Abstract
Purpose
To study the clinical application of low-dose unenhanced computed tomography with iterative reconstruction technique (LDCT-IR) on renal colic in the emergency department.
Materials and Methods
We conducted a prospective, single-blinded, randomized, and non-inferiority study. From March 2014 to August 2015, 112 patients with renal colic were included, and were randomized to either LDCT-IR (n=46) or standard-dose unenhanced CT (SDCT) (n=66) groups. The accuracy of urolithiasis diagnosis was the primary endpoint of this study. Radiation dose, size and location of the stone, hydronephrosis, other diseases except urolithiasis, and results of treatment were analyzed between the two groups.
Results
The average effective dose radiation of SDCT was approximately four times higher than that of LDCT-IR (6.52 mSv vs. 1.63 mSv, p<0.001). There was no significant difference in the accuracy of ureteral stone diagnosis between the two groups (LDCT-IR group: 96.97% vs. SDCT group: 98.96%, p=0.392). No significant difference was observed regarding the size and location of a stone, hydronephrosis, and diagnosis of other diseases, except urolithiasis. False negative results were found in two LDCT-IR patients and in one SDCT patient. In these patients, stones were misread as vascular calcification, and were difficult to diagnose because evidence of hydronephrosis and ureteral dilatation was not found.
Ureter stones are a common health problem in Korea with noted increases in their incidence, prevalence, and recurrence. In general, 50% of patients with recurrence have one recurrent episode, whereas more than 10% have multiple recurrences.1234 Recently, unenhanced computed tomography (CT) with a thin section and multi-detector has been increasingly used for renal colic patients because it provides a rapid and accurate examination.56 Furthermore, unenhanced CT has become the new diagnostic gold standard due to its ability to identify other causes of renal colic, as well as its higher sensitivity and specificity for the detection of ureter stones, compared to other modalities, such as intravenous pyelography or ultrasonography.7
With the widespread use of unenhanced CT for the diagnosis of ureter stones, radiation exposure has become a major concern. Although the risk induced by an individual unenhanced CT scan is minute, the lifetime cumulative effect from a large number of exposures might confer a risk for cancer in young ureter stone patients who have multiple recurrences.8 Therefore, the “as low as reasonably achievable” (ALARA) principle is used to achieve the lowest radiation dose possible during unenhanced CT examinations while maintaining optimal image quality.9 Reducing radiation exposure during the evaluation of renal colic is now one of the main focuses in the field of urology, and low-dose unenhanced CT (LDCT) is the most promising option for diagnosing ureter stones. The recently introduced iterative reconstruction (IR) algorithms for CT have shown promise with regards to dose reduction, compared with standard filtered back projection (FBP), and these algorithms were found to reduce image noise in our previous studies using phantom and clinical trials of renal colic patients.101112 However, these studies have several limitations. In a phantom study, the phantom has a simple constitution, compared with the human body. In addition, a stone with a fixed size in the hole of a phantom could make the diagnosis of urolithiasis rather simple.11 In previous clinical trials, we repeated CT scans at the same time with different settings (standard dose and low dose).10 This approach can lead to enrolment limits regarding the number of patients, as well as significant ethical issues, although we obtained informed consent and provided a thorough explanation. Herein, we evaluated the efficacy of LDCT with the use of the IR technique (LDCT-IR) for reducing the radiation dose and image noise while maintaining clinical usefulness via a prospective and randomized study.
This prospective study was approved by the Institutional Review Board of Chung-Ang University Hospital [IRB No. C2012234 (1194)], and informed consent was obtained from all patients who were enrolled in this study. We attempted to conduct a prospective, single blind, randomized, and non-inferiority study at a single university hospital.
From March 2014 to August 2015, 1142 patients over 19 years of age with renal colic who visited the emergency department were recruited. We relied on the assessment performed by emergency physicians that led to a clinical suspicion of ureter stones. Patients who had signs and symptoms of a urinary tract infection and those with unstable vital signs were excluded. We informed the patients about this prospective study and acquired consent from patients who were scheduled to undergo an unenhanced CT scan. Patients who did not want to participate in this study and those who did not provide informed consent were also excluded. Patients who provided written informed consent were randomly assigned to undergo either LDCT-IR or standard-dose unenhanced CT (SDCT) of the abdomen and pelvis. Although the emergency physician was aware of the group assignments, owing to the obvious difference in the textures of the CT images, neither the patients nor the outcome assessors were aware of these assignments.
