Plasma components, such as fresh frozen plasma (FFP), fresh plasma, frozen plasma, and cryoprecipitates, are commonly used for the correction of bleeding due to the deficiency of blood coagulation factors. Furthermore, blood coagulation factors and plasma proteins are components of plasma that enable the manufacture of plasma derivatives, including factor VIII concentrates, factor IX concentrates, immunoglobulin, and albumin. In this paper, we discuss the current domestic status of plasma use and the related insurance policy of the Health Insurance Review & Assessment Service (HIRA), which ensures health insurance for the entire South Korean nation. This in turn will aid in developing a proposal for the proper use of plasma components.
CURRENT DOMESTIC STATUS OF PLASMA USE
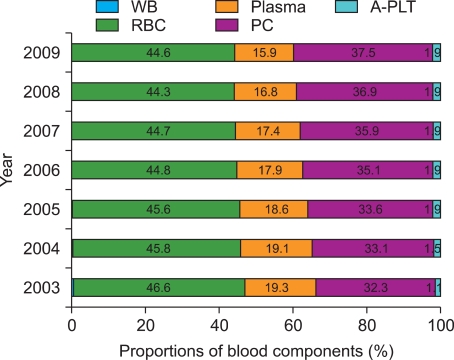
The transfusion of plasma components in Korea began in earnest in the 1990s, with the establishment of blood component therapy as an alternative to whole blood therapy. In 2009, a total of 658,069 units of plasma were supplied from the Korean Red Cross Blood Center (KRCBC), which mainly comprised FFP (92.7%), cryoprecipitates (7.3%), and frozen plasma (0.1%). The KRCBC provides approximately 97% of all the blood components used in Korea. According to the Annals of Statistics from KRCBC, the total plasma supply gradually decreased from 2003 (663,539 units) to 2006 (636,897 units), but then increased slightly from 2007 (643,674 units) to 2009 (658,069 units). Among blood components, lesser amounts of plasma are supplied compared with red blood cells (RBC) and platelets. In Korea, plasma accounts for less than 20% of all blood components supplied, and the proportion of plasma supplied has steadily decreased from 2003 (19.3%) to 2009 (15.9%) (Fig. 1).
Despite using 98% of total plasma components, the total amount of claims to HIRA from tertiary and general hospitals for plasma accounts for approximately 75% of the total plasma supply of KRCBC. Although the proportion of the amount of claims for plasma components to the supply of plasma has gradually increased over time, the remaining 25% might be claimed mostly by automobile insurance and industrial accident insurance, or, in a small proportion of cases, is directly paid for by the patients without filing for claims to HIRA. As a regional emergency medical center of southern Gyeonggi-do, Ajou University Hospital filed for claims to automobile insurance or industrial accident insurance companies for 22.4% of the total plasma units used in 2009.
According to the Annals of Statistics from HIRA, although the amount of plasma used has shown an annual variation, tertiary hospitals have used approximately twice as many plasma components as have general hospitals (1.86-1.96 folds), indicating that the main source of plasma consumption is tertiary hospitals. The average RBC-to-plasma transfusion ratio is 2.31:1, with higher plasma usage in tertiary hospitals (1.9:1) than in general hospitals (3:1). The units of plasma per plasma claim (plasma units/claim) was maintained at 7.6-7.7 units between 2005 and 2008, with a slight annual variation. The "plasma units/claim" was higher in tertiary hospitals (7.8 units) than in general hospitals (7.4 units), and was two times higher than that for RBCs (3.8 units), despite the fact that the amount of plasma used was only half that of RBCs. Regardless of the fact that a smaller number of patients were transfused with FFP compared to RBCs, FFP-transfused patients received more units of FFP when compared to the amount of RBCs used in RBC-transfused patients.
According to the claims filed to HIRA for transfusion from 2003 to 2007, the male-to-female ratio for plasma use was 1.8:1, indicating that men were more likely to receive plasma transfusion. Approximately half of the plasma components supplied were used for patients in their 50s (22.5%) and 60 s (23.3%). Plasma was most frequently used by the departments of internal medicine (53.2%), followed by general surgery (19.0%), thoracic surgery (7.9%), neurosurgery (6.1%), pediatrics (3.5%), obstetrics & gynecology (2.9%), orthopedic surgery (2.8%), emergency medicine (2.1%), and others (2.5%). The departments with the highest "plasma units/claim" were general surgery (8.4 units), internal medicine (7.3 units), and thoracic surgery (6.1 units).
