Abstract
Background
Despite advances in chemotherapy, the prognosis of relapsed acute lymphoblastic leukemia (ALL) remains poor. Few studies on relapsed ALL have reported the importance of intensive consolidation followed with or without allogeneic hematopoietic stem cell transplantation (HSCT).
Methods
We evaluated the post-relapse outcomes in 47 Korean children with a first marrow relapse, and analyzed the prognostic factors.
Results
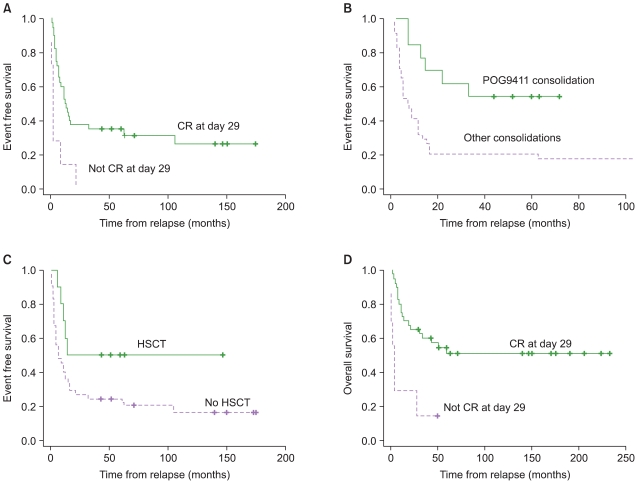
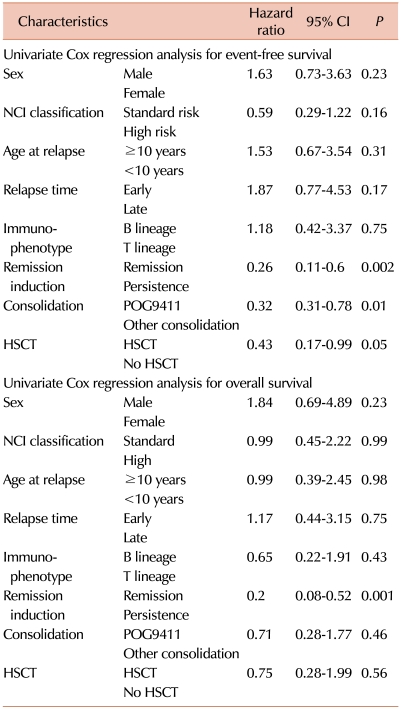
A second complete remission (CR) was achieved in 40 patients (85.1%), and at the time of this study, second CR was maintained in 12 of these patients. The estimated 3-yr event-free survival (EFS) rate after the first marrow relapse was 29.8±6.7%, and the overall survival (OS) rate was 45.3±7.5%. We found that second remission, consolidation of pediatric oncology group chemotherapy regimen (POG 9411), and HSCT significantly affected the outcome of the disease after relapse (P<0.001; P=0.004; P=0.05).
Although the cure rate of childhood acute lymphoblastic leukemia (ALL) has remarkably improved with advances in chemotherapy, relapse still occurs in about 30% of the cases, with many patients showing relapse in the bone marrow (BM) [1, 2]. Although second remission can be achieved after intensive reinduction chemotherapy in a majority of patients, many patients relapse again and experience a dismal outcome [3]. Hematopoietic stem cell transplantation (HSCT) is frequently performed to improve the outcome in patients with relapsed ALL. In this study, we evaluated the post-relapse outcomes of ALL in 47 Korean children with a first marrow relapse, and then analyzed the prognostic factors affecting the outcome, with the special focus on consolidation therapy and HSCT.
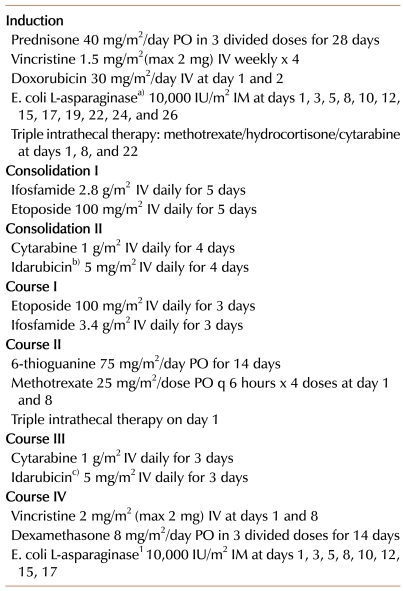
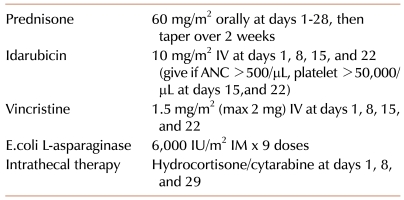
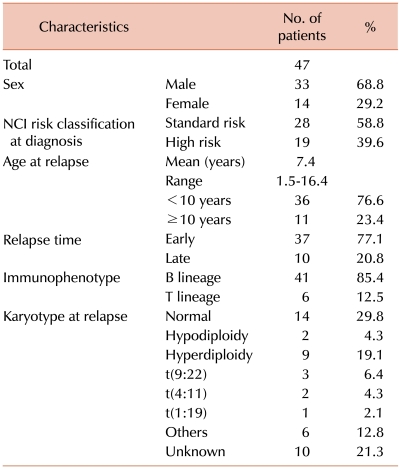
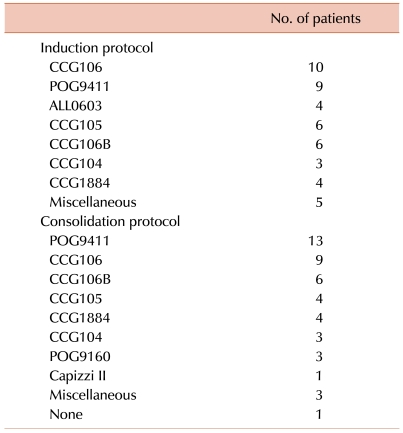
Forty-seven patients (age, >1 yr) with an initial diagnosis of first BM relapse and without L3 morphology were included in this study between 1991 and 2006. Depending on the treatment period and the physicians, patients were treated with various ALL protocols adapted from the Children's Cancer Group (CCG) [4-9] or the Pediatric Oncology Group (POG9411) (Table 1). In addition, 4 patients were treated according to the protocol of the Korean multicenter trial ALL0603 (Table 2). Allogeneic HSCT has been incorporated into intensive, multiagent chemotherapy regimens for the treatment of patients with relapsed ALL since 1999, and in this study, 10 patients underwent HSCT. Four patients received an allogeneic stem cell transplant from a human leukocyte antigen (HLA)-identical sibling donor, and 5 patients received a stem cell transplant from an unrelated donor; 1 patient received a stem cell transplant from an HLA-haploidentical related donor. All patients except the patient who received the haploidentical transplant were conditioned with total body irradiation and cyclophosphamide. The patient who received the haploidentical transplant was conditioned with a busulfan plus cyclophosphamide regimen.
