Abstract
Septic arthritis of the temporomandibular joint (TMJ) is a rare disease. The most common symptoms of this disease are acute malocclusion, limited mouth opening, swelling, and tenderness of affected TMJ. These symptoms are often confused with internal derangement of the articular disc, rheumatoid arthritis, retrodiscitis, or osteoarthritis. Therefore, differential diagnosis by image examination is required. Usually, antimicrobial treatment and surgical drainage by needle aspiration, arthroscopy, or arthrotomy are effective treatment approaches. In this study, a patient who was diagnosed with septic arthritis was treated with arthrocentesis and antibiotics without significant complications. We present a case report with a review of the literature.
Go to : 
Septic arthritis of the temporomandibular joint (TMJ) presents as a severe infection with fever, pain, swelling, redness, and hypofunction in the affected joint. It is also characterized by preauricular edema and trismus12. Septic arthritis of the TMJ occurs from either local dissemination or hematogenous spread from a distant primary infectious site3.
A mortality rate of 12% has been reported for cases of septic arthritis in whole body joints, and significant hypofunction of the affected joint is observed in up to 75% of survivors1. Septic arthritis of the TMJ is known to result in significant morbidity if diagnosis is delayed45. Therefore, we describe the importance of early diagnosis and appropriate treatment of TMJ septic arthritis.
Go to : 
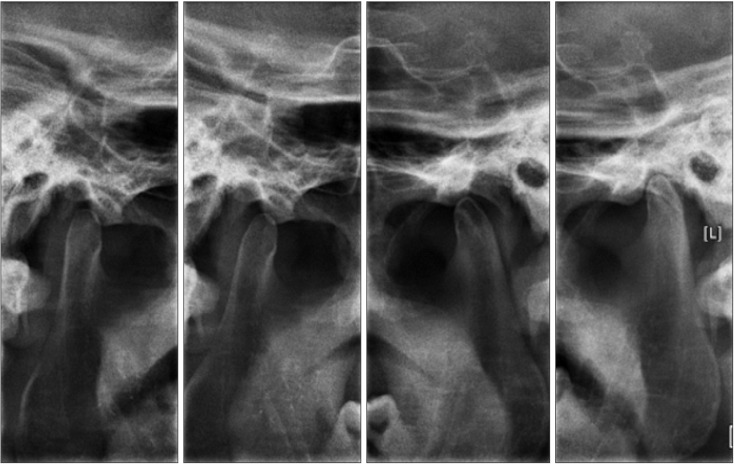
A 52-year-old man presented to the Department of Oral and Maxillofacial Surgery, Gachon University Gil Medical Center (Incheon, Korea) with reports of pain in the right TMJ, acute malocclusion with posterior open bite of the ipsilateral side (Fig. 1), deviation of the lower dental midline to left side, and limited mouth opening. The symptoms began 10 days prior to presentation and progressively worsened. At the onset of symptoms, he was diagnosed with temporomandibular disorder from another dental clinic and prescribed a muscle relaxant and analgesics for 7 days; however, his pain did not improve. He did not have any systemic predisposing factors. Clinical examination showed maximum mouth opening limited to 25 mm, posterior open bite on the right side, and preauricular swelling. Joint space widening on the right TMJ was identified on plain film.(Fig. 2) Serum leukocyte and C-reactive protein were tested prior to arthrocentesis, which showed a normal serum leukocyte and increased C-reactive protein level. We suspected a systemic infection from primary TMJ infectious disease.
After clinical evaluation with laboratory tests and plain films, a provisional diagnosis was made of septic arthritis of the right TMJ. The patient underwent arthrocentesis on the right TMJ under local anesthesia. A traditional two-needle technique was used for arthrocentesis: an imaginary line was marked from the tragus of the ear to the lateral canthus of the eye. At first, one needle was placed approximately 10 mm forward along this line and 2 mm below it. Joint fluid was obtained from the upper joint cavity and was sent for microbiological examination. We observed turbid fluid (Fig. 3) and whitish debris macroscopically. One more needle was inserted in the upper joint cavity and the joint was thoroughly irrigated with 500 mL of 0.9% normal saline. A broad-spectrum antibiotic (amoxicillin 250 mg/clavulanate 125 mg, Cramotin; Dong-A ST, Seoul, Korea) and analgesic (naproxen sodium 275 mg, Anaprox; Chong Kun Dang, Seoul, Korea) were prescribed for 7 days. Staphylococcus aureus was founded in the microbiological examination.
At follow-up 7 days later, the patient's symptoms were slightly improved. However, preauricular swelling, TMJ pain during opening and mastication, and posterior open bite malocclusion were still present.(Fig. 4) Computed tomography (CT) was performed to evaluate the residual exudate in the right TMJ space and the need for additional arthrocentesis. A widening of the joint space and bony change were not observed on contrast enhanced CT, so the patient was prescribed an additional 7 day course of both medications; we also recommended mouth opening exercises.
At the 1-month follow-up, pain with opening and clenching were absent. Occlusion returned to almost normal (Fig. 5), and maximum mouth opening was increased to 35 mm without pain. We recommended aggressive range of motion exercises to minimize the risk of long-term restricted mouth opening6.
Go to : 
TMJ arthritis is caused by either hematogenous dissemination of microorganisms into the well-vascularized synovial membrane or the direct spread of an adjacent contiguous infection1. The most common cause is hematogenous spread from a distant primary infection4. In adults, the spread of local infection to the TMJ has occurred in cases of infection after molar extraction, intra-articular injection, facial burns, and otitis externa. Blunt trauma with resulting capsular injury may also facilitate the hematogenous spread of infection into the joint space5.
Complications of septic arthritis of the TMJ include a high incidence of local spread, recurrence, destruction of joint articular surfaces, and bony ankyloses or fibrotic changes of the TMJ14. Symptoms of acute malocclusion, limited mouth opening, swelling and tenderness may also occur.
