Abstract
Purpose
Children and adolescents diagnosed with cancer experience emotional distress, such as sadness, worrying, and irritability. However, there is little information about the psychological well-being of parents at the time of their child's diagnosis. We sought to identify factors that were associated with emotional distress in cancer patients as a basis for developing innovative psychological interventions.
Materials and Methods
A retrospective chart review was performed on patients newly diagnosed with cancer at a single center in Korea from 2014 to 2016. Eighty-five patients and their mothers completed psychological inventories. To determine factors associated with emotional distress in patients, we assessed the psychological inventory results using multiple linear regression after performing correlation analysis.
Results
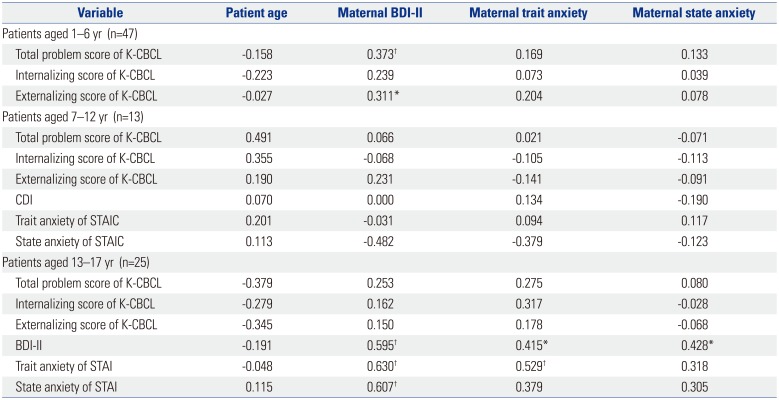
The maternal Beck Depression Inventory-II (BDI-II) score was positively correlated with total problem scores and externalizing scores in patients aged less than 7 years. In patients aged 7–12 years, there was no significant association between the patient's emotional distress and other variables. In contrast, the maternal BDI-II score was the strongest factor associated with patient depression in adolescents.
Conclusion
We suggest that the most important factor affecting emotional distress in children and adolescents with cancer is maternal depression, especially in patients aged 1–6 years and aged 13–17 years. Understanding the factors associated with emotional distress of cancer patients allows us to develop early psychiatric interventions for patients and their parents at the initial psychological crisis.
The probability of 5-year survival for cancer in children and adolescents now exceeds 80% due to dramatic advances in medicine.1 Despite great progress in developing cancer treatment, cancer remains the leading cause of disease-related death among children and adolescents.2 The diagnosis and treatment of cancer present numerous challenges and sources of stress for patients.3 Children and adolescents diagnosed with cancer experience emotional distress, such as sadness, worrying, and irritability among other negative emotions.4 Emotional distress in cancer patients is defined as an unpleasant experience of a psychological, social, and spiritual nature that may interfere with coping with cancer, its symptoms and treatments.5 The prevalence of emotional distress is high in patients diagnosed with cancer in general.6 Despite general agreement that cancer and its treatment can be stressful for patients, few studies have directly addressed the specific factors that affect children and adolescents diagnosed with cancer during early treatment. For children newly diagnosed with cancer, both the Child Behavior Checklist score and emotion-focused coping of their mothers predicted depression, anxiety, and global mental health.78
There is limited information on the psychological well-being of parents at the time of their child's diagnosis. Mothers of children newly diagnosed with cancer reported more depressive symptoms and emotion-focused coping than mothers of children with other acute illnesses such as gastrointestinal infections, fractures or lacerations.7 Previous studies have found that mothers experience substantial posttraumatic stress symptoms near the time of their child's or adolescent's cancer diagnosis and during the first 6 months of treatment.910 Neu, et al.11 reported that 27% of mothers experienced moderate to severe levels of depression and 46% of mothers experienced clinical anxiety during their child's cancer diagnosis. Elevated levels of maternal anxiety and depression may have an impact on an adolescent diagnosed with cancer since depression in mothers has been associated with higher levels of depression in children and adolescents.1213 A recent review of the psychosocial aspects of parents revealed that distress may impair vulnerable parents and may impact children's adjustment to cancer.14
The potential risk factors identified for maladjustment in cancer patients include cancer stage15 and recurrence status.16 In addition to disease factors, patients with premorbid psychiatric history1718 or low resilience are at risk for greater distress when coping with a high symptom burden. According to studies on patient-physician relationships, a physician's empathetic attitude can also have a positive influence on psychological adjustments in newly diagnosed cancer patients.1920 In children, individual variation in adjustment to cancer may be better understood in terms of differences in a child's temperament and coping style.21 Santos, et al.22 reported that family functioning is also a key issue for understanding adaptation in pediatric cancer.
However, less is known about the overall psychological effect of cancer on infants, children and adolescents. More information is needed on the specific factors that affect emotional distress of children and adolescents diagnosed with cancer, and how these stressors are associated with emotional adjustment to the disease and its treatment, particularly in children and adolescents.
The goal of this article was to investigate whether maternal and patient factors are associated with emotional distress of patients newly diagnosed with cancer. From a developmental perspective, we expected differences among infants, children, and adolescents.