The clinical characteristics we examined were: age, sex, immunophenotype of leukemic blasts, the National Cancer Institute (NCI)'s risk classification (standard risk, 1-9 yr of age and WBC count of <50,000/µL vs. high risk: others) at initial presentation [10], early (<36 mo from initial diagnosis) vs. late (≥36 mo from initial diagnosis) relapse, and treatment after relapse. We compared the second remission rates of different induction protocols. We compared the POG9411 consolidation regimen with other post-remission chemotherapies, and analyzed the effect of intensified consolidation on survival after the second remission. In addition, we analyzed that HSCT could affect the outcome of relapsed ALL patients.
Complete remission (CR) was defined as less than 5% blasts in BM aspirates, and hematologic recovery was defined as an absolute neutrophil count of over 1,000/µL and a platelet count greater than 100,000/µL. Univariate analyses of the association between CR rates and induction chemotherapies were performed using the chi-squared test. EFS was defined as the time from the first relapse to the next subsequent event (relapse, second malignancy, follow-up loss, or death from any cause). OS was defined as the time interval between the first relapse and death. EFS and OS curves were estimated using Kaplan-Meier analysis. Univariate Cox regression analysis was performed for each potential predictor of outcome. Relative hazard ratios (HR) with 95% confidence interval (CI) were determined for each factor while controlling the others. P-value was considered to be significant at <0.05. All statistical analyses were performed using SPSS, version 13.0 (SPSS Inc, Chicago, IL).
Forty-seven patients, 33 men and 14 women, were analyzed as of May 2010. Clinical characteristics of patients are shown in Table 3. The follow-up period after relapse ranged from 43 mo to 20 yr (median, 145.7 mo). The mean age at relapse was 7.4±0.6 yr, with a range of 1.5-16.4 yr. The mean time from initial diagnosis to relapse was 17.5±3.2 mo. Forty-one patients had B cell immunophenotype, and 6 patients had T cell immunophenotype. According to the NCI risk classification, 28 patients were standard risk, and 19 patients were high risk. Thirty-seven relapses occurred within 36 mo from initial diagnosis (early relapse), while 10 patients relapsed after more than 36 mo from initial diagnosis (late relapse).
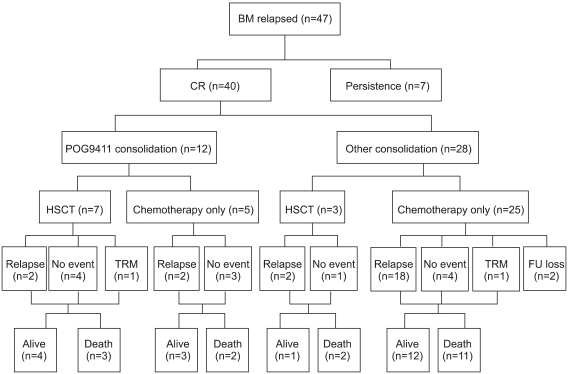
The overall treatment and outcome data are summarized in Fig. 1 and Table 4. Forty patients (85.1%) succeeded in attaining second remission, and 7 patients showed persistence (M2 or M3 marrow at day 29 of induction). There was no significant difference in remission induction rates among ALL0603, POG9411, and other induction chemotherapies of the past (100% vs. 88.9% vs. 82.4%, P=0.6). After achieving second remission, the type of consolidation chemotherapy seemed to influence the outcome. Of the 40 patients who attained second remission, 12 patients (7 early relapses and 5 late relapses) were treated with a POG9411 consolidation regimen. After the second cycle of POG9411 consolidation, 7 patients (6 early relapses and 1 late relapse) underwent HSCT, and 5 patients continued on chemotherapy only. Seven of the 12 patients treated with POG9411 remained in a continuous second remission at the time of this study. On the other hand, of the 28 patients (25 early relapses and 3 late relapses) who received other consolidation regimens, only 3 underwent HSCT, and just 5 remained relapse-free to date. The EFS rate of the POG9411 consolidation group was significantly superior to that of the others (53.8±13.8% vs. 14.7±6.1%, P=0.004) (Fig. 2).
The 3-yr EFS rate of marrow relapsed patients was 29.8±6.7%, and the 3-yr OS rate was 45.3±7.5%. Univariate analyses of EFS (Table 5) revealed that a second remission, POG9411 consolidation, and use of HSCT were significant prognostic factors (Fig. 2). Univariate analyses of OS (Table 5) revealed that achievement of a second remission significantly affected outcome (Fig. 1D). In the early-relapsed group, EFS rates were significantly altered by HSCT (46.7% vs. 13.7%, HR 0.034, 95% CI 0.16-0.93, P=0.034). However, HSCT was performed in only 1 late-relapsed patient, so the benefit of HSCT for late-relapsed patients was not clear (HR 0.45, 95% CI 0.05-4.05, P=0.48). Multivariate analysis concurred with the results of the univariate analysis. However, only a second remission and POG9411 consolidation could significantly improve EFS rates (HR 0.17, 95% CI 0.06-0.47, P=0.001; HR 0.42, 95% CI 0.17-0.97, P=0.03), and just the attainment of remission could affect the OS (HR 0.12, 95% CI 0.03-0.39, P<0.001).
Even with the improvement of chemotherapy, the prognosis of relapsed ALL remained poor. The poor prognosis was attributed to lower remission re-induction rates and a short duration of the second remission [8, 9]. Previous studies have reported that survival after relapse varies significantly depending on the time of relapse, sex, NCI risk classification at initial diagnosis, and the treatment after relapse [11-14]. Our study was limited by the relatively small number of patients. Nonetheless, our study suggested that intensive consolidation, such as POG9411, and allogeneic HSCT were crucial and could improve outcome.
Prior experiences have shown that the most important factor affecting outcome was the time to relapse [14-16]. Although there was not enough statistical significance in our study, early-relapsed patients had a shorter second CR duration and lower OS rates than those of late-relapsed patients. In addition, some studies reported that an initial WBC less than 50,000/µL, and age younger than 10 yr at initial diagnosis predicted a more favorable outcome after relapse [14, 17], while our study failed to show any statistical significance of NCI risk classification on post-relapse outcome.