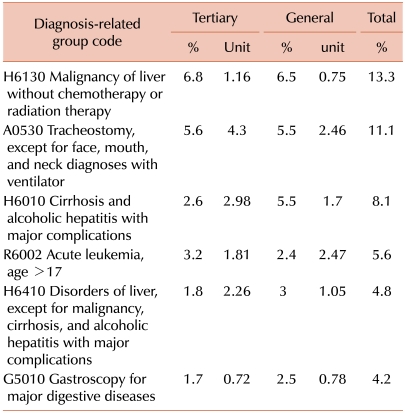
The claims filed to HIRA for transfusion in 2004 revealed that approximately 38% of plasma was given to patients with liver disease or cancer. The annual reports of HIRA from 2006 to 2008 describe patients with liver disease as the group with the highest use of plasma. Excluding the acute leukemia (age>17) group, plasma use showed a declining trend in general hospitals. Table 1 shows the proportion (%) and mean units of plasma used per plasma transfusion among the disease groups categorized by diagnosis-related group (DRG) code in tertiary and general hospitals from 2006 to 2008.
The studies on blood use in Korea have reported that FFP is the blood component with the highest percentage of inappropriate transfusions. Inappropriate transfusion of FFP varied among hospitals, ranging from 30.7% to 59.2%, compared to 2.8-19.9% for RBC transfusion and 4.9-14.3% for platelet transfusion. These reports indicated the following as inappropriate administrations of FFP: use without a specific reason in patients with burns; use as a blood volume expander in patients with decreased albumin levels or blood volume; use for nutritional support of patients or psychological reliefs for patients and attending physicians, routine use with RBC transfusions; and to facilitate healing of post-operative wounds.
Thawed FFP must be discarded, if it is stored longer than 3 hours at room temperature or 24 hours in a refrigerator. In its evaluation of blood wastage in hospitals in 2008, the Division of Human Blood Safety Surveillance reported a high RBC wastage rate (5.1%) in institutes with admission capacities of 100 beds or less, and the highest rates of FFP wastage (2.3%) in institutes with admission capacities of 500 beds or more; these being a significant source of plasma consumption [1].
DOMESTIC INSURANCE POLICY FOR THE USE OF PLASMA
The exact rate of cuts on blood components is currently unknown because official data is not provided by HIRA. Nevertheless, FFP is expected to have the highest cut rates among blood components. However, the reported cut rates on claims to HIRA for blood components from a single tertiary hospital in 2009 were 2.06% for platelets, 1.2% for FFP, and 0.04% for RBCs. The low cut rates for FFP in comparison to platelets could be explained by the high number of FFP units used without claims to HIRA and paid for by the patients.
HIRA does not provide official screening criteria. This is because it is difficult to apply the same screening criteria to insurance claims for FFP transfusion, since each clinical case requiring FFP transfusion is different. Therefore, the medical records and laboratory findings are reviewed in order to decide whether plasma transfusion is needed to stop bleeding or whether coagulation factors should be used instead. The inspection personnel of HIRA are in charge of performing initial evaluations of all claims for blood components and, if necessary, full-time or part-time advisory committee members are consulted for further review prior to making the final decision.
Typical examples of cutbacks on claims for FFP were FFP transfusions without blood coagulation testing, patients with blood coagulation tests results but not supporting FFP transfusion, and albumin supplementation as the sole objective in patients with burns or at post-operation. Claims for FFP by surgical departments are frequently subjected to cuts, which was also apparent in the data from Ajou University, which revealed 86% of cuts occurred in surgical departments. HIRA began evaluations of the adequate use of blood components in general and tertiary-level hospitals that make claims via EDI (Electronic Data Interchange) billing in 2003, with yearly evaluations since 2008. According to the evaluation, the plasma transfusion volume index per diagnosis in 2008 showed tendencies of a decrease in tertiary hospitals and an increase in general hospitals in comparison with those of 2006.
CONCLUSION
Among the blood components, the proportion of plasma use has steadily decreased compared to those of RBC or platelets. FFP is the most commonly used plasma product, but it is also the product with the highest inappropriate transfusion rate and blood disposal rate. Therefore, vigorous efforts by clinicians and the blood bank staffs to prevent wastage and misuse of FFP are needed to encourage proper use of FFP and to prevent wastage of valuable resources.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download