Abstract
In prolonged chronic osteomyelitis, chronic inflammation and low-grade infections can result in new periosteal bone formation. Chronic osteomyelitis with proliferative periostitis (traditionally termed Garré's sclerosing osteomyelitis) mainly affects children and young adults. Here, we present two rare cases of an 11-year-old and a 12-year-old patient with suppurative chronic osteomyelitis with proliferative periostitis without any definitive infection source, such as dental caries or periodontitis. The source of infection was likely to be related to the development of a lower right third molar germ with follicular space widening. Management involved antibiotics and the removal of the third molar germ and surgical debridement. Disease remission and a normal appearance was observed at the six-month follow-up visit.
Osteomyelitis is an inflammatory condition of the bone and bone marrow. The pathogenesis of osteomyelitis of the jaw is predominantly odontogenic microorganisms. Bacterial infection of odontogenic origin can be in the form of a periapical or periodontal abscess, pericoronitis, infected extraction wound, or fracture wound1. Bony pathology such as osteomyelitis, trauma, and neoplastic disease can result in mild irritation or low-grade infection that can affect the jaw and lead to peripheral subperiosteal bone deposition. The differential diagnoses of bony expansion also comprise Ewing's sarcoma, fibrous dysplasia, osteogenic sarcoma, infantile cortical hyperstosis, exostosis, calcifying hematoma, and osteoma.
Osteomyelitis of the mandible due to an impacted third molar occurs very rarely. Only a few case reports have been published. The basic treatment strategy in these reports was removal of the impacted third molar. Further surgical interventions varied from curettage and drainage to condylectomy, coronoidectomy, or extensive decortication. Chronic suppurative osteomyelitis can only be treated successfully by a combination of antimicrobial therapy and surgery for total elimination of the infected and necrotic bony tissue. This approach can lead to complete cure of osteomyelitis and further resolution of proliferative periostitis. Early-onset primary chronic osteomyelitis (juvenile chronic osteomyelitis) differs from secondary chronic suppurative osteomyelitis, which is characterized by recurring periosteal reaction without complete resolution.
A 12-year-old girl was referred to the Department of Oral and Maxillofacial Surgery, Seoul National University Dental Hospital (Seoul, Korea), with a six-week history of recurrent pain and swelling of the right mandible, which had increased over the past month. Under the assumption that an infection was present, the patient had been treated with antibiotics for three weeks and underwent needle aspiration for drainage at a local dental clinic.
