Abstract
Actinomycosis is an infection caused by the actinomyces genus and is associated with trauma or previous infection. A 58-year-old male patient was referred from a private dental clinic for root extraction of the lower right molar. The x-ray showed fractured root-like material distal to the distal root of the lower right second molar. A biopsy during extraction of the root-like material was performed, which revealed a sequestrum with actinomycosis by a pathological examination. In this case, the radiopacity of the suspicious lesion was higher than that of the surrounding alveolar bone, which confused it with the root tip. The diagnosis of actinomycosis required long-term antimicrobial therapy, which is very different from simple extraction or removal of sequestrum.
Go to : 
Actinomycosis is an infection caused by bacteria of the Actinomyces genus and is associated with trauma or previous infection1. An actinomycotic infection usually affects soft tissues and rarely occurs in bones2. This infection is characterized by sulfur granules and suppurative, granulomatous inflammation with abscess and fistula23. A dental origin is typical for cervicofacial actinomycosis (CFA), which is usually limited to the soft tissue without bone involvement3.
The diagnosis of actinomycosis can be complicated by its resemblance to common clinical symptoms such as osteomyelitis, cement-osseous dysplasia, and periodontitis1456; this complication can increase the risk to patient health when vital organs are involved7. In addition, although antimicrobial treatment is effective, the treatment occurs over a long time period3.
This article presents an unusual case of actinomycosis that involved alveolar bone without definite symptoms, which was confused with a retained root tip after incomplete tooth extraction.
Go to : 
A 58-year-old male patient, who has been medicated for hypertension and diabetes mellitus, was referred from a private dental clinic for extraction of a retained root tip. The patient reported extraction of the lower right third molar about one year prior. He presented for irritation of the lingual gingiva distal to the lower right second molar. However, he did not report any pain or swelling. The need for extraction of a fractured root of the second molar was written in the referral paper even though the patient insisted that the root of the third molar had been left intact after the third molar extraction.
The oral examination revealed root-like material with dentin-like color extruding from the lingual aspect of the extraction site. However, there was no gingival swelling or any sign of inflammation around the lesion.(Fig. 1)
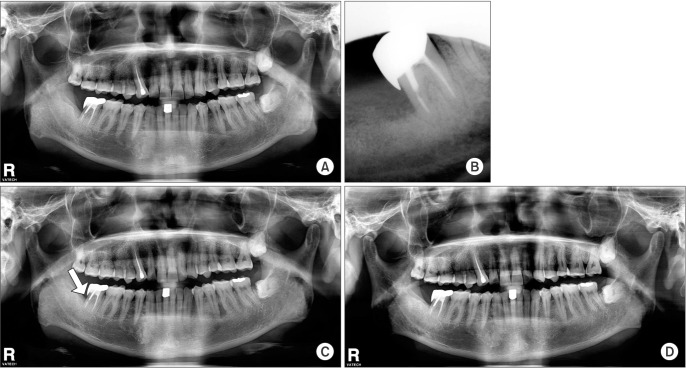
The panoramic radiograph showed root-like material distal to the root of the mandibular right second molar, which was more radiopaque than the surrounding alveolar bone.(Fig. 2, 3)
According to the patient's history, symptoms, clinical, and radiological examination, the lesion was thought to be a retained root tip of the third molar. Therefore removal of the lesion with biopsy was planned without further examination such as computed tomography or microbial identification.
A biopsy was performed during removal of the lesion. The removed lesion was yellow-colored, root- or bone-like hard material and was sent for pathological examination. The patient was treated with Augmentin 625 mg (amoxicillin/clavulanate) every 8 hours and non-steroidal anti-inflammatory drugs for 5 days. Pathological examination on the day of suture removal revealed the lesion to be actinomycosis based on bone fragment filled with sulfur granules and aggregates of Actinomyces on hematoxylin and eosin staining.(Fig. 4)
Therefore, the patient restarted antimicrobial therapy with Augmentin for 2.5 months and was regularly followed-up. (Fig. 5) After 10 months, the patient remained in good health without symptoms, and the radiograph showed bony healing without any sign of infection.
Go to : 
The present study reported a case of unusual actinomycosis without abscess or fistula, which was confused with a retained root tip.
Actinomycosis, as an opportunistic infection, often affects patients with certain medical conditions such as cancer, immunodeficiency, and malnutrition89. Actinomyces are gram-positive anaerobic bacteria that do not cause infection when they remain on the mucosal surface. However, when the mucosal barrier is compromised, an inflammatory process can be initiated8.
CFA is the most common form of actinomycotic infection10. In addition to CFA, actinomycotic infection is a potential complication in bisphosphonate-related osteonecrosis of the jaw and osteoradionecrosis11.
Extended antimicrobial therapy has been recommended for actinomycosis infection in order to prevent disease recurrence3. The duration of antibiotics depends on the severity of the disease, the site of infection, and the clinical and radiological response to the treatment12. Actinomycotic infections are sensitive to many antibiotics, with penicillin being the drug of choice13. The combination of penicillin and a beta-lactamase inhibitor is recommended because of the advantage of coverage against penicillin-resistant aerobic and anaerobic pathogens359. Surgical excision or debridement is also recommended, especially in cases of necrotic tissue, fistulas, or neoplasms313.
Due to the opportunistic character of actinomycotic infection, early and adequate diagnosis prior to therapy is important to prevent the spread of disease14.
More routine biopsies of tissue removed from the oral cavity might be beneficial for the differential diagnosis of actinomycosis infections.
In conclusion, actinomycosis is an infection that can be confused with other common pathologic conditions. However, it should be differentiated because of the need for long-term antibiotic therapy. In this case, the patient's history of tooth extraction and the shape of the lesion were confusing enough to misdiagnose the actinomycosis infection as a retained root tip. The diagnosis resulted in long-term antibiotic therapy rather than simple root tip extraction, which ended with an ideal outcome.
Go to : 
References
1. Finley AM, Beeson MS. Actinomycosis osteomylelitis of the mandible. Am J Emerg Med. 2010; 28:118.e1–118.e4. PMID: 20006231.