Attainment of second remission (M1 marrow at day 29 of re-induction) was a significant prognostic factor for EFS and OS. It was an initial step toward a successful outcome, and patients who failed to go into remission within 4 weeks had a poorer prognosis. In our study, POG9411 consolidation therapy significantly increased the EFS rate after second remission. The POG9411 protocol was designed to deliver very intensive chemotherapy consisting of a modified standard reinduction combination followed by 2 intensive consolidation courses, followed by 4 courses of non-cross resistant drug combinations for continuation therapy. It appeared that POG9411 consolidation helped achieve a greater reduction of leukemia. A recent study of CCG1961 indicated that longer post-induction intensification failed to prolong EFS, while an early aggressive post-induction intensification resulted in better EFS and OS for patients with newly diagnosed high-risk ALL [18]. Many studies have reported that the presence of minimal residual disease (MRD) prior to allogeneic transplantation is predictive of subsequent treatment failure [19, 20]. Superior outcome was observed if patients received the transplant with less malignant cell burden and lower MRD [21]. The end-induction MRD levels are strongly dependent on the intensity of the therapeutic regimens [22]. The POG9411 regimen may more effectively reduce the MRD as compared to other consolidations in this report.
In addition, HSCT significantly improved EFS rate for marrow-relapsed patients. In recent years, HSCT has been increasingly utilized in the management of relapsed leukemia. Previously published retrospective studies showed that the marrow-relapsed patients that received allogeneic HSCT, especially from HLA-matched sibling donors, showed a significantly better outcome than the patients that received chemotherapy alone [23-26]. However, benefits of HSCT in late BM relapse seemed less evident and the late-relapsed patients had a considerably better chance of cure by chemotherapy alone [12, 26]. Our study also demonstrated that HSCT was more beneficial for EFS in early-relapsed patients, while there was no clear advantage of HSCT for EFS in late-relapsed patients.
This study showed that POG9411 intensive consolidation therapy followed by allogeneic HSCT conferred a better survival rate in children with ALL with BM relapse. However, this retrospective study was limited by a relatively small number of patients and multiple heterogeneous treatment regimens. Since these patients were treated over a 20-yr period, the advancement in therapies and supportive care over time may have improved the treatment outcome. Therefore, a prospective multicenter trial involving a larger number of patients treated with a uniform regimen is clearly required for ALL with BM relapse. We believe that the use of an intensive consolidation regimen comprising non-cross resistant drug combinations followed by HSCT should be an integral part of therapeutic strategy in designing a new protocol for the treatment of marrow-relapse ALL in children.
References
1. Chessells JM. Treatment of childhood acute lymphoblastic leukaemia: present issues and future prospects. Blood Rev. 1992; 6:193–203. PMID: 1486288.