There was prominent right facial swelling, erythema, and tenderness at the angle and inferior border of the mandible.(Fig. 1) No cutaneous fistula was present on the first day. Several days later, a cutaneous fistula had formed. There was regional lymphadenopathy, but sensation of lower lip and chin area was intact.
On intra-oral examination, the patient had full, well-maintained dentition with erupting second molars. There were no caries lesions or periodontal pathology. No intra-oral draining sinus was found. She denied fevers or chills and difficulty swallowing or talking. The maximal inter-incisal opening was 15 mm due to guarding secondary to pain.
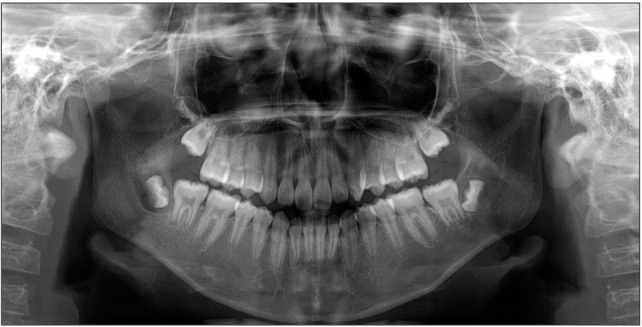
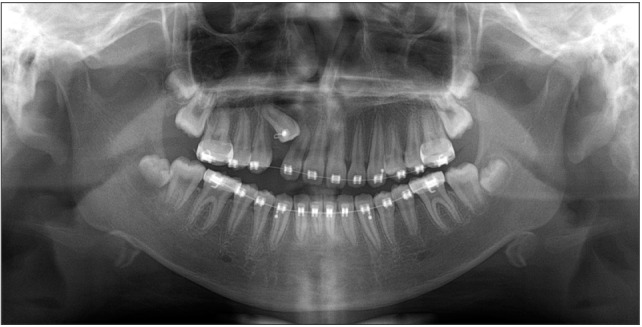
A panoramic radiograph was taken as an initial diagnostic study. There was overall sclerosis on the body and angle of the right mandible. There was a lytic lesion (bony crypt) on the right mandibular third molar.(Fig. 2) A prominent proliferative periosteal reaction was present on the angle, body, and sigmoid notch area of the right mandible.(Fig. 3)
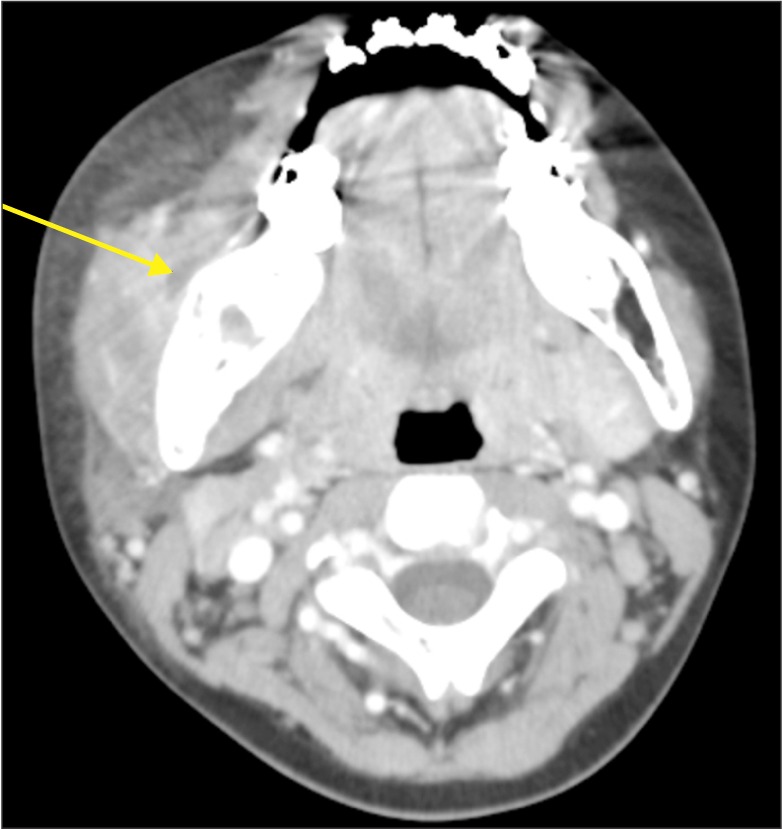
A two-dimensional computed tomography (CT) scan with contrast material was taken for evaluation of suspected osteomyelitis. The CT image showed widening of the follicular space of the right mandibular third molar with definitive cortical perforation on the buccal and lingual sides accompanied by an outer cortical periosteal reaction.(Fig. 4) The attenuation of bone marrow on the body of the right mandible was increased. Pus formation was observed on the buccal side of the third molar germ. Based on the clinical findings and radiographic imaging, a provisional diagnosis of chronic suppurative osteomyelitis of the mandible with proliferative periostitis was made.
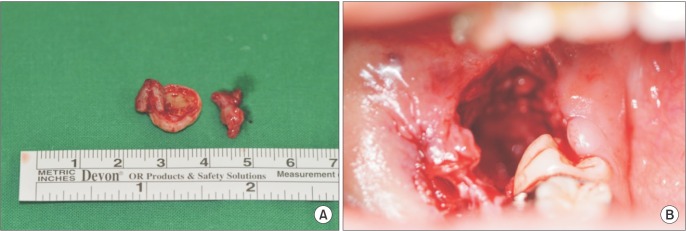
Surgical management including saucerization and germectomy under general anesthesia were planned. First, the lesion was drained through the cheek, and microbial cultures were collected.(Fig. 5. A) An incision was made along the external oblique ridge, and a mucoperiosteal flap was elevated. We observed destruction of alveolar bone distal to the second molar. The right mandibular third molar tooth germ was surgically extracted, followed by debridement and saucerization of the extraction site.(Fig. 5. B, 5. C) Histological samples were collected, and a drain was inserted for further pus drainage and left in place for two weeks.
Antibiotic treatment with a first-generation cephalosporin and clindamycin was continued for two weeks after surgical treatment. Resolution of inflammation with decreases in high-sensitivity C-reactive protein (hs-CRP) rate and swelling and increased mouth opening was achieved one week after surgery. Microbiological culture yielded only commensal organisms. The histopathology demonstrated the presence of inflammatory granulation tissue around the tooth germ. After one month of follow-up, the swelling and infection had resolved, but the bony expansion remained due to residual proliferative periostitis. After six months of follow-up, the patient exhibited restored facial symmetry with normal bony contour of the mandible on radiographic examination.
