Abstract
Purpose
Recurrent patellar dislocation is often associated with genu valgum. The purpose of this study was to analyze the short-term results of single-incision, closing-wedge distal femoral osteotomy (CWDFO) combined with medial reefing and lateral release for recurrent patellar instability with genu valgum.
Materials and Methods
Combined CWDFO/medial reefing/lateral release was performed on 10 knees. Clinical evaluation was based on pre- and postoperative Knee Society Score (KSS) and Kujala patellofemoral score. Radiographic evaluation was performed with reference to the weight-bearing line (WBL), the femorotibial angle (FTA), and the mechanical lateral distal femoral angles in the knee-standing view.
Results
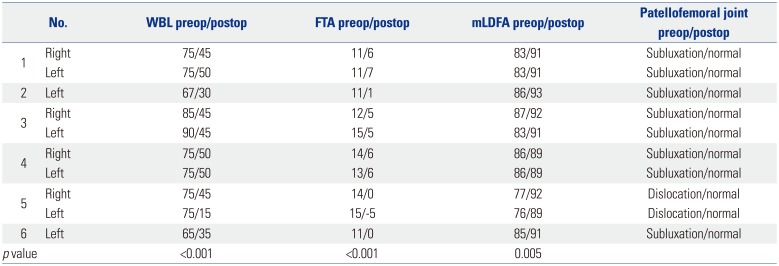
At a mean follow-up of 20±11.7 months (range, 12–42 months), KSS scores improved significantly, from 46.7±5.2 preoperatively to 87±4.4 postoperatively (p<0.001), as did the Kujala score, from 44±8 preoperatively to 86.6±6.8 postoperatively (p<0.001). The WBL decreased significantly, from 76±7% preoperatively to 41±11% postoperatively (p<0.001). The FTA was improved significantly, from 12.7±1.7° preoperatively to 4±4° postoperatively (p<0.001), as was the mLDFA, from 83±4° preoperatively to 91±1.3° postoperatively (p<0.001).
Patellar instability, seen frequently in adolescents and young adults, often is associated with previous knee injury.12 It is caused by various factors, including genu valgum, trochlea dysplasia, femoral intorsion, and patella alta.12 Whereas initial episodes of patellar dislocation typically are managed conservatively by immobilization and physiotherapy, chronic/recurrent dislocation and instability are treated primarily by surgery.3
The surgical treatment options include lateral release and medial plication,45 distal realignment procedures, such as tibial tubercle osteotomy,67 and procedures combining both proximal and distal realignment techniques.8 Distal femoral osteotomy (DFO), though most commonly advocated as a treatment option for lateral-compartment osteoarthritis,9 recently has been found to be effective for chronic patellar dislocation as well.10111213 DFO helps to correct excessive Q angle and genu valgum deformity, both of which are commonly associated with patellar instability.12 Furthermore, biplanar closing-wedge DFO (CWDFO) provides better stability and promotes bone healing, due to increased cancellous bone surface area at the osteotomy site.9101415 For these reasons, CWDFO could be a valuable procedure in a chronic patellar instability patient with excessive Q-angle stemming from significant genu valgum, Additional medial reefing with lateral release could be helpful when instability would be potentially intractable in the patient.1011121316
The purpose of this study was to analyze the short-term results of single-incision CWDFO combined with medial reefing and lateral release for recurrent patellar instability with genu valgum. We hypothesized that the technique would provide satisfactory clinical outcomes in patient with chronic patellar instability and significant genu valgum at a minimum follow-up of 1 year.
We reviewed the clinical and radiographic records of 10 knees in six patients (2 males, 4 females) undergoing CWDFO combined with medial reefing and arthroscopic lateral release for recurrent patellar instability between 2012 and 2015 with a minimum follow-up of 1 year. The patients' mean age at surgery was 26.5±6.4 years (range: 20–38 years). All of them had been operated on by one senior orthopaedic surgeon. The indication for surgical treatment was chronic patellar instability, either habitual or recurrent, combined with genu valgum deformity [criteria: exceeding 6–8° femorotibial angle (FTA) and 60% Mikulicz line; less than 86° mechanical lateral distal femoral angle (mLDFA) on anteroposterior (AP) long-leg weight-bearing lower-extremity scanograph].1718 The patients' demographic data are presented in Table 1.
All of the patients were assessed preoperatively and at final follow-up according to the Knee Society Score (KSS)19 and Kujala knee score.20 The radiographic evaluation included full-length, standing hip-to-ankle, knee AP, and lateral and patellar merchant radiographs. The position of the weight-bearing line (WBL), as well as the FTA and mLDFA, were measured on full-length, standing hip-to-ankle radiographs both pre- and postoperatively (at final follow-up).21 This study was approved by the Institutional Review Board (IRB) of Inje University Ilsan Paik Hospital.
Preoperative planning was performed using full-length, standing hip-to-ankle radiographs. PACS View (PACS; Marotech Inc., Seoul, Korea) was used for preoperative determination of the extent of correction. Our target line traveled 45% across the width of the plateau medially to laterally.
