This article has been
cited by other articles in ScienceCentral.
Abstract
Radiocontrast media-induced acute severe thrombocytopenia is a very rare complication and potentially life-threatening. Here, we report the case of a 63-year-old male patient with severe acute thrombocytopenia following first exposure to intravenous non-ionic contrast media without immediate allergic reactions. His platelet count dropped from 107000/µL to 2000/µL after six hours of radiocontrast infusion. After administration of corticosteroid and transfusion of platelet concentrates, the platelet count returned gradually to normal within 5 days. To the best of our knowledge, non-ionic contrast media-induced isolated acute severe thrombocytopenia following no signs or symptoms of immediate allergic reaction has never been described.
Go to :

Keywords: Thrombocytopenia, contrast media, non-ionic, hypersensitivity
INTRODUCTION
Contrast media can occasionally produce allergic reactions, ranging from minor to life-threatening anaphylactoid responses. Intravenous contrast media can also induce acute thrombocytopenia, although it is a very rare complication that has been mostly reported in patients who received ionic contrast media, which was usually used for coronary arteriography.
123 Non-ionic contrast-induced acute thrombocytopenia is far more rare and has been usually accompanied by signs or symptoms of immediate allergic reaction, including respiratory distress, chest discomfort, facial flushing, or skin rash.
45
Here, we report the case of a 63-year-old male patient with a self-limiting severe acute thrombocytopenia following first exposure to intravenous non-ionic contrast medium without any signs or symptoms of immediate allergic reactions.
Go to :

CASE REPORT
A 63-year-old male had visited an outside clinic with easy fatigue. Laboratory evaluation revealed elevation of liver transaminases with alanine aminotransaminase of 47 IU/L, aspartate aminotransferase of 106 IU/L, and gamma-glutamyl trans-peptidase of 935 IU/L. The patient had a history of chronic alcohol intake over 30 years and hypertension for 8 years. His daily medication consisted of felodipine 5 mg, losartan 50 mg, atorvastatin 20 mg, and aspirin 100 mg, and he denied any recent changes in medication.
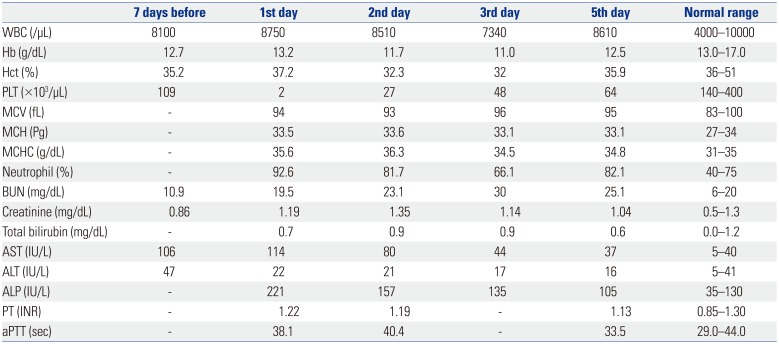
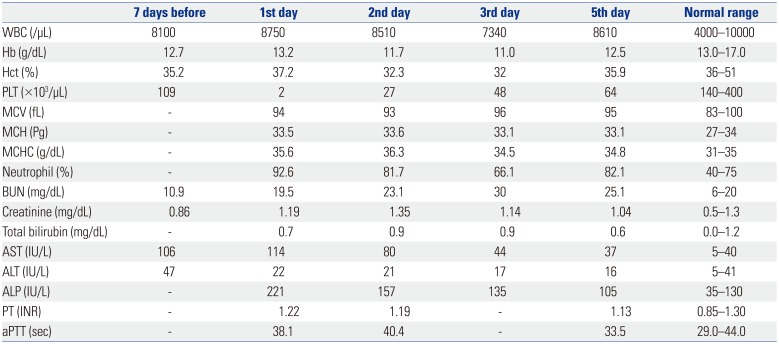
A non-ionic low osmolarity contrast agent [120 mL, Ioversol (Optiray 350©)] enhanced computed tomography (CT) scan was performed to clarify the cause of abnormal liver function test. During infusion of contrast media, no specific signs or symptoms were observed. CT scan detected chronic liver disease with mild splenomegaly, which was consistent with alcoholic liver disease. The patient returned home with no signs or symptoms of immediate allergic reactions. Six hours after examination, he was admitted to our emergency room (ER) reporting sudden onset bleeding from his intravenous site, along with a huge bruise and hematoma. At presentation to the ER, he had a blood pressure of 105/58 mm Hg, a heart rate of 71/min, and a respiration rate of 18/min. No fever, urticaria, itches, rash, respiratory distress, or chest discomfort was recorded. Laboratory test showed severe thrombocytopenia with a platelet count of 2000/µL, which was 107000/µL at the aforementioned clinic 7 days prior. Mild anemia and elevated liver transaminases were also reported, which were considered to be associated with chronic alcohol intake (
Table 1). Other laboratory parameters, including prothrombin time and activated partial thromboplastin time, were within normal limits. Peripheral blood smear showed normal size and shape of white blood and red blood cells, except a markedly decreased number of platelets. Serological studies showed no evidence of viral hepatitis or autoimmune disease, and there were no signs or symptoms of infectious disease.
Table 1
Results of Laboratory Evaluation before and after Development of Acute Thrombocytopenia
|
7 days before |
1st day |
2nd day |
3rd day |
5th day |
Normal range |
|
WBC (/µL) |
8100 |
8750 |
8510 |
7340 |
8610 |
4000–10000 |
|
Hb (g/dL) |
12.7 |
13.2 |
11.7 |
11.0 |
12.5 |
13.0–17.0 |
|
Hct (%) |
35.2 |
37.2 |
32.3 |
32 |
35.9 |
36–51 |
|
PLT (×103/µL) |
109 |
2 |
27 |
48 |
64 |
140–400 |
|
MCV (fL) |
- |
94 |
93 |
96 |
95 |
83–100 |
|
MCH (Pg) |
- |
33.5 |
33.6 |
33.1 |
33.1 |
27–34 |
|
MCHC (g/dL) |
- |
35.6 |
36.3 |
34.5 |
34.8 |
31–35 |
|
Neutrophil (%) |
- |
92.6 |
81.7 |
66.1 |
82.1 |
40–75 |
|
BUN (mg/dL) |
10.9 |
19.5 |
23.1 |
30 |
25.1 |
6–20 |
|
Creatinine (mg/dL) |
0.86 |
1.19 |
1.35 |
1.14 |
1.04 |
0.5–1.3 |
|
Total bilirubin (mg/dL) |
- |
0.7 |
0.9 |
0.9 |
0.6 |
0.0–1.2 |
|
AST (IU/L) |
106 |
114 |
80 |
44 |
37 |
5–40 |
|
ALT (IU/L) |
47 |
22 |
21 |
17 |
16 |
5–41 |
|
ALP (IU/L) |
- |
221 |
157 |
135 |
105 |
35–130 |
|
PT (INR) |
- |
1.22 |
1.19 |
- |
1.13 |
0.85–1.30 |
|
aPTT (sec) |
- |
38.1 |
40.4 |
- |
33.5 |
29.0–44.0 |