All of the CT scans were performed with a 256-multi-detector computed tomography scanner (Brilliance iCT, Philips Healthcare, Cleveland, OH, USA). As previously described, SDCT (with a tube voltage of 120 kV and tube current-time product of 150 mAs) or LDCT (with a tube voltage of 100 kV and tube current-time product of 60 mAs) were performed for the detection of ureter stones, and an automatic exposure control (Doseight, Philips Healthcare) according to the patient’s body mass index was used in all of the scans.1012 The FBP technique was applied to reconstruct the SDCT images, and the IR technique (iDose reconstruction technique, level 5, Philips Healthcare) was applied for the LDCT images.1012
The actual radiation dose was generated directly from the CT scanner, and was recorded in terms of the dose-length products (DLPs). The DLPs were converted into the effective dose (ED; in mSv) by multiplying the conversion coefficient 0.015 mSv/mGy/cm. The reduction rates of both the DLP and ED were compared between the two scans.
During the daytime, CT reports were initially prepared by one of two expert radiologists who had participated in previous research on LDCT-IR, and for CT examinations performed afterhours, preliminary reports were provided by on-call radiologists who had limited experience in interpreting LDCT images.1012 The preliminary reports were supplemented by additional reports from expert radiologists. However, these addenda were not included in the outcome analysis since we could not objectively determine how they might affect clinical decisions. All of the interpreting radiologists were able to access the clinical and laboratory findings and consult with the referring physician. The CT reports conformed to a predefined structured format, indicating the likelihood of ureter stones on a four-point scale (none, low possibility, high possibility, and ureter stone) according to the presence of pyeloureterectasis, perinephric and periureteral soft tissue standing, comet tail signs, soft tissue rim sign, and location of stones. The maximal in-plane stone diameters were measured using electric calipers.5 If the diagnosis of ureter stone remained indeterminate after the initial CT examination and clinical observation or medical therapy, additional abdominal ultrasound, intravenous pyelography, or SDCT could be performed at the discretion of the physicians or urologists on call.
Depending on the urgency of CT, the urologists decided on immediate management or pain control, and patients who were managed by pain control were followed-up to establish the final diagnosis and results of the urological interventions [medical expulsion therapy (MET), extracorporeal shock wave lithotripsy (ESWL), retrieval of a stone by cystoscopy, ureteroscopy, or nephroscopy].
The primary endpoint was stone detection rate according to the final clinical diagnosis, and the secondary endpoints for the clinical outcomes included differences in the clinical manifestation of patients and reductions in the rates of both the DLP and ED between the LDCT-IR and SDCT groups.
All statistical analyses were performed using IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA), and the differences were considered statistically significant at a p-value of <0.05. The sensitivity, specificity, and accuracy of the LDCT-IR and SDCT techniques for the diagnosis of ureter stones were calculated. Fisher’s exact test and the Mann-Whitney U test were used to compare the performances of the two assessments and secondary endpoints.
During the study period, 112 patients who provided informed consent were randomly assigned to either the LDCT-IR (46 patients) or SDCT (66 patients) group (Fig. 1). Eleven patients of the LDCT-IR group and 15 patients of the SDCT group were lost to follow-up after discharge, and the remaining 35 patients in the LDCT-IR group and 51 patients in the SDCT group were included in the outcome analyses. There were no differences in age, sex, and history of a previous ureter stone between the two groups, and the mean body mass index was also similar between the two groups (24.4 kg/m2 in the LDCT-IR group vs. 23.9 kg/m2 in the SDCT group) (Table 1).
The average DLP (108.4 mGy vs. 434.8 mGy, p<0.001) and ED (1.63 mSv vs. 6.52 mSv, p<0.001) were significantly decreased in the LDCT-IR group, compared with the SDCT group, and the estimated dose reduction of ED with LDCT-IR relative to SDCT was 75.2% (Table 1).
