Abstract
Purpose
To evaluate the time to bone union after open reduction and internal fixation with cerclage cables followed by intramedullary nailing (IMN) for unstable humeral shaft fractures.
Materials and Methods
Patients with a humeral shaft fracture treated by IMN were enrolled. One group of patients was treated via open reduction and internal fixation with cables followed by IMN (cable group; n=32), while the other group was treated with a conventional closed IMN (non-cable group; n=64). The length of time to bone union and functional scores [Disabilities of the Arm, Shoulder and Hand (DASH) and University of California, Los Angeles (UCLA) scores] were measured for all patients.
Results
No significant differences were found in terms of age, gender, injury type, or smoking history between the two groups, except for the type of fracture. The cable group had significantly more complex types of fracture than the non-cable group (p<0.001). The mean time to bone union was 3.9 months in the cable group, while in the non-cable group, it was 4.4 months (p=0.041). The incidence of postoperative complications, such as non-union, delayed union, and radial nerve palsy, was similar between the two groups (p>0.05). No differences were identified in terms of DASH and UCLA scores (28.8 and 32.1 in the cable group and 26.4 and 32.6 in the non-cable group, respectively; p=0.335 and 0.264).
Most humeral shaft fractures can be treated using the functional bracing method.1 Surgery is considered when this conservative treatment fails to maintain the stability of reduction, open fracture, or other combined injuries. Many surgical techniques have been introduced to correct humeral shaft fractures, and there have been debates regarding their clinical indications.2 One of the standard surgical treatments is closed reduction and internal fixation using antegrade intramedullary nails. This technique has several potential advantages over other methods, including open reduction and internal fixation with plates, in terms of reduced disruption to the surrounding soft tissue and greater preservation of extramedullary vascularity around the fracture site.23 However, it can be difficult to perform a closed reduction or obtain the required stability from fixation with an intramedullary nail in highly unstable fractures of the humeral shaft in which there are complex or severely-displaced fragments, and such difficulties could result in delayed union or non-union of the bone fragments.4 Manipulation during cl-osed reduction can lead to the development of iatrogenic radial nerve palsy, since the lateral intermuscular septum fixes the radial nerve in fractures of the distal humerus.5 Therefore, in unstable humeral fractures, we have performed open reduction and internal fixation using one or two cerclage cables followed by an intramedullary nail to gain greater stability. Cerclage cables have been commonly used to fix periprosthetic fractures following total knee or hip arthroplasties at the femur or tibia, since they are particularly useful in the long bones that are occupied with the intramedullary stem.678 In addition, cerclage cables are used for subtrochanteric femur fractures treated with intramedullary nails and have provided satisfactory clinical results.9 There may be concern about delaying the bone union or increasing nonunion caused by cerclage cables in humeral shaft fracture, for the cables have been shown to affect periosteal circulation in a cadaveric study.10
To the best of our knowledge, there has been no previous study evaluating the clinical results of the open cerclage cable technique followed by intramedullary nailing (IMN) in humeral shaft fractures. Therefore, the purpose of this study was to compare the clinical results between two surgical techniques in humeral shaft fractures: the open cerclage cable technique followed by IMN and the conventional closed nailing technique. Our hypothesis was that one or two cerclage cables applied after open reduction would not delay bone union in patients with an unstable humeral shaft fracture treated with antegrade intramedullary nails, compared to the closed nailing technique. Moreover, this technique could provide similar functional results and postoperative complications to the closed nailing technique.
We examined the medical records of 232 patients who had undergone surgery for humeral diaphyseal fractures from January 2001 to January 2014. Patients who had received internal fixation with an antegrade intramedullary nail were included in this study. All patients were aged 18 years or older. The exclusion criteria included an open or pathologic fracture, treatment by a plate or bone graft, revision surgery or surgery combined with preoperative nerve palsy, and an ipsilateral fracture in the upper extremities. Patients who were lost to follow-up within 1 year of surgery or who died as a result of combined injuries prior to documentation of fracture union were also excluded. After applying these criteria, a total of 96 patients were included in the study and were divided into two groups. One group had surgery with open reduction and internal fixation using one or two cerclage cables combined with an antegrade intramedullary nail (cable group; n=32), while the second group was treated with the conventional technique of closed reduction and internal fixation with an intramedullary nail (non-cable group; n=64).
Background data were recorded for each of the enrolled patients, including age, gender, injury type (such as high or low energy), smoking history, and fracture type. Fracture types were classified using the Orthopaedic Trauma Association/AO Foundation (OTA/AO) 12-diaphyseal humerus classification.11