The patient was placed in a supine position on a radiolucent operating table, and a tourniquet was applied to the thigh. Initially, knee arthroscopy was performed in order to visually confirm patellar subluxation or dislocation from the superolateral portal view (Fig. 1A). Then, lateral release was performed, with the knee in full extension, from the superior to the inferior pole of the patella using electrocauterization. For DFO, a longitudinal skin incision was made beginning 10 cm above the patella and extending distally to the patellar apex. By a subvastus approach, the anteromedial aspect of the supracondylar area of the femur was then exposed. After incising the muscle fascia, the vastus medialis was stripped from the intermuscular septum and retracted using a Hohmann retractor.
The DFO was planned as a medial biplanar CWDFO on a plane beginning approximately 2 cm superior to the adductor tubercle in the medial supracondylar area and ending in the lateral supracondylar area. The starting point was marked under fluoroscopy on the medial supracondylar area by electrocauterization using a fixation plate as a reference. The target angle of correction was marked with two Kirschner wires under fluoroscopic guidance. The target point of the lateral cortex was above the lateral epicondyle (Fig. 1B). The axial part of the osteotomy involved the posterior two-thirds of the femur, and was performed up to 5 mm from the lateral femoral cortex in order to preserve it. Using a small oscillating saw, a medial-based wedge was created along the inner margins of the two Kirschner wires previously applied.
The direction of the frontal plane was marked by electrocauterization from the superior margin of the axial osteotomy to the anterior femoral cortex, and was angled approximately 110° from the axial osteotomy (Fig. 1C). The frontal-plane osteotomy was performed with an oscillating saw from the medial cortex and by cutting completely through the lateral cortex. The medial bone wedge was then removed, and the medial osteotomy was carefully closed by application of consistent pressure. The alignment of the axis of the leg was evaluated and confirmed by fluoroscopy. The osteotomy was stabilized using a TomoFix MDP plate (Synthes, West Chester, PA, USA). After fixation of the osteotomy, the medial retinaculum was carefully incised along the medial border of the patella, and approximately 1 cm was reefed. The medial structure, including the vastus medialis obliquus, medial capsule and medial retinaculum, were overlapped and tightened on the medial border of the patella using No. 2 Ethibond sutures (Ethicon Inc., Johnson & Johnson, Somerville, NJ, USA) with the knee at approximately 30° flexion (Fig. 1D). A final evaluation was performed to confirm the patellofemoral alignment through full range of motion.
For a period of 4 weeks, the patients walked with partial weight bearing. Range-of-motion exercises were initiated on postoperative day 3. Radiographs were obtained on postoperative day 7 to confirm the patellar femoral alignment and distal femur, and radiographs were reviewed after 4, and 8 weeks and 3, and 6 months in order to evaluate the healing of the osteotomy and the correction of the patellar instability (Fig. 2).
The assumption of the normal distribution of the variable was checked using the Kolmogorov-Smirnov test. The paired t-test was used to compare the preoperative and postoperative knee scores, WBL, FTA and mLDFA. SPSS software (version 18; SPSS Inc., Chicago, IL, USA) was used for the statistical analyses, with p<0.05 set as statistically significant.
At a mean follow-up of 20±11.7 months (range: 12–42 months), KSS improved markedly, from 46.7±5.2 preoperatively to 87±4.4 at final follow-up (p<0.001), and Kujala score was significantly improved as well, from 44±8 preoperatively to 86.6±6.8 at final follow-up (p<0.001) (Table 2).
The WBL decreased significantly, from 76±7% preoperatively to 41±11% postoperatively (p<0.001). Similarly, the FTA was improved significantly, from 12.7±1.7° preoperatively to 4±4° postoperatively (p<0.001), as was the mLDFA, from 83±4° preoperatively to 91±1.3° postoperatively (p<0.001) (Table 3).
On postoperative patellar merchant views, none of the knees showed patellar subluxation or dislocation. At final follow-up, all of the knees showed complete union at the osteotomy site. Two weeks postoperatively, one of the knees showed stiffness and limited flexion. This patient underwent additional manipulation under anesthesia. There was no infection, compartment syndrome, thrombosis, or non-union.