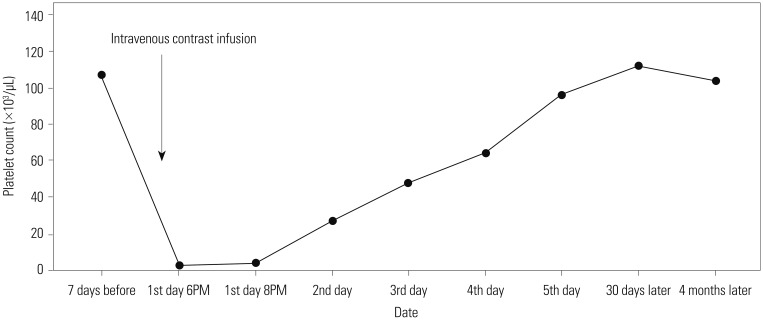
Since drug-induced thrombocytopenia was highly suspected, the patient received platelet concentrates (10 units) and methylprednisolone (1 mg/kg for 5 days) intravenously. The platelet count returned gradually to baseline by day 5, and no further exacerbation of thrombocytopenia was observed during follow-up (
Fig. 1). Liver transaminases were also recovered upon drinking cessation, and there were no significant changes in other laboratory tests. He was discharged on the fifth day.
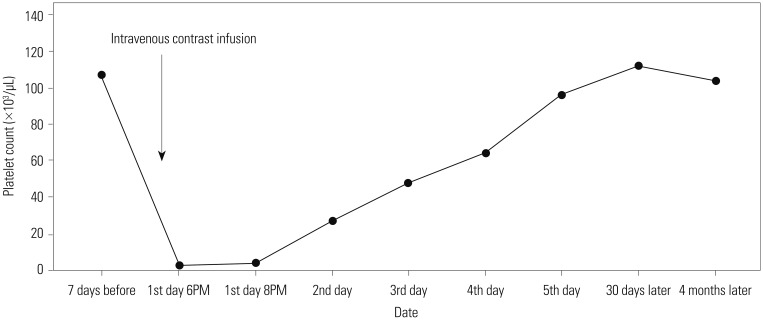 | Fig. 1Changes in platelet level before and after development of acute thrombocytopenia.
|
Go to :