In regard to the likelihood of ureter stones on the four-point scale, the incidence of ureter stones was no different between the two groups (84.8% in the LDCT-IR group vs. 89.4% in the SDCT group, p=0.978). A low possibility was observed in 5 patients (3 in the LDCT-IR group and 2 in the SDCT group) and a high possibility was observed in 5 patients (2 in the LDCT-IR group and 3 in the SDCT group) (Table 1). Additionally, the incidence of hydronephrosis (80.4% in the LDCT-IR group vs. 89.4% in the SDCT group, p=0.183) and incidence of stone multiplicity (28.3% in the LDCT-IR group vs. 33.3% in the SDCT group, p=0.569) were similar between the two groups (Table 1).
Table 2 shows the stone characteristics of both groups, and 60 stones in the LDCT-IR group and 114 stones in the SDCT group were detected. The mean size of stones was 3.86 mm in the LDCT-IR group and 3.91 mm in the SDCT group (p=0.861), and stones less than 4 mm totalled 32 (53.3%) in the LDCT-IR group and 62 (54.4%) in the SDCT group. The major site of the stones was similar between the two groups [left ureter stones: 31 (51.7%) in the LDCT-IR group and 62 (54.4%) in the SDCT group], and lower ureter stones [19 (31.7%) in the LDCT-IR group and 37 (32.5%) in the SDCT group]. We did not find any differences in the size, site, and location of the ureter stones between the two groups.
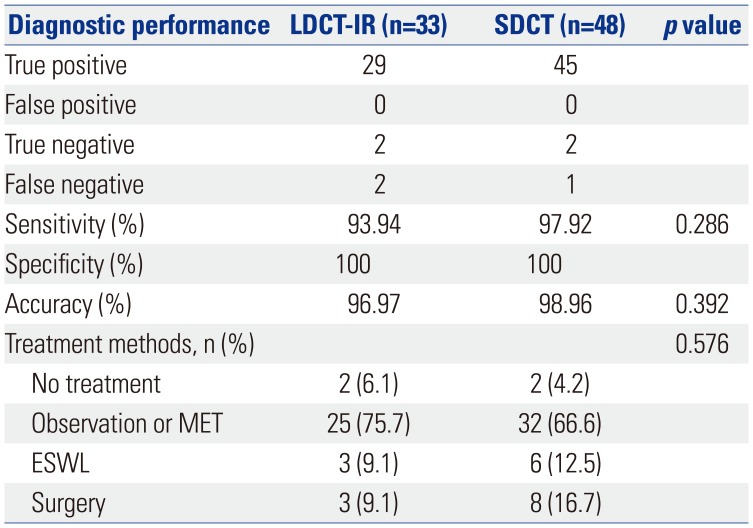
Thirty-one patients (88.9 %, 31 of 35 patients) in the LDCT-IR group and 47 patients (92.2 %, 47 of 51 patients) in the SDCT group had clinically proven stones (Fig. 2). When a scoring system with two categories (stone probability: 1 and 2=none, 3 and 4=stone present) was used, three patients (2 in the LDCT-IR group and 1 in the SDCT group) had a documented vascular calcification rather than ureteral stones (probability: 2) that was clinically proven to be a ureter stone (false negatives) (Fig. 3A-C). Unsuspected diseases beyond ureter stones were identified in one patient with acute diverticulitis in the SDCT group (Fig. 3D). The sensitivity and specificity of the LDCT-IR were 93.94 % and 100%, respectively, and those for the SDCT were 97.92 % and 100%, respectively. The accuracy of LDCT-IR and SDCT for the detection of symptomatic ureteral stones did not show any differences between the two groups (96.97 vs. 98.96, p=0.392) (Table 3).
Most patients (27 in the LDCT-IR group and 35 in the SDCT group) had documented spontaneous stone passing by MET or observation, and 11 patients (3 in the LDCT-IR group and 8 in the SDCT group) underwent endoscopic stone fragmentation and removal via cystoscopy, rigid or flexible ureteroscopy, whereas 9 patients (3 in the LDCT-IR group and 6 in the SDCT group) showed stone fragmentation by ESWL (Table 3). The pattern of stone management in the two groups was found to be similar (p=0.576).
In our study, the LDCT-IR scan was not inferior to the SDCT scan for the stone detection rate according to the final clinical diagnosis and clinical outcomes, which included the difference in the clinical manifestations of patients. Moreover, LDCT-IR reduced the radiation dose to 75.2%, compared to SDCT. This means that the LDCT-IR scan is useful for evaluation of renal colic patients and for the diagnosis of ureter stones in the ED, with an overall sensitivity and specificity of 93.9% and 100%, respectively.
In our study, we used LDCT-IR to decrease the image noise accompanied by radiation dose reduction. Malkawi, et al.13 reported that LDCT scan (10%) without any post-processing noise reduction techniques was inferior to SDCT scan for the evaluation of renal colic patients, and had an overall sensitivity and specificity of 70% and 39%, respectively. However, Kwon, et al.10 investigated 116 patients with suspicious ureter stones by LDCT-IR, and the mean ED was 1.39 mSv, which showed a 76.6% reduction. The sensitivity and specificity of LDCT-IR were 99.1% and 100%, respectively, and it had a diagnostic accuracy of 100% for stones greater than 3 mm. Park, et al.14 investigated 103 patients by LDCT-IR and observed a mean ED of 0.68 mSv. An accuracy of 100% for ureteral stones more than 3 mm in diameter was achieved with an approximately 91.82% reduction of the radiation dose.
Application of LDCT-IR is suitable for the detection of ureter stones because of its high contrast between almost all ureter stones and the adjacent lower density soft tissue. However, this difference may be inaccurately placing the calcifications on LDCT without IR inside or outside of the ureter, and it is difficult to distinguish ureteral stones and phleboliths with vascular calcifications. This placement error is due to the loss of resolution at the thin ureter, and the reason for this loss is that LDCT is not designed to evaluate soft tissue. This problem would apply to all ureteral stones without ureteral dilatation or hydronephrosis. However, the IR technique is available for low contrast abdominal soft structures, and this technique is thus applicable for distinguishing between ureteral stones and phleboliths.10 Therefore, we believe that the IR technique might be essential for clinically available LDCT.