This study was conducted at a university-based, level 1 trauma center. All operations were performed by a single senior surgeon with more than 15 years of experience in orthopedic surgery. Reduction was attempted under general anesthesia using manual traction. If this was easily performed, the conventional closed nailing technique followed by postoperative rehabilitation, as described in Chapman, et al.,12 was used. However, if closed reduction failed or the reduced humerus was too unstable to maintain the reduced status, open reduction was selected instead. This usually happened in OTA/AO A1, B1, or C type fractures. The location and length of incision required for reduction of the fracture was confirmed using an image intensifier. A skin incision was created along the anterolateral aspect of the arm, and the length of the incision was within half the length of the fracture extent, approximately 4–5 cm long. The brachialis muscle was split longitudinally, while injury to the periosteum was kept to a minimum. Incarcerated soft tissue and hematoma were removed to clear the surgical field and create an anatomical reduction. To maintain the anatomical reduction by forceps or clamps, one cerclage cable (Cable-ready, Zimmer, Warsaw, IN, USA) was applied. The tip of the cable passer (Zimmer) was kept in contact with the cortex so as not to jam the radial nerve or muscles between the cable and the humerus. Cable passers with a varying radius simplified this procedure. Considering the anatomic position of the radial nerve, passing the tip of the passer from posterior to medial was preferred. The regulation tension of the cerclage cable, with a diameter of 1.8 mm, was set to 70 lb. If the reduced fragments were still unstable, an additional cable was added in the same manner. All cases were stabilized by an AO unreamed humeral nail (Synthes, Oberdorf, Switzerland) with an appropriate length and a diameter of 6.7 or 7.5 mm.
Radiographs, function [indexed by scores on the Disabilities of the Arm, Shoulder and Hand (DASH)13 and the University of California, Los Angeles (UCLA)14], and postoperative complications, such as non-union, delayed union, and radial nerve palsy or infection, were evaluated during every visit to the outpatient clinic at 1, 2, 3, 4, 6, and 12 months after surgery. The mean duration of the follow-up was 32.2 months in the cable group and 29.6 months in the non-cable group. Radiographic interpretation was conducted by a single orthopedic surgeon blinded to patient information. Bone union was determined as cortical continuity and obliteration of the fracture line. Non-union was defined as a fracture that showed absence of bone union for at least 6 months. This study was approved by the Ethics Committee at our university.
To compare the two groups, we used a Mann-Whitney U-test for continuous variables and Fisher's exact tests for categorical variables. Statistical significance was considered for p<0.05. SPSS software for Windows (ver. 12.0.1; SPSS, Inc., Chicago, IL, USA) was used for the statistical analysis.
The patients' demographic data are provided in Table 1. No significant differences in terms of age, gender, injury type, or smoking history were found between the groups, except for the type of fracture. The cable group had significantly more complex fracture types than the non-cable group: 69% of the cases in the cable group were classed as type 12B, while 72% of cases in the non-cable group were classed as type 12A (p<0.001).
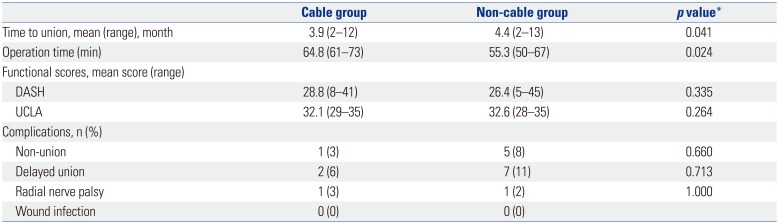
The length of time to bone union was shorter in the cable group (mean, 3.9 months) than the non-cable group (mean, 4.4 months); this difference was found to be statistically significant (p=0.041) (Fig. 1). At the final follow-up, the mean DASH scores for disabilities were 28.8 in the cable group and 26.4 in the non-cable group (p=0.335). The UCLA scores for shoulder function in the two groups were 32.1 and 32.6, respectively (p=0.264).
In terms of postoperative complications, non-union was identified in one case in the cable group and in five cases in the non-cable group (p=0.660). Three of the cases from the non-cable group underwent re-operation by augmented fixation with a locking compression plate (LCP), while the remainder underwent an auto iliac bone graft and augmented LCP. The incidence of radial nerve palsy was found to be comparable between the two groups. In both groups, each case of radial nerve injury had fully improved within 6 months after surgery (Table 2).
Cerclage cables have been regularly used in the lower extremities for periprosthetic fractures following arthroplasty and have provided satisfactory clinical results.815 However, few studies have investigated the use of cables in the upper extremities. A case of a periprosthetic fracture after shoulder arthroplasty was reported in which a plate/cable system for the humeral shaft was used.16 One study reported that, of 125 cases with a humeral shaft fracture, 20% of patients with an extended oblique or spiral type of fracture were fixed with cerclage wiring followed by IMN; however, no subgroup results were reported.2
We compared the clinical results of the open cerclage cable technique followed by nailing to the traditional closed nailing technique in humeral shaft fractures. As indicated by our results, the cable group, which had a greater number of patients with complex types of fracture, had a greater tendency for bone union to occur over a shorter time than the non-cable group. Other clinical results, such as functional score and the incidence of postoperative complications, such as non-union, delayed union, radial nerve palsy, and infection, were found to be similar between the two groups. Therefore, we deemed the open cerclage cable technique followed by nailing to be an effective and safe treatment for fractures of the humeral shaft.