DISCUSSION
Since their introduction in the 1920s, radiographic iodinated contrast media have been among the most commonly used drugs in modern medicine. The advent of low-osmolar iodinated contrast media has decreased the overall incidence of contrast-induced adverse events; the majority of adverse effects are mild and self-limited.
6 Nonetheless, severe or life-threatening complications, including cardiovascular collapse, bronchospasm, laryngeal edema, loss of consciousness, and seizure, can still occur occasionally. Acute severe thrombocytopenia induced by contrast media is extremely rare, with few cases reported in the literature. Most previous cases were associated with ionic contrast media used for coronary angiography.
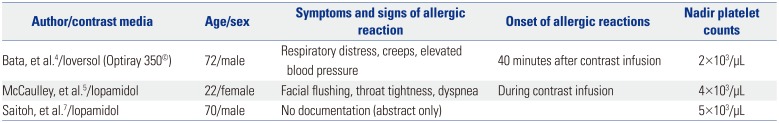
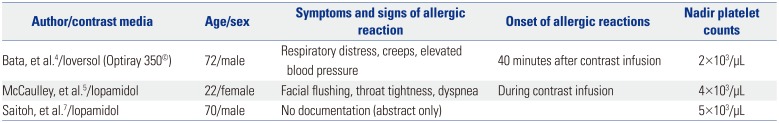
In our case, isolated acute severe thrombocytopenia was caused by non-ionic low osmolar contrast media without any signs or symptoms of immediate allergic reaction, which has never been described before. Three cases of non-ionic contrast-induced acute severe thrombocytopenia have been reported so far: Two cases demonstrated acute thrombocytopenia following symptoms of immediate allergic reaction after contrast infusion (
Table 2).
45 The other case did not describe whether any signs or symptoms of allergic reaction were observed after contrast infusion or not.
7
Table 2
Reported Cases of Non-Ionic Contrast Media-Induced Acute Thrombocytopenia
|
Author/contrast media |
Age/sex |
Symptoms and signs of allergic reaction |
Onset of allergic reactions |
Nadir platelet counts |
|
Bata, et al.4/Ioversol (Optiray 350©) |
72/male |
Respiratory distress, creeps, elevated blood pressure |
40 minutes after contrast infusion |
2×103/µL |
|
McCaulley, et al.5/Iopamidol |
22/female |
Facial flushing, throat tightness, dyspnea |
During contrast infusion |
4×103/µL |
|
Saitoh, et al.7/Iopamidol |
70/male |
No documentation (abstract only) |
|
5×103/μL |

Adverse reactions to contrast media are typically divided into two categories, chemotoxic reactions and hypersensitivity reactions.
89 Chemotoxic reactions are associated with the chemical properties of radiocontrast agent and dependent upon dose and infusion rate. These reactions, including emesis, flushing, warmth, increased vagal tone, and organ toxicities, are relatively common, usually transient, and self-limited. Hypersensitivity reactions are idiosyncratic and dose-independent, which include angioedema, bronchospasm, shock, and loss of consciousness. Several non-IgE mediated mechanisms have been proposed for hypersensitivity reactions.
1011 Drug-induced platelet destruction is usually caused by drug-induced antibodies; however, this can be difficult to prove.
12 Most instances of drug-induced thrombocytopenia are considered as idiosyncratic, and no predisposing genetic or environmental factors have been identified.
13 Although the mechanism of contrast-induced thrombocytopenia remains unclear, an immunological mechanism is also postulated. Furthermore, previous studies demonstrated that radiocontrast media could activate coagulation, kinin, and/or complement cascade,
101114 which might result in platelet aggregation with resultant thrombocytopenia. However,
in vitro studies evaluating the effects of contrast media on platelets have showed conflicting results.
1516 Further investigations are needed to clarify the pathophysiology of contrast-induced thrombocytopenia.
There is no established treatment for contrast-induced thrombocytopenia because of its rarity and uncertain pathophysiology. In many cases, patients have received treatment with high dose intravenous corticosteroids, which are widely used in management of anaphylaxis. However, the role of corticosteroids in contrast-induced thrombocytopenia has never been studied to date. In our opinion, corticosteroids may be beneficial in preventing or reducing the severity of possible delayed adverse effects of radiocontrast media. Intravenous immune globulin and plasma exchange have been used in management of drug-induced thrombocytopenia, although the benefit of these treatments is still uncertain.
The present case demonstrated a rare but severe hematologic adverse effect of non-ionic low osmolar contrast media. Contrast-induced acute severe thrombocytopenia can occur even in patients without no symptoms or signs of immediate allergic reactions. Given the wide-spread use of intravenous contrast media, this case reminds clinicians to be aware of a rare, but life-threatening, hematologic complication caused by contrast media.
Go to :