One patient in the SDCT group was clinically proven as having a ureter stone, although it was documented as phlebolith in our study. This patient did not have ureteral dilatation and hydronephrosis. Although efforts to differentiate a ureter stone from a phlebolith have been made with the “tissue rim” or “comet tail” signs, the tissue rim sign has the disadvantage of size dependency. Smaller ureteral stones are more likely to exhibit a tissue rim sign than are larger calculi.1516 According to a study by Heneghan, et al.,17 the soft tissue rim sign was found to have a sensitivity of 77% and specificity of 92%. The comet tail sign has been found to have a sensitivity 21–65% and a specificity of 100%.1618 Their presence without ureteral dilatation needs to consider phlebolith, but it is occasionally observed adjacent to calculi.15 From our results, the difficulty of differentiating between ureteral stones and phlebolith is not only evident for LDCT but is also evident for SDCT, so it is very important that an experienced physician reviews the CT scan to overcome this problem.
In our study, unsuspected diseases beyond ureter stones were identified in one patient with acute diverticulitis in the SDCT group. The presence of an alternative diagnosis on standard high dose CT may be as high as 13%, and Poletti, et al.19 reposted the same detection rate of an alternative diagnosis in their series. In terms of an alternative diagnosis, our results are not conclusive. In general, young adults whose presentations mimic renal colic would rarely prove to have serious chronic or malignant disease. Reports indicate that it is feasible to considerably reduce the dose of CT radiation for the diagnosis of appendicitis or diverticulitis, which are important alternative diagnoses.820 For other alternative diagnoses, such as those of a complicated adnexal cyst, pelvic inflammatory disease, or acute pyelonephritis, CT examination may not be critical since the diagnosis in these cases should be based on clinical findings or other types of diagnostic tests.
Our study had a few limitations in that only limited numbers of patients were enrolled, even though the study used a prospective blinded technique. According to sample size calculation in this non-inferiority study, a total of 304 subjects, 152 persons per group, was required. However, it was difficult to recruit patients for our study because they were worried about additional imaging and misdiagnosis from LDCT. Compared with SDCT, LDCT-IR was not inferior in terms of the diagnosis of ureter stones, although these concerns and our study overcame the ethical problem of previous studies in which LDCT and SDCT were simultaneously performed in patients. Additionally, a potential limitation of LDCT is misdiagnosis as mentioned above. There may be other diseases that can cause colicky flank pain, such as ureteropelvic junction obstruction, acute pyelonephritis, urothelial carcinoma, or diseases of gastrointestinal or gynaecological organs, that can be exacerbated by low-dose CT. In the present study, one patient was diagnosed with acute appendicitis. It is clear that a close physical examination and careful inspection of clinical symptoms is necessary. Finally, this study was not designed to evaluate the interobserver variability or effect of having the studies read by urologists instead of radiologists. The reason for the design of this study was that the interobserver agreement was consistently excellent (0.907–1.000) when the analysis was categorized by the size and location of the ureter stones, which was shown in our previous study.10 The interpretation of LDCT-IR by urologists was reliable and not inferior to that by radiologists. Overall, our results indicate that LDCT-IR can be used instead of SDCT as the first-line imaging test because the ultimate clinical outcomes and diagnostic performance can be maintained if LDCT-IR is incorporated into the diagnostic process with selective additional imaging and clinical observation.
In this study, we observed that the use of LDCT-IR as a first-line imaging test was not inferior to SDCT with respect to the diagnosis of ureter stones and that it is clinically available for the evaluation of renal colic patients.
ACKNOWLEDGEMENTS
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology, Republic of Korea (2015R1A1A1A0500110) and (2017R1D1A1B03031514), and the Korea Health Technology R&D Project (HI17C0710).
References
1. Chi BH, Chang IH, Choi SY, Suh DC, Chang CW, Choi YJ, et al. Daily mean temperature and urolithiasis presentation in six cities in Korea: time-series analysis. J Korean Med Sci. 2017; 32:999–1008. PMID: 28480659.