2. Sharkawy AA. Cervicofacial actinomycosis and mandibular osteomyelitis. Infect Dis Clin North Am. 2007; 21:543–556. viiiPMID: 17561082.

3. Brook I. Actinomycosis: diagnosis and management. South Med J. 2008; 101:1019–1023. PMID: 18791528.

4. Smith MH, Harms PW, Newton DW, Lebar B, Edwards SP, Aronoff DM. Mandibular Actinomyces osteomyelitis complicating florid cemento-osseous dysplasia: case report. BMC Oral Health. 2011; 11:21. PMID: 21777471.

5. Kim NR, Park JB, Ko Y. Differential diagnosis and treatment of periodontitis-mimicking actinomycosis. J Periodontal Implant Sci. 2012; 42:256–260. PMID: 23346471.

6. Rankow RM, Abraham DM. Actinomycosis: masquerader in the head and neck. Ann Otol Rhinol Laryngol. 1978; 87:230–237. PMID: 646293.

7. Bennhoff DF. Actinomycosis: diagnostic and therapeutic considerations and a review of 32 cases. Laryngoscope. 1984; 94:1198–1217. PMID: 6381942.
8. Kaplan I, Anavi K, Anavi Y, Calderon S, Schwartz-Arad D, Teicher S, et al. The clinical spectrum of Actinomyces-associated lesions of the oral mucosa and jawbones: correlations with histomorphometric analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:738–746. PMID: 19748292.

9. Won HR, Park JH, Kim KS. Simultaneous actinomycosis with aspergillosis in maxillary sinus. Br J Oral Maxillofac Surg. 2013; 51:e51–e53. PMID: 22445647.

10. Figueiredo LM, Trindade SC, Sarmento VA, de Oliveira TF, Muniz WR, Valente RO. Actinomycotic osteomyelitis of the mandible: an unusual case. Oral Maxillofac Surg. 2013; 17:299–302. PMID: 23239430.

11. Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005; 63:1567–1575. PMID: 16243172.

12. Choi J, Koh WJ, Kim TS, Lee KS, Han J, Kim H, et al. Optimal duration of IV and oral antibiotics in the treatment of thoracic actinomycosis. Chest. 2005; 128:2211–2217. PMID: 16236876.

13. Sun CX, Henkin JM, Ririe C, Javadi E. Implant failure associated with actinomycosis in a medically compromised patient. J Oral Implantol. 2013; 39:206–209. PMID: 21767210.

14. Sakallioğlu U, Açikgöz G, Kirtiloğlu T, Karagöz F. Rare lesions of the oral cavity: case report of an actinomycotic lesion limited to the gingiva. J Oral Sci. 2003; 45:39–42. PMID: 12816363.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download