Research approval for a retrospective chart review was granted by the Institutional Review Board for research with human subjects at Yonsei University Severance Hospital. We retrospectively reviewed the medical records of patients newly diagnosed with cancer who were admitted to Yonsei Cancer Center and referred for psychiatric consultation between November 2014 and October 2016. Of 210 patients, 85 patients were included in the analysis. Inclusion criteria for patients were as follows: newly diagnosed with cancer including relapse after remission; diagnosed within the past 3 months; no pre-existing mental disorders; completed psychological inventories at the initial psychiatric evaluation; sufficient knowledge of the Korean language; presence of a mother as a caregiver; and age between 1 and 17 years.
The following psychological inventory results were obtained from the patients and their mothers at the initial psychiatric evaluation. The Korean-Child Behavior Checklist (K-CBCL) was completed by mothers considering the behavior of their children in the previous 3 months. The inventory consists of 119 items which are summed into three global scores (total problem, internalizing, and externalizing scores). the inventories for the children between ages 7 and 12 years were: 1) Children's Depression Inventory (CDI) (Kovac, 1981) and 2) State-Trait Anxiety Inventory for Children (STATIC) (Spielberger, 1973). The inventories for the children between ages 13 and 17 years were: 1) Beck Depression Inventory-II (BDI-II) (Beck, et al., 1979) and 2) State-Trait Anxiety Inventory (STAI) (Spielberger, 1983). The STAIC and STAI consist of two subscales that measure state anxiety and trait anxiety.
All statistical analyses in this study were performed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA). Categorical variables were presented as percentages. Pearson correlation analysis was used to analyze correlations between patient data including age, K-CBCL, CDI, BDI-II, STATIC, and STAI scores, and maternal data including BDI-II and STAI scores. To determine factors associated with patient emotional distress, multiple linear regression was used after performing correlation analyses. The stepwise method was used for the order of significance in the correlation analysis. Correlations between variables with p-values<0.05 were considered significant.
Table 1 lists the demographic and clinical characteristics of patients and their mothers. Patient mean age was 7.6 years. The total number of patients included in the analysis was 85. There were 47 infants and preschool-aged children in the 1–6 year patient age group, 13 school-aged children in the 7–12 year patient age group, and 25 adolescents in the 13–17 year patient age group. About 24.7% were diagnosed with acute lymphoblastic leukemia, and 10.6% were diagnosed with acute myeloid leukemia. About 9.4% had relapsed cancer.
Maternal BDI-II score was positively correlated with patient total problem and externalizing scores (Fig. 1A and C), although there was no significant association between maternal BDI-II score and patient internalizing score (Fig. 1B). Among the variables, maternal BDI-II score was the only factor associated with patient total problem and externalizing scores (Table 2).
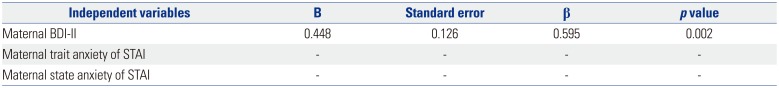
We conducted analyses of the association between patient emotional distress and other variables (Table 3). Patient BDI-II score was associated with various factors including maternal BDI-II (Fig. 3), maternal trait anxiety and maternal state anxiety scores. Patient trait anxiety score was associated with maternal BDI-II and maternal trait anxiety scores. Patient state anxiety was associated with maternal state anxiety. Factors related to the BDI-II score in patients aged 13–17 were identified using multiple stepwise linear regression analysis. Maternal BDI-II score was the only factor associated with patient depression (Table 4).
Our study extends the findings of previous research on the psychological responses of patients to cancer diagnosis by assessing the more immediate emotional responses within 3 months of diagnosis. Most previous studies examined patients with terminal cancer23 or cancer survivors,24 while others assessed patients during the first year after diagnosis.2125 In our present study, most patients were scored in the subclinical range of psychological inventories. This finding is comparable with the findings of previous studies. This might be related to patient's different coping strategies to deal with acute stress. In addition, we identified that maternal depression emerged as the strongest factor associated with subjective emotional distress in adolescents newly diagnosed with cancer.