2. Choi SY, Lee SY, Chi BH, Kim JW, Kim TH, Chang IH. Urbanization may affect the incidence of urolithiasis in South Korea. Springerplus. 2016; 5:1891. PMID: 27843748.

3. Chung JD, Kim TH, Myung SC, Moon YT, Kim KD, Chang IH. Influence of overweight on 24-hour urine chemistry studies and recurrent urolithiasis in children. Korean J Urol. 2012; 53:268–274. PMID: 22536471.

4. Kim SC, Moon YT, Hong YP, Hwang TK, Choi SH, Kim KJ, et al. Prevalence and risk factors of urinary stones in Koreans. J Korean Med Sci. 1998; 13:138–146. PMID: 9610613.

5. Boulay I, Holtz P, Foley WD, White B, Begun FP. Ureteral calculi: diagnostic efficacy of helical CT and implications for treatment of patients. AJR Am J Roentgenol. 1999; 172:1485–1490. PMID: 10350277.

6. Fulgham PF, Assimos DG, Pearle MS, Preminger GM. Clinical effectiveness protocols for imaging in the management of ureteral calculous disease: AUA technology assessment. J Urol. 2013; 189:1203–1213. PMID: 23085059.

7. Lee DH, Chang IH, Kim JW, Chi BH, Park SB. Usefulness of nonenhanced computed tomography for diagnosing urolithiasis without pyuria in the emergency department. Biomed Res Int. 2015; 2015:810971. PMID: 26421303.

8. Ahn S. LOCAT group. LOCAT (low-dose computed tomography for appendicitis trial) comparing clinical outcomes following low- vs standard-dose computed tomography as the first-line imaging test in adolescents and young adults with suspected acute appendicitis: study protocol for a randomized controlled trial. Trials. 2014; 15:28. PMID: 24438500.

9. Ibrahim M, Parmar H, Christodoulou E, Mukherji S. Raise the bar and lower the dose: current and future strategies for radiation dose reduction in head and neck imaging. AJNR Am J Neuroradiol. 2014; 35:619–624. PMID: 23449649.

10. Kwon JK, Chang IH, Moon YT, Lee JB, Park HJ, Park SB. Usefulness of low-dose nonenhanced computed tomography with iterative reconstruction for evaluation of urolithiasis: diagnostic performance and agreement between the urologist and the radiologist. Urology. 2015; 85:531–538. PMID: 25733262.