The time taken for bone union to occur in a humeral shaft fracture is reported to be approximately 4 months and the rate of non-union is 4–13%.41718 Although open reduction and internal fixation with cerclage cables followed by IMN could have advantages over the conventional closed nailing technique, such as easier and more anatomic reduction and stability, there remains the concern of whether the technique can delay the time required for bone union to take place or increase the rate of non-union by decreasing the periosteal blood circulation. There have been several reports in the literature that have supported the concept that the humeral shaft has sufficiently strong circulation to allow healing of the fracture while remaining resistant to surgical dissection around the fracture site. In a randomized study, both the conventional open plating technique and minimal invasive plate osteosynthesis (MIPO) showed no significant difference in the time taken for bone union to occur in humeral shaft fractures (15.8 and 14.6 weeks, respectively).19 Additionally, another randomized study reported that the closed IMN and dynamic compression plating techniques result in comparable bone union in such fractures.17 A cadaver study concluded that a small number of cerclage cables had a minimal effect on the periosteal blood supplying the femur as long as they were not vigorously applied.20 Therefore, our hypothesis was that additional fixation with one or two cerclage cables after open reduction for complex types of fracture might be reasonable, even though it may also affect periosteal circulation in the humerus. In the current study, the mean length of time to bone union in the cable group was 3.9 months, which was shorter than that in the non-cable group, even though the cable group included much more complex types of fractures. Therefore, the open cerclage cable technique may not affect the rate of bone union adversely.
Radial nerve palsy probably occurs as a result of excessive traction or manipulation and interposition of the nerve at the fracture site.21 Most occurrences of radial nerve palsy following treatment for humeral shaft fracture are transient and do not require further intervention, as long as the nerve is not interposed at the fracture site.22 If radial nerve palsy does develop in a case of distal humeral fracture following conventional closed IMN, it could be difficult to determine its cause (i.e., neuropraxia from excessive manipulation or interposition of the nerve at the bone fragments). Therefore, open reduction during IMN in the distal humeral fracture can provide other advantages, such as the intraoperative inspection of the interposition of the nerve at the fragments. Jamming of the radial nerve between the cable and humeral cortex can be prevented if the cable passer is in touch with the cortex, as mentioned in the surgical technique.
In patients who have undergone open reduction and additional fixation with cerclage cables, the muscles in the arm, particularly the brachialis, may experience increased injury, compared with the closed nailing technique. However, DASH scores, reflecting the level of disability in the arm, were similar between the two groups. Other studies have reported excellent functional scores after the union of humeral shaft fractures with treatment techniques, such as conventional plating or MIPO, which suggests that the muscles in the humerus recover well without any functional deficits.
Open reduction and fixation with cerclage cables prior to IMN may lead to even more advantages. The radiation exposure time during the operation can be decreased compared to the conventional nailing technique. Although the exposure time has not been investigated in the present study, the open reduction method can decrease the level of radiation exposure, compared to closed reduction.19
Our study had some limitations. First, it was a comparative study, but not of a randomized design. The open cerclage cable technique can be used only for cases where closed reduction is difficult or where the fracture is highly unstable even after closed reduction has taken place, which may complicate a randomized comparative study. Second, the cable and non-cable groups included different types of fractures. However, this was inevitable because the more complex the fracture, the greater the need for additional fixation with cerclage cables via open reduction. Markedly comminuted fracture with multiple small fragments may not be a good indication for the open nailing technique as it is difficult to stabilize the fracture site using cerclage cables. In the future, if there were a larger number of patients, it would be possible to analyze them according to fracture subtype, such as 12A, 12B, and 12C, etc. Third, the open cable technique should be performed carefully not to hurt the radial nerve.
In conclusion, we have shown that additional fixation with one or two cerclage cables following open reduction may not delay the time taken for bone union to occur or increase the rate of postoperative complications, such as radial nerve palsy, compared with the conventional closed nailing technique. Therefore, in humeral fractures that are highly unstable or would be difficult to reduce in a closed manner, open reduction and internal fixation with one or two cerclage cables followed by IMN may be a safe and effective option.
References
1. Bhandari M, Devereaux PJ, McKee MD, Schemitsch EH. Compression plating versus intramedullary nailing of humeral shaft fractures--a meta-analysis. Acta Orthop. 2006; 77:279–284. PMID: 16752291.