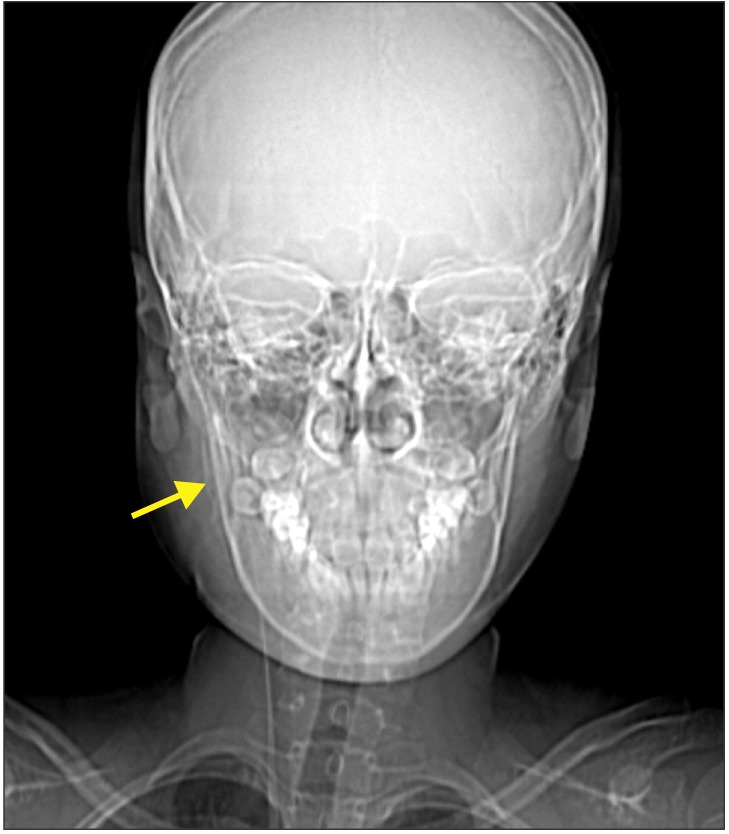
An 11-year-old female was referred from the Department of Pediatric Dentistry with progressive swelling and abscess of the right mandible.(Fig. 6) She had presented to the hospital with the same chief complaint two weeks prior. At that time, she was prescribed amoxicillin syrup 250 mg three times a day and ibuprofen syrup 200 mg three times a day for five days with chlorhexidine mouth rinse, which were very effective and rapidly relieved her symptoms. Her symptoms returned and were then interpreted as salivary gland inflammation and pariostitis by her pediatrician four days prior, and antibiotics were again prescribed. Her swelling and trismus worsened, and she was admitted and underwent enhanced CT scanning. A course of intravenous metronidazole and amoxicillin clavulanate was prescribed. She had tender swelling over the right mandibular angle and ramus. Her mouth opening was limited to 11 mm between her incisors.
Radiological examination revealed loss of the right mandibular third molar follicular cortex with peripheral diffuse bone destruction and new periosteal bone formation and an increase in bone marrow attenuation.(Fig. 7) Focal abscess formation was also seen.(Fig. 8) Under the diagnosis of osteomyelitis with cellulitis and focal abscess, immediate intraoral incision and drainage of the right mandibular posterior buccal vestibule were performed.
Three days after the incision and drainage, she had symptomatically improved, and her erythrocyte sedimentation rate and hs-CRP had decreased from 51 to 30 mm/hr and from 3.95 to 0.7 mg/dL, respectively. The next day, she underwent surgical extraction of the third molar germ and saucerization.(Fig. 9)
The histology report confirmed the diagnosis of osteomyelitis of the mandible. She was discharged three days later. After two weeks of follow-up, there was dramatic resolution of her swelling.(Fig. 10)
Only a few cases of osteomyelitis of the mandible due to an impacted third molar have been published in the literature. Reck et al.2 reported a case of osteomyelitis of the coronoid process as a consequence of third molar pericoronal infection in a 16-year-old boy, who was treated with tooth extraction and partial coronoidectomy. Mohammed-Ali et al.3 reported cases of osteomyelitis secondary to pericoronitis. One was osteomyelitis of the mandibular ramus originating from the lower left third molar in a 22-year-old female, the treatment of which was tooth extraction and exploration and drainage from the left submasseteric space. The other was a case of sclerosing osteomyelitis in the lower right third molar extraction space in a 21-year-old female that was treated with extensive decortication. Cases of condylar osteomyelitis due to an ectopic third molar in a 35-year-old female4 and a lower left third molar in a 37-year-old male5 have also been reported; treatment was