11. Choi SY, Ahn SH, Choi JD, Kim JH, Lee BI, Kim JI, et al. Determination of optimal imaging settings for urolithiasis CT using filtered back projection (FBP), statistical iterative reconstruction (IR) and knowledge-based iterative model reconstruction (IMR): a physical human phantom study. Br J Radiol. 2016; 89:20150527. PMID: 26577542.

12. Park SH, Kim KD, Moon YT, Myung SC, Kim TH, Chang IH, et al. Pilot study of low-dose nonenhanced computed tomography with iterative reconstruction for diagnosis of urinary stones. Korean J Urol. 2014; 55:581–586. PMID: 25237459.

13. Malkawi IM, Han E, Atalla CS, Santucci RA, O'Neil B, Wynberg JB. Low-dose (10%) computed tomography may be inferior to standard-dose CT in the evaluation of acute renal colic in the emergency room setting. J Endourol. 2016; 30:493–496. PMID: 26728321.

14. Park SB, Kim YS, Lee JB, Park HJ. Knowledge-based iterative model reconstruction (IMR) algorithm in ultralow-dose CT for evaluation of urolithiasis: evaluation of radiation dose reduction, image quality, and diagnostic performance. Abdom Imaging. 2015; 40:3137–3146. PMID: 26197735.

15. Guest AR, Cohan RH, Korobkin M, Platt JF, Bundschu CC, Francis IR, et al. Assessment of the clinical utility of the rim and comet-tail signs in differentiating ureteral stones from phleboliths. AJR Am J Roentgenol. 2001; 177:1285–1291. PMID: 11717067.

16. Bell TV, Fenlon HM, Davison BD, Ahari HK, Hussain S. Unenhanced helical CT criteria to differentiate distal ureteral calculi from pelvic phleboliths. Radiology. 1998; 207:363–367. PMID: 9577482.

17. Heneghan JP, Dalrymple NC, Verga M, Rosenfield AT, Smith RC. Soft-tissue “rim” sign in the diagnosis of ureteral calculi with use of unenhanced helical CT. Radiology. 1997; 202:709–711. PMID: 9051021.

18. Boridy IC, Nikolaidis P, Kawashima A, Goldman SM, Sandler CM. Ureterolithiasis: value of the tail sign in differentiating phleboliths from ureteral calculi at nonenhanced helical CT. Radiology. 1999; 211:619–621. PMID: 10352582.

19. Poletti PA, Platon A, Rutschmann OT, Schmidlin FR, Iselin CE, Becker CD. Low-dose versus standard-dose CT protocol in patients with clinically suspected renal colic. AJR Am J Roentgenol. 2007; 188:927–933. PMID: 17377025.

20. Tack D, Bohy P, Perlot I, De Maertelaer V, Alkeilani O, Sourtzis S, et al. Suspected acute colon diverticulitis: imaging with low-dose unenhanced multi-detector row CT. Radiology. 2005; 237:189–196. PMID: 16126929.