In infants and preschoolers, emotion regulation is dyadic because the primary caregiver is central to providing regulation that an offspring needs, which in turn facilitates the development of autonomous emotion regulation.2627 Previous studies suggested that increased parenting stress predicted poorer behavioral, emotional, and social adjustments in children with cancer.2829 Greater illness-related parenting stress is correlated with greater parental emotional distress such as depression and anxiety.30 Manian and Bornstein31 suggested that infants of depressed mothers used more internally self-soothing strategies to reduce negative emotions than infants of mothers who were not depressed. In our sample, an elevated maternal BDI-II score was correlated with total problem score and externalizing score in patients aged 1–6 years. It seems that parenting issues, mediated by maternal depression, can lead to emotional distress in infants and preschoolers and result in externalized symptoms including aggressive behaviors. However, maternal BDI-II score was not correlated with internalizing score. This discrepancy might be due to the high ratio of boys to girls in patients aged 1–6 years. Previous studies reported that current maternal depression was related positively to internalizing score of girls and to externalizing score of boys.32 In addition, illness-related parenting stress is related to parental responsibility for managing treatment.33 Because children younger than 7 years old have less autonomy and depend more on their mothers, their mothers may feel a greater responsibility than mothers of children older than 7 years. In adolescent patients, depressive mood and anxiety were positively correlated with maternal depression; in contrast, subjective emotional distress in school-aged patients was not related to maternal depression.
There are several potential explanations for the discrepancy found between children and adolescents. The difference could be explained primarily by the development of empathy in adolescents. Two components of empathy, empathic concern and perspective thinking, increase throughout adolescence.34 Perspective thinking is a cognitive component of empathy that does not begin to emerge until childhood, although empathic concern which is an emotional component of empathy appears to stabilize in early childhood.3435 Perspective thinking allows the understanding of the mental state and viewpoints of others, and moderates the relationship between cognitive and emotional empathy.36 Hereby, adolescents with cancer may be more susceptible to maternal depression than school-aged children. This is in line with findings that subjective illness perception in adolescent and young adult cancer patients is the strongest predictor of their own stress symptoms and is significantly correlated with stress symptoms in caregivers.37
However, school-aged children have difficulties recognizing their mother's emotional status because of their immature empathy. In addition, they often perceive their illness as a punishment for a perceived wrong.38 School-aged patients' subjective depressive mood and anxiety may be most strongly related to their own beliefs about their illness rather than maternal emotional distress. Furthermore, emotional understanding in young children developes primarily through socialization processes within the family context, especially through the quality of mother-child relationships. Sympathy and personal distress responses to a mother's distress might facilitate the socialization process by allowing children to focus on their parent rather than their own distress, and providing opportunities for parents to respond to children's emotions facilitate emotional learning.39
This study has several limitations. First, the cross-sectional study design does not provide the ability to clearly discern psychological trajectories over time. In addition, the direction of the influence between parental distress and patient distress could not be elucidated. Future research may use a longitudinal study design to clarify the direction of this moderation effect. Second, the number of patients with relapsed cancer was not large enough to analyze the difference between the initial diagnosis and relapse. Relapse of cancer is known to be negatively associated with a child's self-perception and positively associated with trait anxiety.40 Third, the number of patients aged 7–12 was small compared to other age group, therefore, there might not be a significant correlation. Fourth, we were unable to make broader conclusion about vulnerable maternal characteristics. The inclusion of multiple variables including maternal age, coping strategies and attachment types of mothers would provide advanced results. Fifth, further research may benefit from focusing on more homogeneous samples of children with specific diagnosis of cancer or specific treatment received that may present specific types of stressors. And finally, we included cancer patients only in this study; further research is necessary to compare the differences between cancer diagnosis and other traumatic stressors.
In conclusion, this study suggests that the most important factor affecting the emotional distress of patients, especially adolescents, is maternal depression. Understanding the factors associated with emotional distress of cancer patients allows us to develop early psychiatric interventions including supportive psychotherapy for patients and their primary caregivers at the initial psychological crisis. Finally, the results suggest that early psychiatric assessment is important to reduce emotional distress and improve the quality of life of patients. Future research should continue to develop innovative interventions for managing emotional distress of patients in the oncology setting.
ACKNOWLEDGEMENTS
This work was supported by the research fund from Yonsei Psychiatric Association (2015).
References
1. McGregor LM, Metzger ML, Sanders R, Santana VM. Pediatric cancers in the new millennium: dramatic progress, new challenges. Oncology (Williston Park). 2007; 21:809–820. PMID: 17722742.
2. Sun W, Gaynon PS, Sposto R, Wayne AS. Improving access to novel agents for childhood leukemia. Cancer. 2015; 121:1927–1936. PMID: 25678105.