This paper describes the advantages of single-incision medial biplanar CWDFO combined with medial retinaculum reefing and lateral release for treatment of recurrent dislocation of the patella with genu valgus knee. Due to multiple complex contributing factors, recurrent dislocation of the patella is difficult to treat. The most common causes are reported to be disorders of the extensor mechanism such as soft-tissue restraints, patella alta, genu valgum, and malrotation of the lower extremity.45 The frequency of recurrent dislocation after acute patellar dislocation reportedly is 40–60% with conservative treatment and 10–30% with surgery.5
There are several techniques for treatment patellar dislocation, including proximal realignment, distal realignment, and combined proximal and distal realignment procedures; reports on CWDFO combined with proximal soft-tissue procedures for treatment of recurrent dislocation of the patella in valgus knee remain rare. DFO can be performed using an opening- or closing-wedge technique, though the former has been implicated in patellofemoral contact pressure increment, bone graft use, collapse, and delayed rehabilitation, due to breakage of the far cortex. For these reasons, opening-wedge DFO (OWDFO) is unsuitable for the purposes described in this paper.
The clinical results of isolated lateral release for patellar instability, meanwhile, reportedly are poor, and include ongoing instability and poor patient satisfaction, among other issues.7 Medial reefing procedures for patellar instability frequently are performed (and typically in conjunction with lateral release) to achieve proximal realignment. However, most of the relevant reports are not relevant to valgus knee. Medial patellofemoral ligament reconstruction, an effective surgical procedure, requires a soft-tissue procedure (either autograft or allograft). Still, most reports, again, are not relevant to valgus knees.
This paper presents cases of patients with recurrent patellar dislocation in a valgus knee. Regardless of trauma, all of the patients had valgus knee and more than one experience of patellar dislocation. It has been reported that proximal alignment should be performed when the tibial tubercle-trochlear groove (TTTG) distance is normal, whereas distal alignment combined with proximal alignment is preferable in cases where the TTTG distance is more than 20 mm.22 There have been several reports of the treatment of patellar dislocation with genu valgum. Purushothaman, et al.13 described posttraumatic chronic patellar dislocation using OWDFO and medial patellofemoral ligament reconstruction. Shen, et al.8 reported a procedure combining proximal soft-tissue, DFO, and distal tibial tuberosity realignment for treatment of genu valgum. Kwon, et al.12 reported a case of habitual patellar dislocation treated by CWDFO with medial reefing and lateral retinacular release. Kwak, et al.11 reported a case of habitual patellar dislocation treated by OWDFO with medial reefing in a patient with hypoplasia of the lateral femoral condyle. Hinterwimmer, et al.10 reported a method of biplanar lateral OWDFO for patellofemoral malalignment.
There are several advantages to the new combined technique for the treatment of recurrent patellar dislocation with genu valgus knee. First, varus osteotomy can contribute to decreased risk of re-dislocation of the aligned patella, specifically by reducing the strong lateral vector applied to the patellar cause of the genu valgus.13 By correction of the valgus moment of the femur, the patellofemoral joint can be better stabilized. Second, medial CWDFO combined with medial retinaculum reefing can be performed via a single incision, which is more cosmetic than lateral OWDFO with medial reefing, which entails two incisions. Third, medial CWDFO offers an early-rehabilitation advantage over lateral OWDFO, due to its direct bone-to-bone contact. Additionally, biplanar CWDFO has been shown to improve the primary stability of the osteotomy and bone contact surface area, which can promote more rapid bone healing than is possible in the case of uniplanar CWDFO.11
The disadvantages of this technique, which include the risks of non-union and patellar re-dislocation, are of concern. No such complications, however, were observed in our study. In any event, the new technique requires further clinical study of primary cases with longer follow-up periods.
In conclusion, use of single-incision CWDFO combined with medial reefing and lateral release prevents patellar dislocation, corrects deformity, and improves clinical outcomes.
References
1. Ries Z, Bollier M. Patellofemoral instability in active adolescents. J Knee Surg. 2015; 28:265–277. PMID: 25892009.