Fig. 1
Flow chart of the patient inclusion and review protocol. ED, emergency department; LDCT-IR, low-dose unenhanced computed tomography with iterative reconstruction technique; SDCT, standard-dose unenhanced computed tomography.
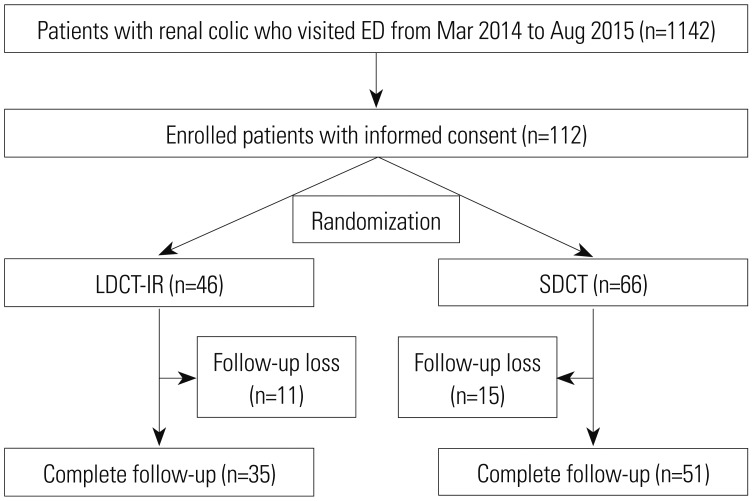
Fig. 2
A comparison between LDCT-IR and SDCT for a ureter stone. (A) LDCT-IR sets (axial, coronal, and sagittal images) of a 35-year-old man with a right lower ureteral stone (white arrows). The body mass index of the patient was 34.3 kg/m2, and the effective radiation dose was 3.384 mSv. (B) SDCT sets (axial, coronal, and sagittal images) of a 50-year-old woman with a left upper ureteral stone (white arrows). The body mase index of the patient was 20.8 kg/m2, and the effective radiation dose was 4.416 mSv. LDCT-IR, low-dose computed tomography with iterative reconstruction technique; SDCT, standard-dose unenhanced computed tomography.
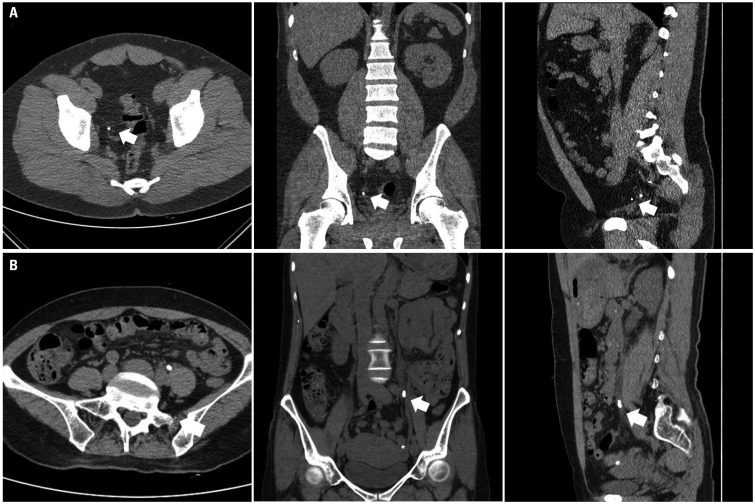
Fig. 3
LDCT-IR and SDCT for false negative findings for ureter stone and causes other than ureter stone. (A) LDCT-IR sets (axial, coronal, and sagittal images) of a 21-year-old man with a right mid ureteral stone (white arrows). The radiologist did not discriminate between a ureter stone and vascular calcification. (B) LDCT-IR sets (axial, coronal, and sagittal images) of a 40-year-old man with a left mid