2. Rivera GK, Raimondi SC, Hancock ML, et al. Improved outcome in childhood acute lymphoblastic leukaemia with reinforced early treatment and rotational combination chemotherapy. Lancet. 1991; 337:61–66. PMID: 1670723.

3. Chessells JM. Relapsed lymphoblastic leukaemia in children: a continuing challenge. Br J Haematol. 1998; 102:423–438. PMID: 9695956.
4. Uckun FM, Nachman JB, Sather HN, et al. Poor treatment outcome of Philadelphia chromosome-positive pediatric acute lymphoblastic leukemia despite intensive chemotherapy. Leuk Lymphoma. 1999; 33:101–106. PMID: 10194126.

5. Hutchinson RJ, Gaynon PS, Sather H, et al. Intensification of therapy for children with lower-risk acute lymphoblastic leukemia: long-term follow-up of patients treated on Children's Cancer Group Trial 1881. J Clin Oncol. 2003; 21:1790–1797. PMID: 12721256.

6. Heath JA, Steinherz PG, Altman A, et al. Human granulocyte colony-stimulating factor in children with high-risk acute lymphoblastic leukemia: a Children's Cancer Group Study. J Clin Oncol. 2003; 21:1612–1617. PMID: 12697887.

7. Gaynon PS, Steinherz PG, Bleyer WA, et al. Intensive therapy for children with acute lymphoblastic leukaemia and unfavourable presenting features. Early conclusions of study CCG-106 by the Childrens Cancer Study Group. Lancet. 1988; 2:921–924. PMID: 2902379.
8. Gaynon PS, Harris RE, Altman AJ, et al. Bone marrow transplantation versus prolonged intensive chemotherapy for children with acute lymphoblastic leukemia and an initial bone marrow relapse within 12 months of the completion of primary therapy: Children's Oncology Group study CCG-1941. J Clin Oncol. 2006; 24:3150–3156. PMID: 16717292.

9. Feig SA, Harris RE, Sather HN. Bone marrow transplantation versus chemotherapy for maintenance of second remission of childhood acute lymphoblastic leukemia: a study of the Childrens Cancer Group (CCG-1884). Med Pediatr Oncol. 1997; 29:534–540. PMID: 9324340.

10. Smith M, Arthur D, Camitta B, et al. Uniform approach to risk classification and treatment assignment for children with acute lymphoblastic leukemia. J Clin Oncol. 1996; 14:18–24. PMID: 8558195.

11. Wheeler K, Richards S, Bailey C, Chessells J. Comparison of bone marrow transplant and chemotherapy for relapsed childhood acute lymphoblastic leukaemia: the MRC UKALL X experience. Medical Research Council Working Party on Childhood Leukaemia. Br J Haematol. 1998; 101:94–103. PMID: 9576189.
12. Borgmann A, von Stackelberg A, Hartmann R, et al. Unrelated donor stem cell transplantation compared with chemotherapy for children with acute lymphoblastic leukemia in a second remission: a matched-pair analysis. Blood. 2003; 101:3835–3839. PMID: 12732501.

13. Chessells JM, Veys P, Kempski H, et al. Long-term follow-up of relapsed childhood acute lymphoblastic leukaemia. Br J Haematol. 2003; 123:396–405. PMID: 14616997.