2. Waterman BR, Belmont PJ Jr, Owens BD. Patellar dislocation in the United States: role of sex, age, race, and athletic participation. J Knee Surg. 2012; 25:51–57. PMID: 22624248.

3. Smith TO, Song F, Donell ST, Hing CB. Operative versus non-operative management of patellar dislocation. A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011; 19:988–998. PMID: 21234544.

4. Lee JJ, Lee SJ, Won YG, Choi CH. Lateral release and medial plication for recurrent patella dislocation. Knee Surg Sports Traumatol Arthrosc. 2012; 20:2438–2444. PMID: 22426853.

5. Ricchetti ET, Mehta S, Sennett BJ, Huffman GR. Comparison of lateral release versus lateral release with medial soft-tissue realignment for the treatment of recurrent patellar instability: a systematic review. Arthroscopy. 2007; 23:463–468. PMID: 17478275.

6. Drexler M, Dwyer T, Dolkart O, Goldstein Y, Steinberg EL, Chakravertty R, et al. Tibial rotational osteotomy and distal tuberosity transfer for patella subluxation secondary to excessive external tibial torsion: surgical technique and clinical outcome. Knee Surg Sports Traumatol Arthrosc. 2014; 22:2682–2689. PMID: 23740327.

7. Hall MJ, Mandalia VI. Tibial tubercle osteotomy for patello-femoral joint disorders. Knee Surg Sports Traumatol Arthrosc. 2016; 24:855–861. PMID: 25326765.

8. Shen HC, Chao KH, Huang GS, Pan RY, Lee CH. Combined proximal and distal realignment procedures to treat the habitual dislocation of the patella in adults. Am J Sports Med. 2007; 35:2101–2108. PMID: 17724090.

9. Brinkman JM, Freiling D, Lobenhoffer P, Staubli AE, van Heerwaarden RJ. Supracondylar femur osteotomies around the knee: patient selection, planning, operative techniques, stability of fixation, and bone healing. Orthopade. 2014; 43(Suppl 1):S1–S10. PMID: 25331499.
10. Hinterwimmer S, Minzlaff P, Saier T, Niemeyer P, Imhoff AB, Feucht MJ. Biplanar supracondylar femoral derotation osteotomy for patellofemoral malalignment: the anterior closed-wedge technique. Knee Surg Sports Traumatol Arthrosc. 2014; 22:2518–2521. PMID: 24748287.

11. Kwak JH, Sim JA, Kim NK, Lee BK. Surgical treatment of habitual patella dislocation with genu valgum. Knee Surg Relat Res. 2011; 23:177–179. PMID: 22570831.

12. Kwon JH, Kim JI, Seo DH, Kang KW, Nam JH, Nha KW. Patellar dislocation with genu valgum treated by DFO. Orthopedics. 2013; 36:840–843. PMID: 23746026.

13. Purushothaman B, Agarwal A, Dawson M. Posttraumatic chronic patellar dislocation treated by distal femoral osteotomy and medial patellofemoral ligament reconstruction. Orthopedics. 2012; 35:e1668–e1672. PMID: 23127463.

14. Brinkman JM, Hurschler C, Staubli AE, van Heerwaarden RJ. Axial and torsional stability of an improved single-plane and a new biplane osteotomy technique for supracondylar femur osteotomies. Knee Surg Sports Traumatol Arthrosc. 2011; 19:1090–1098. PMID: 21161172.