ureteral stone (white arrows). The radiologist discriminated it as a vascular calcification rather than as a ureter stone. (C) SDCT sets (axial, coronal, and sagittal images) of a 33-year-old woman with a left lower ureteral stone (white arrows). The radiologist discriminated the calcification because there was no ureteral dilatation and no ureteral course tracking. (D) SDCT sets (axial, coronal, and sagittal images) of a 40-year-old man who complained of left flank pain. The radiologist discriminated the several diverticula in D-colon with pericolic infiltration (white arrows) and no urinary stone. The final diagnosis of left flank pain was acute diverticulitis. LDCT-IR, low-dose computed tomography with iterative reconstruction technique; SDCT, standard-dose unenhanced computed tomography.
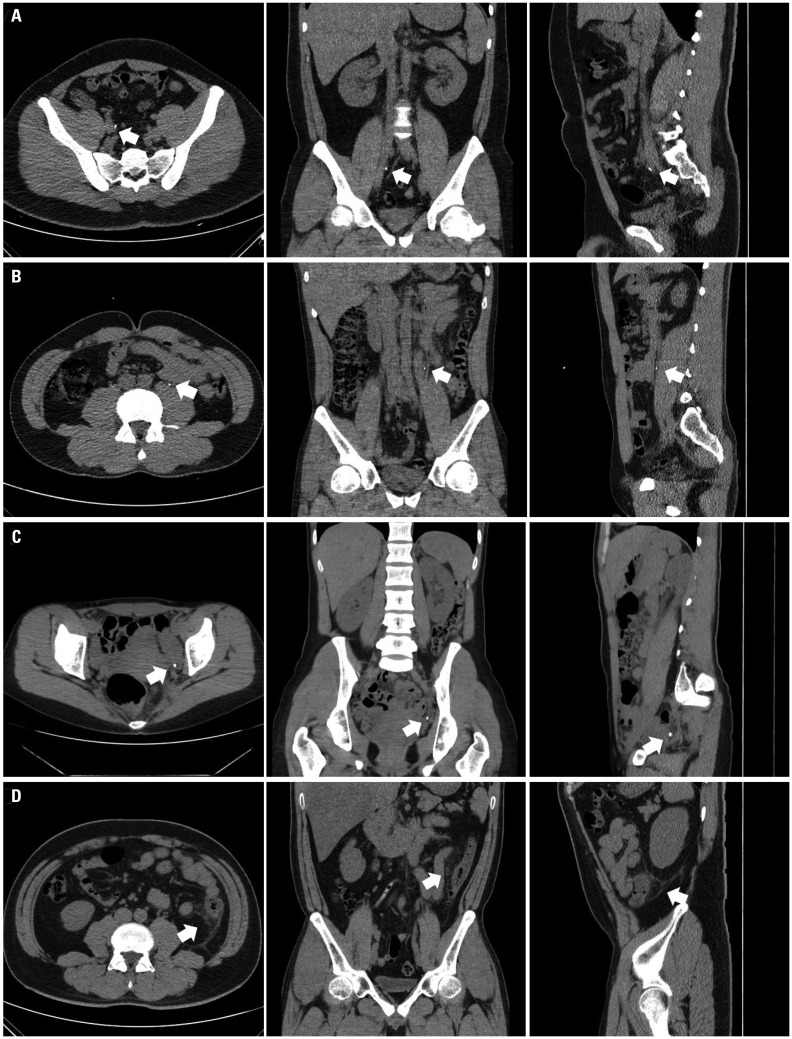
Table 1
A Summary of the Patient Demographics, Urine Test Results, and Characteristics of Urolithiasis
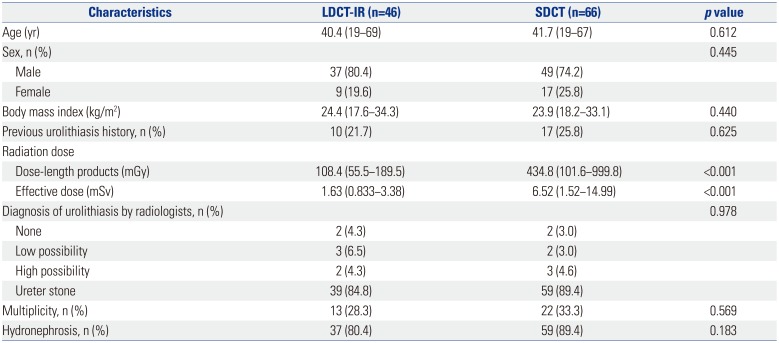
Table 2
A Summary of the Categorization Used in the Diagnosis and Management for LDCT-IR and SDCT
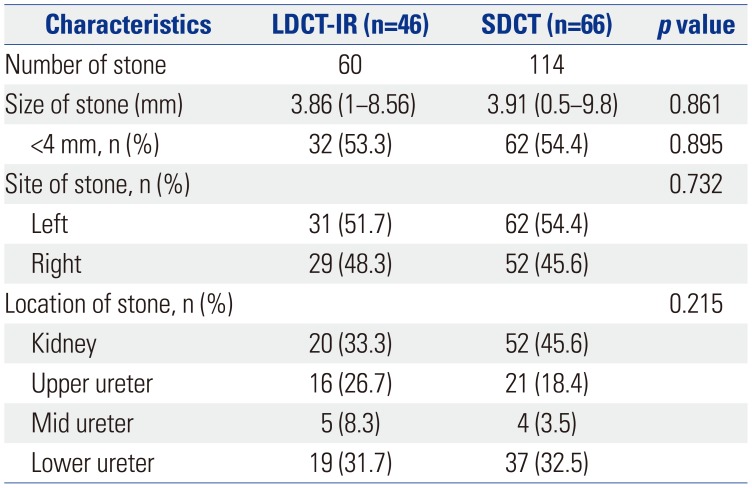
Table 3
The Diagnostic Performance and Diagnostic Confidence of the LDCT-IR and SDCT in Patients with Symptomatic Ureteral Stone according to the Clinical Follow-Up and Management




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download