Septic arthritis of the TMJ is a medical emergency due to its severe complications. Therefore, early diagnosis and treatment of TMJ septic arthritis are required to obtain better clinical outcomes. Unfortunately, the primary symptoms of septic TMJ arthritis may be confused with other TMJ disorders such as internal derangement, synovial chondromatosis, or rheumatoid arthritis6. Therefore, the diagnostic criteria should include imaging findings, joint fluid analysis, and laboratory examination as well as clinical appearance1.
Imaging studies are useful for accurate diagnosis. Increased intracapsular fluid caused by accumulation of pus and inflammatory exudate results in restriction of condyle movement and joint space widening1. These pathologic changes in the TMJ can be observed on plain film. Contrast-enhanced CT is used to identify pathologic changes such as joint effusions, condylar surface change, ankylosis, and osteomyelitis of the TMJ. Magnetic resonance imaging (MRI) is useful for earlier detection of joint effusions and evaluation of joint surfaces and periarticular soft tissue7. Therefore, MRI is considered a very useful method in the diagnosis of septic arthritis. T2 scan on MRI is highly recommended to evaluate joint effusions. However, in our case, septic arthritis of the TMJ was already confirmed after arthrocentesis and microbiological examination of the aspirated joint fluid prior to additional imaging. Therefore, MRI was not deemed useful after proceeding with arthrocentesis because the infused saline and remaining exudate could not be distinguished on MRI. At the patient's second visit, his symptoms were considerably improved. Therefore, MRI was not felt to be necessary. Joint fluid aspiration is recommended for additional investigation when septic arthritis has been diagnosed. The joint aspirate should be examined grossly for color and turbidity as indicators of infection, microscopically for joint fluid analysis, and then submitted for culture, Gram stain, and sensitivity analysis7. Joint fluid will be light yellow, transparent, and glistening in the patient with a temporomandibular disorder or rheumatoid arthritis. In contrast, it will be turbid or semitransparent in an infected joint1. The most common pathogen isolated in septic arthritis of the TMJ is Staphylococcus aureus, followed by Neisseria, Haemophilus influenzae, and Streptococcus4.
Several laboratory parameters are also useful for diagnosis, such as white blood count with differential and C-reactive protein testing1. The serum leukocyte count can be normal or increased due to antibiotic use.
C-reactive protein level indicates the severity of disease quite accurately. It may be used to identify disease resolution and may be increased at the initial stage8. In this case, we suspected septic arthritis based on clinical and radiographic examinations. Therefore, we performed arthrocentesis for diagnosis and management, and aspirated turbid and semitransparent fluid. Staphylococcus aureus was found on culture of the aspirated fluid, which is known to be common in septic arthritis.
In terms of treatment, no definitive concurrence on the management of TMJ septic arthritis has been reached2. In general, appropriate joint drainage, antimicrobial treatment, and joint immobilization are recommended. However, surgical drainage methods are controversial as no single diagnostic criterion has been proven48.
Empiric medication with antibiotics should be started immediately when acute septic arthritis has been diagnosed. Broad-spectrum antibiotics such as intravenous penicillins or cephalosporins are often used and can be changed to an oral regimen after the joint infection is under control1. Antibiotics should be tailored according to culture and sensitivity tests.
In the acute period, septic arthritis may be managed by aspiration alone with the addition of arthrotomy and washout for pediatric patients5. Aspiration of the infected synovial fluid in addition to antibiotic administration are used for the treatment of TMJ. Within 48 to 72 hours after drainage, the infected joints become sterile. Different surgical drainage methods such as needle aspiration, arthroscopy, and arthrotomy have been described1. Mouth opening restriction can occur after acute inflammation, so exercises are highly recommended to recover the length of mouth opening. In this patient, joint drainage with arthrocentesis and a 14-day course of antibiotics taken for 14 days were prescribed. Physical therapy and active mouth opening exercises improved mouth opening to 35 mm.
In conclusion, septic arthritis may be confused with other temporomandibular disorders. Therefore, when a patient presents with pain, fever, swelling, preauricular edema, trismus, and acute malocclusion, septic arthritis should be considered depending on imaging findings, joint aspiration, aspirated fluid analysis, and laboratory examination. Septic arthritis can be managed with antibiotics, surgical drainage, and joint immobilization.
Go to : 
References
1. Cai XY, Yang C, Zhang ZY, Qiu WL, Chen MJ, Zhang SY. Septic arthritis of the temporomandibular joint: a retrospective review of 40 cases. J Oral Maxillofac Surg. 2010; 68:731–738. PMID: 19954877.