14. Nguyen K, Devidas M, Cheng SC, et al. Factors influencing survival after relapse from acute lymphoblastic leukemia: a Children's Oncology Group study. Leukemia. 2008; 22:2142–2150. PMID: 18818707.

15. Henze G, Fengler R, Hartmann R, Niethammer D, Schellong G, Riehm H. BFM group treatment results in relapsed childhood acute lymphoblastic leukemia. Haematol Blood Transfus. 1990; 33:619–626. PMID: 2182452.

16. Buchanan GR, Rivera GK, Pollock BH, et al. Alternating drug pairs with or without periodic reinduction in children with acute lymphoblastic leukemia in second bone marrow remission: a Pediatric Oncology Group Study. Cancer. 2000; 88:1166–1174. PMID: 10699908.
17. Malempati S, Gaynon PS, Sather H, La MK, Stork LC. Outcome after relapse among children with standard-risk acute lymphoblastic leukemia: Children's Oncology Group study CCG-1952. J Clin Oncol. 2007; 25:5800–5807. PMID: 18089878.

18. Seibel NL, Steinherz PG, Sather HN, et al. Early postinduction intensification therapy improves survival for children and adolescents with high-risk acute lymphoblastic leukemia: a report from the Children's Oncology Group. Blood. 2008; 111:2548–2555. PMID: 18039957.
19. Paganin M, Zecca M, Fabbri G, et al. Minimal residual disease is an important predictive factor of outcome in children with relapsed 'high-risk' acute lymphoblastic leukemia. Leukemia. 2008; 22:2193–2200. PMID: 18754029.

20. Mehta PA, Davies SM. Pre-transplant minimal residual disease in children with acute lymphoblastic leukemia. Pediatr Blood Cancer. 2007; 48:1–2. PMID: 16642487.

21. Krejci O, van der Velden VH, Bader P, et al. Level of minimal residual disease prior to haematopoietic stem cell transplantation predicts prognosis in paediatric patients with acute lymphoblastic leukaemia: a report of the Pre-BMT MRD Study Group. Bone Marrow Transplant. 2003; 32:849–851. PMID: 14520434.

22. zur Stadt U, Harms DO, Schlüter S, et al. MRD at the end of induction therapy in childhood acute lymphoblastic leukemia: outcome prediction strongly depends on the therapeutic regimen. Leukemia. 2001; 15:283–285. PMID: 11236947.

23. Matsuzaki A, Nagatoshi Y, Inada H, et al. Prognostic factors for relapsed childhood acute lymphoblastic leukemia: impact of allogeneic stem cell transplantation--a report from the Kyushu-Yamaguchi Children's Cancer Study Group. Pediatr Blood Cancer. 2005; 45:111–120. PMID: 15782402.

24. Boulad F, Steinherz P, Reyes B, et al. Allogeneic bone marrow transplantation versus chemotherapy for the treatment of childhood acute lymphoblastic leukemia in second remission: a single-institution study. J Clin Oncol. 1999; 17:197–207. PMID: 10458234.

25. Barrett AJ, Horowitz MM, Pollock BH, et al. Bone marrow transplants from HLA-identical siblings as compared with chemotherapy for children with acute lymphoblastic leukemia in a second remission. N Engl J Med. 1994; 331:1253–1258. PMID: 7935682.

26. Eapen M, Raetz E, Zhang MJ, et al. Outcomes after HLA-matched sibling transplantation or chemotherapy in children with B-precursor acute lymphoblastic leukemia in a second remission: a collaborative study of the Children's Oncology Group and the Center for International Blood and Marrow Transplant Research. Blood. 2006; 107:4961–4967. PMID: 16493003.

Fig. 2
Event-free survival rates and overall survival rates of patients with marrow-relapse ALL. Event-free survival rates differed due to the achievement of second remission (A), consolidation chemotherapy after remission (B), and allogeneic hematopoeitic stem call transplantation (HSCT) (C). Overall survival rates were significantly affected by the achievement of second remission (D).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download