3. Rodriguez EM, Dunn MJ, Zuckerman T, Vannatta K, Gerhardt CA, Compas BE. Cancer-related sources of stress for children with cancer and their parents. J Pediatr Psychol. 2012; 37:185–197. PMID: 21841187.

4. Collins JJ, Devine TD, Dick GS, Johnson EA, Kilham HA, Pinkerton CR, et al. The measurement of symptoms in young children with cancer: the validation of the Memorial Symptom Assessment Scale in children aged 7-12. J Pain Symptom Manage. 2002; 23:10–16. PMID: 11779663.
5. National Comprehensive Cancer Network. Distress management. Clinical practice guidelines. J Natl Compr Canc Netw. 2003; 1:344–374. PMID: 19761069.
6. Graves KD, Arnold SM, Love CL, Kirsh KL, Moore PG, Passik SD. Distress screening in a multidisciplinary lung cancer clinic: prevalence and predictors of clinically significant distress. Lung Cancer. 2007; 55:215–224. PMID: 17084483.

7. Barrera M, D'Agostino NM, Gibson J, Gilbert T, Weksberg R, Malkin D. Predictors and mediators of psychological adjustment in mothers of children newly diagnosed with cancer. Psychooncology. 2004; 13:630–641. PMID: 15334531.

8. Virtue SM, Manne S, Mee L, Bartell A, Sands S, Ohman-Strickland P, et al. The role of social and cognitive processes in the relationship between fear network and psychological distress among parents of children undergoing hematopoietic stem cell transplantation. J Clin Psychol Med Settings. 2014; 21:223–233. PMID: 25081956.

9. Phipps S, Long A, Hudson M, Rai SN. Symptoms of post-traumatic stress in children with cancer and their parents: effects of informant and time from diagnosis. Pediatr Blood Cancer. 2005; 45:952–959. PMID: 15806541.

10. Dunn MJ, Rodriguez EM, Barnwell AS, Grossenbacher JC, Vannatta K, Gerhardt CA, et al. Posttraumatic stress symptoms in parents of children with cancer within six months of diagnosis. Health Psychol. 2012; 31:176–185. PMID: 21942750.

11. Neu M, Matthews E, King NA, Cook PF, Laudenslager ML. Anxiety, depression, stress, and cortisol levels in mothers of children undergoing maintenance therapy for childhood acute lymphoblastic leukemia. J Pediatr Oncol Nurs. 2014; 31:104–113. PMID: 24608702.

12. Okado Y, Long AM, Phipps S. Association between parent and child distress and the moderating effects of life events in families with and without a history of pediatric cancer. J Pediatr Psychol. 2014; 39:1049–1060. PMID: 25064801.

