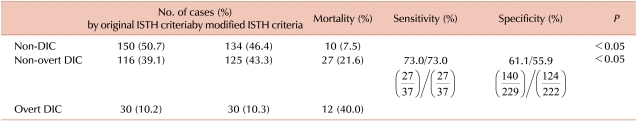
We modified the ISTH criteria for non-overt DIC diagnosis; for all paramedic applications and rejected any negative scores that did not accurately reflect laboratory data. Like in the ISTH criteria, a score of 5 or greater was denoted as non-overt DIC. When the modified criteria for non-overt DIC was used, the number of non-overt DIC diagnoses increased from 116 to 125 and the number of non-DIC diagnoses decreased from 150 to 134 (Table 2). Mortality rate was also calculated during the study period, and the sensitivity and specificity were determined.
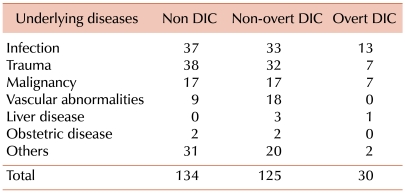
Underlying causative diseases included infections, trauma, and malignancy (in order of prevalence) (Table 3).
Of the 296 enrolled patients, 7 had stable D-dimer levels and no parametric changes, including protein C and antithrombin.
In all, 289 patients with increased D-dimer levels and significant parametric changes showed progression to either overt or non-overt DIC. However, no differences in the parameters were found between the patients who survived and those who died during the course of the study.
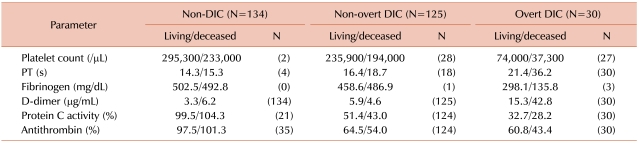
Of the 125 patients with non-overt DICs, 28 (22.4%) and 18 (14.4%) showed slightly increased platelet levels and PT levels, respectively. These relatively small changes in non-overt DIC patients were abruptly increased in patients with overt DIC. Moreover, 124 (99.2%) patients with non-overt DIC showed decreased protein C and antithrombin levels that were almost similar to those noted in overt DIC patients. However, the levels decreased earlier in non-overt DIC patients than in overt DIC patients (Table 4).
Of the 289 patients with increased D-dimer levels, 134 (46.4%) were diagnosed with non-DIC, of which 10 died (mortality rate, 7.5%).
In all, 125 (43.3%) patients were diagnosed with non-overt DIC, of which 27 died (mortality rate, 21.6%), including 4 patients who progressed to overt DIC. The sensitivities for mortality were 73.0% for non-overt DIC, which was same as that of the original ISTH criteria and the specificities were 61.1% and 55.9%, respectively. In all, 30 (10.3%) patients were diagnosed with overt DIC, of which 12 died (mortality rate, 40.0%). This mortality rate was higher than that of non-overt DIC patients (P<0.05) (Tables 5, 6).
DIC is characterized by systemic blood coagulation hyperactivation resulting in the consumption of platelets and coagulation factors, potentially leading to severe bleeding. Fibrinolytic activity depression and fibrin deposition occurs in the microcirculation, contributing to multiple organ failure. DIC is typically associated with several predisposing causes. In this study, the major underlying disorders associated with non-overt DIC included infection, trauma, and malignancy, which are similar to those that have been previously reported [2].
In 2001, the SSC of the ISTH recommended a new scoring system for non-overt DIC diagnosis [1]. Toh and Downey [2] showed that this proposed scoring system could be effectively applied. However, diagnosing the presence and severity of non-overt DIC using the ISTH scoring system can be complicated. For example, utilization of negative scores does not accurately reflect parametric changes, and does not display significant differences in sensitivity and specificity calculations for mortality. Therefore, in our ISTH modified criteria, negative scores were rejected: platelet counts were increased in 9 cases and this, in combination with elimination of negative scores, increased the number of non-overt DIC patients from 116 to 125 and decreased the number of non-DIC patients from 150 to 134. There were no PT values below the normal limits, and D-dimer with protein C and/or antithrombin levels were stable in 7 cases. In the remaining 289 cases, changes in plasma protein C or antithrombin levels were always observed with an associated increase in D-dimer level. A Japanese study reported that plasma D-dimer levels increased and plasma protein C and antithrombin levels decreased in the non-overt DIC cases [3]; our data was consistent with these findings.
Although the ISTH scoring system for non-overt DIC allows for the measurement of protein C and antithrombin levels, Kinasewitz et al. [4] insisted that the combination of scoring abnormal results in the PT, platelet count, and D-dimer levels might provide sufficient criteria to diagnose DIC without the use of molecular markers. Additionally, Toh and Hoots [5] were hesitant to validate the value by including PC and AT estimations. However, our data showed a good relationship between the 2 parametric changes for DIC status.
In our study, the mortality rate of non-overt DIC patients was 21.6%, including the 4 cases that progressed to overt DIC. This rate was lower than those reported in other studies [2], where the mortality rate was as high as 78%, which was same as that in their overt DIC patients. They showed that non-overt DIC itself carries a prognosis independent of overt DIC, and suggested that a score of 5 or higher may represent a decompensated phase of hemostatic dysfunction, albeit at an earlier stage than overt DIC. Additionally, another study reported mean intervals between non-overt and consequent overt DIC and death to be 1 and 5 days, respectively [6]. Therefore, a diagnosis of non-overt DIC may present a therapeutic window of opportunity for targeting treatment. Dhainaut et al. [7] reported a retrospective analysis on the use of activated protein C in severe sepsis. Patients without overt DIC had a mortality rate of 22.1%, but placebo-treated DIC patients had a mortality rate of 27.1%, with less benefit. In a study involving the KyberSept cohort of patients treated with antithrombin, the authors did not use negative scores for the decrease in antithrombin and protein C activities. A reduction in non-overt DIC patient mortality was observed at 28 and 90 days with 25.7 and 34.6%, compared to mortality rates of 40.9 and 51.8%, respectively, in the placebo groups [8]. These results show that an effective method of reducing DIC mortality rates is to begin treatment early, while the patients are still in the non-overt DIC stage.
In conclusion, we attempted to modify the ISTH criteria for non-overt DIC diagnosis to allow simple and practical early detection of non-overt DIC, which may improve disease outcomes.
References
1. Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M. Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH). Towards definition, clinical and laboratory criteria and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001; 86:1327–1330. PMID: 11816725.