ACKNOWLEDGEMENTS
This study was supported by Inha University Hospital Research Grant.
Go to :

Notes
Go to :

References
1. Chang JC, Lee D, Gross HM. Acute thrombocytopenia after i.v. administration of a radiographic contrast medium. Am J Roentgenol. 1989; 152:947–949. PMID:
2705351.

2. Cubero-Gómez JM, Guerrero Márquez FJ, Diaz-de la-Llera L, Fernández-Quero M, Guisado-Rasco A, Villa-Gil-Ortega M. Severe thrombocytopenia induced by iodinated contrast after coronary angiography: The use of gadolinium contrast and intravascular ultrasound as an alternative to guide percutaneous coronary intervention. Rev Port Cardiol. 2017; 36:61.e1–61.e4. PMID:
27986390.

3. Wiemer M, Kreuzpaintner G, Lauer B, Kiefel V, Schultheiss HP, Horstkotte D, et al. [Recurrent immune thrombocytopenia: a rare complication after contrast medium injection]. Dtsch Med Wochenschr. 1995; 120:1236–1240. PMID:
7671781.
4. Bata P, Tarnoki AD, Tarnoki DL, Horvath E, Berczi V, Szalay F. Acute severe thrombocytopenia following non-ionic low-osmolarity intravenous contrast medium injection. Korean J Radiol. 2012; 13:505–509. PMID:
22778575.

5. McCaulley JA, Deering SH, Pates JA. Severe thrombocytopenia after contrast infusion in pregnancy. Obstet Gynecol. 2013; 121(2 Pt 2 Suppl 1):473–475. PMID:
23344413.
6. Hunt CH, Hartman RP, Hesley GK. Frequency and severity of adverse effects of iodinated and gadolinium contrast materials: retrospective review of 456,930 doses. Am J Roentgenol. 2009; 193:1124–1127. PMID:
19770337.

7. Saitoh T, Saiki M, Sawada U, Kawamura N, Tohno H, Horie T. [Severe thrombocytopenia induced by radiographic non-ionic contrast medium]. Rinsho Ketsueki. 2001; 42:507–511. PMID:
11505531.
8. Morcos SK, Thomsen HS. Adverse reactions to iodinated contrast media. Eur Radiol. 2001; 11:1267–1275. PMID:
11471623.

9. Brockow K, Ring J. Classification and pathophysiology of radiocontrast media hypersensitivity. Chem Immunol Allergy. 2010; 95:157–169. PMID:
20519888.

10. Szebeni J. Hypersensitivity reactions to radiocontrast media: the role of complement activation. Curr Allergy Asthma Rep. 2004; 4:25–30. PMID:
14680617.

11. Szebeni J. Complement activation-related pseudoallergy: a new class of drug-induced acute immune toxicity. Toxicology. 2005; 216:106–121. PMID:
16140450.

12. Aster RH, Curtis BR, McFarland JG, Bougie DW. Drug-induced immune thrombocytopenia: pathogenesis, diagnosis, and management. J Thromb Haemost. 2009; 7:911–918. PMID:
19344362.

13. Aster RH, Bougie DW. Drug-induced immune thrombocytopenia. N Engl J Med. 2007; 357:580–587. PMID:
17687133.

14. Simon RA, Schatz M, Stevenson DD, Curry N, Yamamoto F, Plow E, et al. Radiographic contrast media infusions. Measurement of histamine, complement, and fibrin split products and correlation with clinical parameters. J Allergy Clin Immunol. 1979; 63:281–288. PMID:
85650.
15. Li X, Gabriel DA. Differences between contrast media in the inhibition of platelet activation by specific platelet agonists. Acad Radiol. 1997; 4:108–114. PMID:
9061083.
16. Aspelin P, Stacul F, Thomsen HS, Morcos SK, van der. ESUR). Effects of iodinated contrast media on blood and endothelium. Eur Radiol. 2006; 16:1041–1049. PMID:
16395531.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download