13. Trask PC, Paterson AG, Trask CL, Bares CB, Birt J, Maan C. Parent and adolescent adjustment to pediatric cancer: associations with coping, social support, and family function. J Pediatr Oncol Nurs. 2003; 20:36–47. PMID: 12569433.

14. Kearney JA, Salley CG, Muriel AC. Standards of psychosocial care for parents of children with cancer. Pediatr Blood Cancer. 2015; 62(Suppl 5):S632–S683. PMID: 26700921.

15. Groarke A, Curtis R, Groarke JM, Hogan MJ, Gibbons A, Kerin M. Post-traumatic growth in breast cancer: how and when do distress and stress contribute? Psychooncology. 2016; 8. 08. [Epub]. DOI: 10.1002/pon.4243.

16. Andersen BL, Shapiro CL, Farrar WB, Crespin T, Wells-Digregorio S. Psychological responses to cancer recurrence. Cancer. 2005; 104:1540–1547. PMID: 16118802.

17. Stafford L, Komiti A, Bousman C, Judd F, Gibson P, Mann GB, et al. Predictors of depression and anxiety symptom trajectories in the 24 months following diagnosis of breast or gynaecologic cancer. Breast. 2016; 26:100–105. PMID: 27017248.

18. Alfonsson S, Olsson E, Hursti T, Lundh MH, Johansson B. Socio-demographic and clinical variables associated with psychological distress 1 and 3 years after breast cancer diagnosis. Support Care Cancer. 2016; 24:4017–4023. PMID: 27129841.
19. Roberts CS, Cox CE, Reintgen DS, Baile WF, Gibertini M. Influence of physician communication on newly diagnosed breast patients' psychologic adjustment and decision-making. Cancer. 1994; 74(1 Suppl):336–341. PMID: 8004605.

20. Cuisinier MC, Van Eijk JT, Jonkers R, Dokter HJ. Psychosocial care and education of the cancer patient: strengthening the physician's role. Patient Educ Couns. 1986; 8:5–16. PMID: 10300737.

21. Miller KS, Vannatta K, Compas BE, Vasey M, McGoron KD, Salley CG, et al. The role of coping and temperament in the adjustment of children with cancer. J Pediatr Psychol. 2009; 34:1135–1143. PMID: 19451171.

22. Santos S, Crespo C, Canavarro MC, Kazak AE. Parents' romantic attachment predicts family ritual meaning and family cohesion among parents and their children with cancer. J Pediatr Psychol. 2017; 42:114–124. Guest Editors: Gerhardt CA, Berg CA, et al.

23. Hayes RD, Lee W, Rayner L, Price A, Monroe B, Hansford P, et al. Gender differences in prevalence of depression among patients receiving palliative care: the role of dependency. Palliat Med. 2012; 26:696–702. PMID: 21775410.

24. Wang R, Syed IA, Nathan PC, Barr RD, Rosenberg-Yunger ZR, Klassen AF. Exploring cancer worry in adolescent and young adult survivors of childhood cancers. J Adolesc Young Adult Oncol. 2015; 4:192–199. PMID: 27077153.

25. Zebrack BJ, Corbett V, Embry L, Aguilar C, Meeske KA, Hayes-Lattin B, et al. Psychological distress and unsatisfied need for psychosocial support in adolescent and young adult cancer patients during the first year following diagnosis. Psychooncology. 2014; 23:1267–1275. PMID: 24664958.

26. Ostlund BD, Measelle JR, Laurent HK, Conradt E, Ablow JC. Shaping emotion regulation: attunement, symptomatology, and stress recovery within mother-infant dyads. Dev Psychobiol. 2017; 59:15–25. PMID: 27481553.

27. Luby JL, Belden A, Harms MP, Tillman R, Barch DM. Preschool is a sensitive period for the influence of maternal support on the trajectory of hippocampal development. Proc Natl Acad Sci U S A. 2016; 113:5742–5747. PMID: 27114522.

28. Colletti CJ, Wolfe-Christensen C, Carpentier MY, Page MC, McNall-Knapp RY, Meyer WH, et al. The relationship of parental overprotection, perceived vulnerability, and parenting stress to behavioral, emotional, and social adjustment in children with cancer. Pediatr Blood Cancer. 2008; 51:269–274. PMID: 18454464.