2. Metsemakers WJ, Wijnen V, Sermon A, Vanderschot P, Nijs S. Intramedullary nailing of humeral shaft fractures: failure analysis of a single centre series. Arch Orthop Trauma Surg. 2015; 135:1391–1399. PMID: 26254579.

3. Chen F, Wang Z, Bhattacharyya T. Outcomes of nails versus plates for humeral shaft fractures: a Medicare cohort study. J Orthop Trauma. 2013; 27:68–72. PMID: 23343827.
4. Atalar AC, Kocaoglu M, Demirhan M, Bilsel K, Eralp L. Comparison of three different treatment modalities in the management of humeral shaft nonunions (plates, unilateral, and circular external fixators). J Orthop Trauma. 2008; 22:248–257. PMID: 18404034.

5. Whitson RO. Relation of the radial nerve to the shaft of the humerus. J Bone Joint Surg Am. 1954; 36-A:85–88. PMID: 13130592.

6. Sandhu R, Avramidis K, Johnson-Nurse C. Dall-Miles cable and plate fixation system in the treatment of periprosthetic femoral fractures: a review of 20 cases. J Orthop Surg (Hong Kong). 2005; 13:259–266. PMID: 16365489.

7. Huang MT, Lin CJ. Percutaneous cerclage wiring-assisted interlocking nailing for torsional tibia fractures: a modification with improved safety and simplicity. J Trauma. 2011; 71:1054–1058. PMID: 21986745.
8. Howell JR, Masri BA, Garbuz DS, Greidanus NV, Duncan CP. Cable plates and onlay allografts in periprosthetic femoral fractures after hip replacement: laboratory and clinical observations. Instr Course Lect. 2004; 53:99–110. PMID: 15116604.
9. Cebesoy O, Subasi M, Isik M. Cerclage cable in fracture: frustration or necessity? Int Orthop. 2011; 35:783–784. PMID: 21384149.

10. Apivatthakakul T, Phaliphot J, Leuvitoonvechkit S. Percutaneous cerclage wiring, does it disrupt femoral blood supply? A cadaveric injection study. Injury. 2013; 44:168–174. PMID: 23164676.

11. Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007; 21(10 Suppl):S1–S133. PMID: 18277234.
12. Chapman JR, Henley MB, Agel J, Benca PJ. Randomized prospective study of humeral shaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma. 2000; 14:162–166. PMID: 10791665.

13. Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001; 14:128–146. PMID: 11382253.
14. Amstutz HC, Sew Hoy AL, Clarke IC. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981; (155):7–20.
15. Ritter MA, Lutgring JD, Davis KE, Berend ME, Meding JB. A clinical, radiographic, and cost comparison of cerclage techniques: wires vs cables. J Arthroplasty. 2006; 21:1064–1067. PMID: 17027552.

16. De Smet L, Debeer P, Degreef I. Fixation of a periprosthetic humeral fracture with CCG-cable system. Acta Chir Belg. 2005; 105:543–544. PMID: 16315845.

17. Changulani M, Jain UK, Keswani T. Comparison of the use of the humerus intramedullary nail and dynamic compression plate for the management of diaphyseal fractures of the humerus. A randomised controlled study. Int Orthop. 2007; 31:391–395. PMID: 16900354.

18. Jiang R, Luo CF, Zeng BF, Mei GH. Minimally invasive plating for complex humeral shaft fractures. Arch Orthop Trauma Surg. 2007; 127:531–535. PMID: 17401571.

19. Kim JW, Oh CW, Byun YS, Kim JJ, Park KC. A prospective randomized study of operative treatment for noncomminuted humeral shaft fractures: conventional open plating versus minimal invasive plate osteosynthesis. J Orthop Trauma. 2015; 29:189–194. PMID: 25210833.
20. Rhinelander FW, Stewart CL. Experimental fixation of femoral osteotomies by cerclage with nylon straps. Clin Orthop Relat Res. 1983; (179):298–307.

21. Ekholm R, Ponzer S, Törnkvist H, Adami J, Tidermark J. Primary radial nerve palsy in patients with acute humeral shaft fractures. J Orthop Trauma. 2008; 22:408–414. PMID: 18594306.

22. Livani B, Belangero WD, Castro de Medeiros R. Fractures of the distal third of the humerus with palsy of the radial nerve: management using minimally-invasive percutaneous plate osteosynthesis. J Bone Joint Surg Br. 2006; 88:1625–1628. PMID: 17159176.
Fig. 1
(A and B) A 29-year-old man with an OTA/AO type-B2 right humeral shaft fracture after a slip down event. Open reduction and internal fixation of the fragments with two cerclage cables followed by intramedullary nailing was performed. (C and D) A radiograph taken 4.5 months after surgery shows bone union. OTA, Orthopaedic Trauma Association.
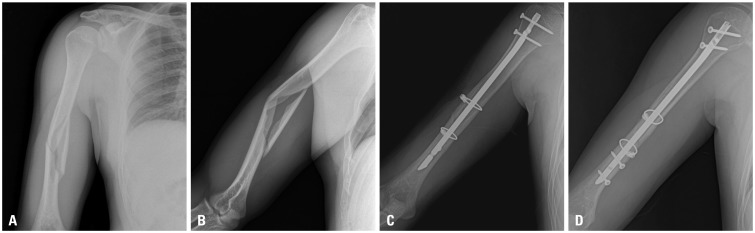
Table 1
Background Data of Patients Enrolled in the Cable and Non-Cable Groups
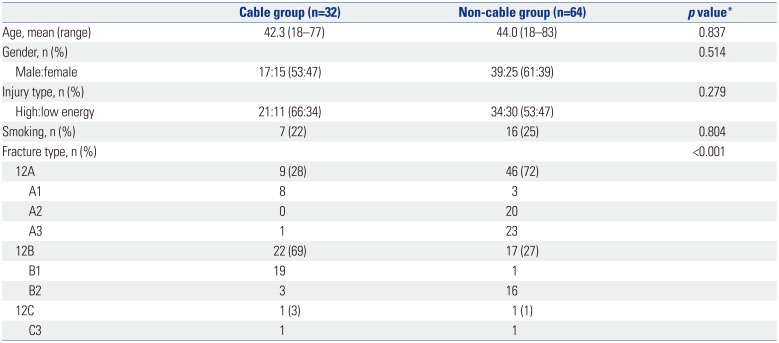
Table 2
Clinical Outcomes, Including Time to Union, Operation Time, Functional Scores, and Complications, in the Cable and Non-Cable Groups




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download