15. van Heerwaarden R, Najfeld M, Brinkman M, Seil R, Madry H, Pape D. Wedge volume and osteotomy surface depend on surgical technique for distal femoral osteotomy. Knee Surg Sports Traumatol Arthrosc. 2013; 21:206–212. PMID: 22766687.

16. Iliadis AD, Jaiswal PK, Khan W, Johnstone D. The operative management of patella malalignment. Open Orthop J. 2012; 6:327–339. PMID: 22927893.

17. Forkel P, Achtnich A, Metzlaff S, Zantop T, Petersen W. Midterm results following medial closed wedge distal femoral osteotomy stabilized with a locking internal fixation device. Knee Surg Sports Traumatol Arthrosc. 2015; 23:2061–2067. PMID: 24676790.

18. Haviv B, Bronak S, Thein R, Thein R. The results of corrective osteotomy for valgus arthritic knees. Knee Surg Sports Traumatol Arthrosc. 2013; 21:49–56. PMID: 22940779.

19. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989; (248):13–14. PMID: 2805470.

20. Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Neli-markka O. Scoring of patellofemoral disorders. Arthroscopy. 1993; 9:159–163. PMID: 8461073.

22. Sherman SL, Erickson BJ, Cvetanovich GL, Chalmers PN, Farr J 2nd, Bach BR Jr, et al. Tibial tuberosity osteotomy: indications, techniques, and outcomes. Am J Sports Med. 2014; 42:2006–2017. PMID: 24197613.
Fig. 1
(A) Biplane distal femur osteotomy and medial reefing procedure arthroscopic superiorlateral view-subluxed patellar target point is above the lateral epicondyle of distal femur biplane osteotomy lateral release and medial reefing. (B) Biplane distal femur osteotomy and medial reefing procedure arthroscopic superiorlateral view-subluxed patellar target point is above the lateral epicondyle of distal femur biplane osteotomy lateral release and medial reefing. (C) Biplane distal femur osteotomy and medial reefing procedure arthroscopic superiorlateral