2. Klüppel LE, Bernabé FB, Primo BT, Stringhini DJ, da Costa DJ, Rebellato NL, et al. Septic arthritis of the temporomandibular joint. J Craniofac Surg. 2012; 23:1752–1754. PMID: 23147304.

3. Parmar J. Case report: septic arthritis of the temporomandibular joint in a neonate. Br J Oral Maxillofac Surg. 2008; 46:505–506. PMID: 18282642.

4. Leighty SM, Spach DH, Myall RW, Burns JL. Septic arthritis of the temporomandibular joint: review of the literature and report of two cases in children. Int J Oral Maxillofac Surg. 1993; 22:292–297. PMID: 8245570.

5. Bounds GA, Hopkins R, Sugar A. Septic arthritis of the temporomandibular joint--a problematic diagnosis. Br J Oral Maxillofac Surg. 1987; 25:61–67. PMID: 2948546.

6. Gayle EA, Young SM, McKenna SJ, McNaughton CD. Septic arthritis of the temporomandibular joint: case reports and review of the literature. J Emerg Med. 2013; 45:674–678. PMID: 23896057.
7. Trimble LD, Schoenaers JA, Stoelinga PJ. Acute suppurative arthritis of the temporomandibular joint in a patient with rheumatoid arthritis. J Maxillofac Surg. 1983; 11:92–95. PMID: 6575113.

8. Sembronio S, Albiero AM, Robiony M, Costa F, Toro C, Politi M. Septic arthritis of the temporomandibular joint successfully treated with arthroscopic lysis and lavage: case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:e1–e6. PMID: 17095265.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download