extraction, curettage, and drainage. Very similar to our case, Tong et al.6 reported a case of chronic osteomyelitis with proliferative periostitis affecting the mandibular angle of a 12-year-old male patient secondary to an un-erupted lower third molar. All of the reported cases, except that by Tong et al.6, were secondary to pericoronitis of a fully developed impacted third molar, not a tooth germ. In contrast, proliferative periostitis was prominent in our case.
Chronic osteomyelitis of the jaw in adolescents and young adults is often accompanied by bony expansion. Since Carl Garré first described an irritation-induced focal thickening of the periostium and cortical bone of the tibia in 1893, this phenomenon has been more accurately termed chronic osteomyelitis with proliferative periostitis, with periosteal reaction of new bone formation concentrically around the cortex7. When osteomyelitis exists with no infection source or it is a non-suppurative type, such as early-onset primary chronic osteomyelitis (juvenile chronic osteomyelitis), treatment varies from only NSAID medication to massive surgical intervention such as partial resection of the mandible8. Eyrich et al.8 reported 11 cases of primary chronic osteomyelitis in children and adolescents ranging in age from 4.5 to 17 years, with pain, swelling, local induration, and accompanying proliferative periostitis. Three of these patients experienced relapse, and one demonstrated no improvement during the observation period. Heggie et al.9 also reported eight cases of juvenile mandibular chronic osteomyelitis ranging in age from 7 to 12 years, the treatment and outcome/recurrence of which varied. Those cases were all examples of primary inflammatory disease with unknown etiology, different from our case of confirmed infection and definitive purulent discharge with secondary chronic osteomyelitis.
In cases of secondary chronic suppurative osteomyelitis, management is a course of antibiotics in combination with surgical debridement10. In the present cases, the patients were prescribed antibiotics in combination with surgical extraction of the third molar germ, debridement, and saucerization. After two weeks of follow-up, the soft tissue swelling and infection had resolved. The bony expansion from proliferative periostitis had also resolved, and the patient had regained facial symmetry.
In conclusion, for unknown reasons, hematogenous infection can occur, resulting in low-grade infection and inflamed granulation tissue formation around the fully impacted third molar germ. This infection can act as a source of chronic inflammation of bone and lead to periosteal reaction, especially in juveniles. A combination of antibiotic therapy, germectomy, and surgical debridement was effective in the treatment of chronic suppurative osteomyelitis with proliferative osteitis.
References
1. Hudson JW. Osteomyelitis of the jaws: a 50-year perspective. J Oral Maxillofac Surg. 1993; 51:1294–1301. PMID: 8229407.