view-subluxed patellar target point is above the lateral epicondyle of distal femur biplane osteotomy lateral release and medial reefing. (D) Biplane distal femur osteotomy and medial reefing procedure arthroscopic superiorlateral view-subluxed patellar target point is above the lateral epicondyle of distal femur biplane osteotomy lateral release and medial reefing.
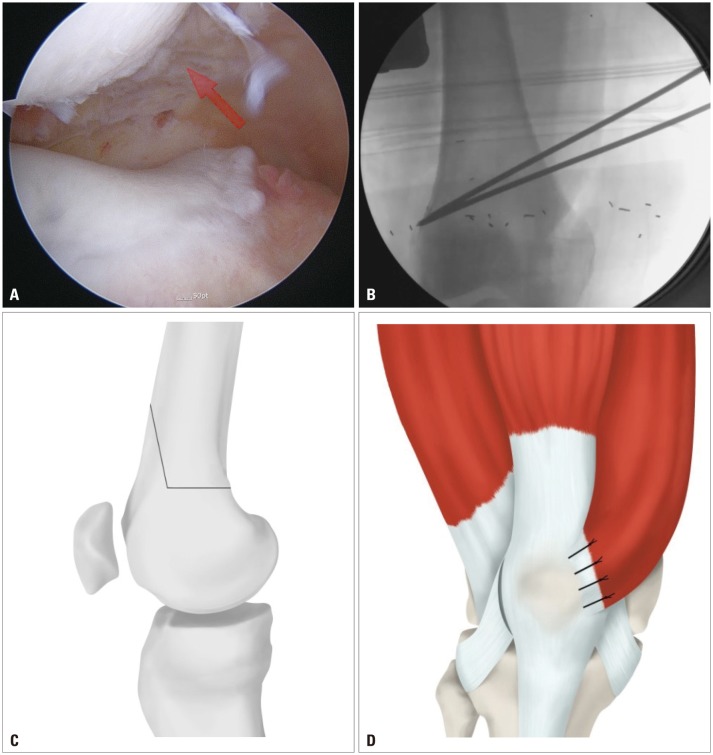
Fig. 2
(A-a) Preoperative standing, full length, hip-to-ankle radiograph of a 21-year-old male patient showing bilateral genu valgus deformity as shown by the weight bearing lines (green line) and subluxation of patellar both. (A-b) Postoperative standing, full length, hip-to-ankle radiograph of the same patient at 1-year follow-up showing significant change in the weight bearing lines after a combined medial closed-wedge distal femoral osteotomy and lateral release with medial reefing and normal alignment of patellofemoral joint. (B-a) Preoperative standing, full length, hip-to-ankle radiograph of a 21-year-old male patient showing bilateral genu valgus deformity as shown by the weight bearing lines (green line) and subluxation of patellar both. (B-b) Postoperative standing, full length, hip-to-ankle radiograph of the same patient at 1-year follow-up showing significant change in the weight bearing lines after a combined medial closed-wedge distal femoral osteotomy and lateral release with medial reefing and normal alignment of patellofemoral joint.
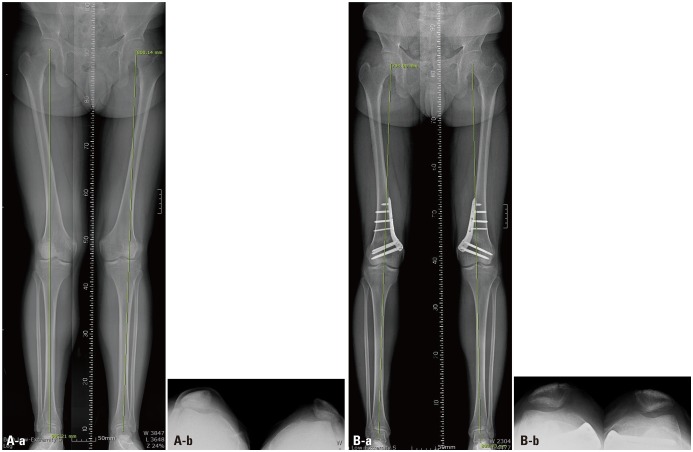
Table 1
Demographic Data on Patients
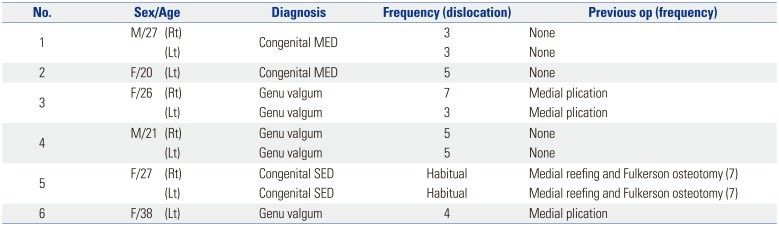
Table 2
Preoperative and One-Year Follow-Up Clinical Outcomes for Patients
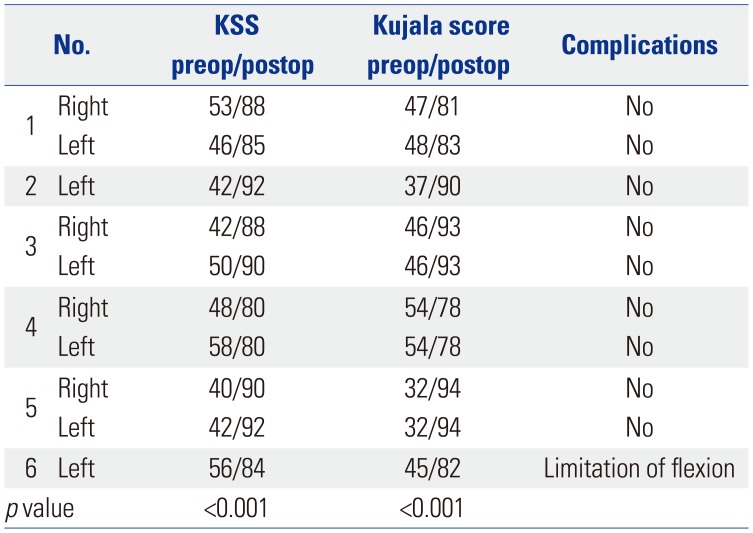
Table 3
Preoperative and One-Year Follow-Up Radiologic Parameters




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download