2. Toh CH, Downey C. Performance and prognostic importance of a new clinical and laboratory scoring system for identifying non-overt disseminated intravascular coagulation. Blood Coagul Fibrinolysis. 2005; 16:69–74. PMID: 15650549.

3. Wada H, Wakita Y, Nakase T, et al. Mie DIC study Group. Outcome of disseminated intravascular coagulation in relation to the score when treatment was begun. Thromb Haemost. 1995; 74:848–852. PMID: 8571309.

4. Kinasewitz GT, Zein JG, Lee GL, Nazir SA, Taylor FB Jr. Prognostic value of a simple evolving disseminated intravascular coagulation score in patients with severe sepsis. Crit Care Med. 2005; 33:2214–2221. PMID: 16215373.

5. Toh CH, Hoots WK. SSC on Disseminated Intravascular Coagulation of the ISTH. The scoring system of the Scientific and Standardisation Committee on Disseminated Intravascular Coagulation of the International Society on Thrombosis and Haemostasis: a 5-year overview. J Thromb Haemost. 2007; 5:604–606. PMID: 17096704.

6. Dhainaut JF, Shorr AF, Macias WL, et al. Dynamic evolution of coagulopathy in the first day of severe sepsis: relationship with mortality and organ failure. Crit Care Med. 2005; 33:341–348. PMID: 15699837.

7. Dhainaut JF, Yan SB, Joyce DE, et al. Treatment effects of drotrecogin alfa (activated) in patients with severe sepsis with or without overt disseminated intravascular coagulation. J Thromb Haemost. 2004; 2:1924–1933. PMID: 15550023.
8. Kienast J, Juers M, Wiedermann CJ, et al. Treatment effects of high-dose antithrombin without concomitant heparin in patients with severe sepsis with or without disseminated intravascular coagulation. J Thromb Haemost. 2006; 4:90–97. PMID: 16409457.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download