2. Reck SF, Fielding AF, Hess DS. Osteomyelitis of the coronoid process secondary to chronic mandibular third molar pericoronitis. J Oral Maxillofac Surg. 1991; 49:89–90. PMID: 1985188.

3. Mohammed-Ali RI, Collyer J, Garg M. Osteomyelitis of the mandible secondary to pericoronitis of an impacted third molar. Dent Update. 2010; 37:106–108. PMID: 20415010.

4. Lambade P, Lambade D, Dolas RS, Virani N. Ectopic mandibular third molar leading to osteomyelitis of condyle: a case report with literature review. Oral Maxillofac Surg. 2013; 17:127–130. PMID: 22847038.

5. Wang R, Cai Y, Zhao YF, Zhao JH. Osteomyelitis of the condyle secondary to pericoronitis of a third molar: a case and literature review. Aust Dent J. 2014; 59:372–374. PMID: 24819410.

6. Tong AC, Ng IO, Yeung KM. Osteomyelitis with proliferative periostitis: an unusual case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 102:e14–e19. PMID: 17052617.

7. Benca PG, Mostofi R, Kuo PC. Proliferative periostitis (Garré's osteomyelitis). Oral Surg Oral Med Oral Pathol. 1987; 63:258–260. PMID: 3469611.

8. Eyrich GK, Baltensperger MM, Bruder E, Graetz KW. Primary chronic osteomyelitis in childhood and adolescence: a retrospective analysis of 11 cases and review of the literature. J Oral Maxillofac Surg. 2003; 61:561–573. PMID: 12730835.

9. Heggie AA, Shand JM, Aldred MJ, Talacko AA. Juvenile mandibular chronic osteomyelitis: a distinct clinical entity. Int J Oral Maxillofac Surg. 2003; 32:459–468. PMID: 14759102.

10. van Merkesteyn JP, Groot RH, van den Akker HP, Bakker DJ, Borgmeijer-Hoelen AM. Treatment of chronic suppurative osteomyelitis of the mandible. Int J Oral Maxillofac Surg. 1997; 26:450–454. PMID: 9418149.

Fig. 1
Clinical photos. A. Swelling of the right mandible. B. Lateral view. C. Intraoral photo showing pericoronitis of the lower second molar.

Fig. 4
Computed tomography image reveals cortical perforation around the right third molar follicle and pus formation.
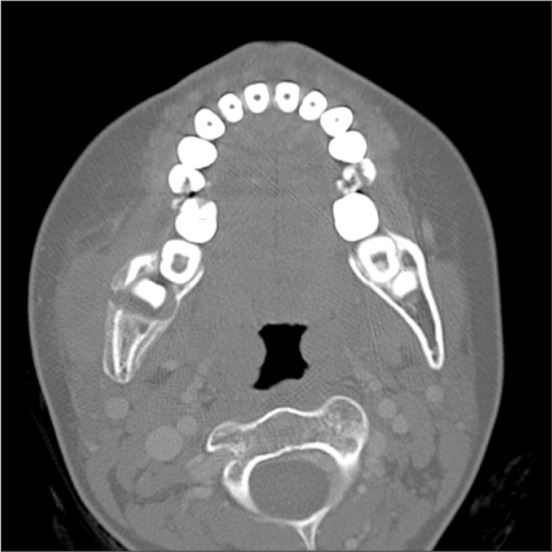
Fig. 5
Surgical intervention. A. Initial presentation of the cutaneous sinus and pus discharge. B. Extraction of the tooth germ. C. Intraoral lesions after surgical debridement.
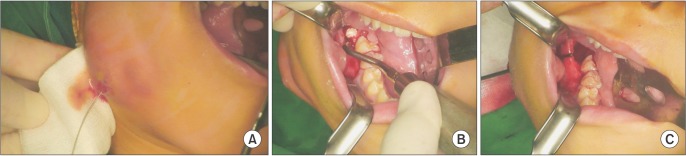
Fig. 6
Clinical photos. A. Swelling of the right mandible. B. Oblique view. C. Erupting second molar covered with operculum. A drain was introduced.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download