29. Fedele DA, Mullins LL, Wolfe-Christensen C, Carpentier MY. Longitudinal assessment of maternal parenting capacity variables and child adjustment outcomes in pediatric cancer. J Pediatr Hematol Oncol. 2011; 33:199–202. PMID: 21336169.

30. Manuel JC. Risk and resistance factors in the adaptation in mothers of children with juvenile rheumatoid arthritis. J Pediatr Psychol. 2001; 26:237–246. PMID: 11329483.

31. Manian N, Bornstein MH. Dynamics of emotion regulation in infants of clinically depressed and nondepressed mothers. J Child Psychol Psychiatry. 2009; 50:1410–1418. PMID: 19788549.

32. Foster CE, Webster MC, Weissman MM, Pilowsky DJ, Wickramaratne PJ, Rush AJ, et al. Course and severity of maternal depression: associations with family functioning and child adjustment. J Youth Adolesc. 2008; 37:906–916. PMID: 25013241.

33. Helgeson VS, Becker D, Escobar O, Siminerio L. Families with children with diabetes: implications of parent stress for parent and child health. J Pediatr Psychol. 2012; 37:467–478. PMID: 22267104.

34. Van der Graaff J, Branje S, De Wied M, Hawk S, Van Lier P, Meeus W. Perspective taking and empathic concern in adolescence: gender differences in developmental changes. Dev Psychol. 2014; 50:881–888. PMID: 24040846.

35. Eisenberg N, Cumberland A, Guthrie IK, Murphy BC, Shepard SA. Age changes in prosocial responding and moral reasoning in adolescence and early adulthood. J Res Adolesc. 2005; 15:235–260. PMID: 20592955.

36. Hinnant JB, O'Brien M. Cognitive and emotional control and perspective taking and their relations to empathy in 5-year-old children. J Genet Psychol. 2007; 168:301–322. PMID: 18200891.

37. Juth V, Silver RC, Sender L. The shared experience of adolescent and young adult cancer patients and their caregivers. Psychooncology. 2015; 24:1746–1753. PMID: 25808790.

38. Walker C, Papadopoulos L, Lipton M, Hussein M. The importance of children's illness beliefs: the Children's Illness Perception Questionnaire (CIPQ) as a reliable assessment tool for eczema and asthma. Psychol Health Med. 2006; 11:100–107. PMID: 17129899.

39. Tully EC, Donohue MR, Garcia SE. Children's empathy responses and their understanding of mother's emotions. Cogn Emot. 2015; 29:118–129. PMID: 24650197.

40. Hockenberry-Eaton M, Dilorio C, Kemp V. The relationship of illness longevity and relapse with self-perception, cancer stressors, anxiety, and coping strategies in children with cancer. J Pediatr Oncol Nurs. 1995; 12:71–79. PMID: 7612200.

Fig. 1
Correlations between maternal BDI-II score and K-CBCL score of patients aged 1–6 years. (A) Scatter plot showing a significant positive correlation between maternal BDI-II score and patient total problem score (p<0.01, r=0.373, n=47). (B) Scatter plot showing lack of correlation between maternal BDI-II score and patient internalizing score (p=0.11, r=0.239, n=47). (C) Scatter plot showing a significant positive correlation between maternal BDI-II score and patient externalizing score (p<0.05, r=0.311, n=47). Comparisons were made using the Pearson correlation. Each point represents an individual patient. BDI-II, Beck Depression Inventory-II; K-CBCL, Korean-Child Behavior Checklist.
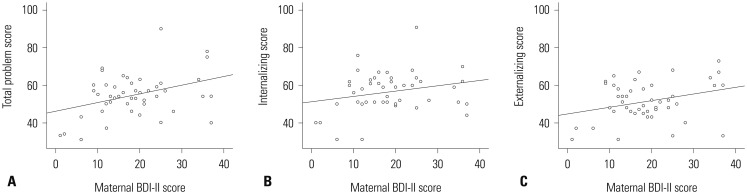
Fig. 2
Correlation between maternal BDI-II score and CDI score of patients aged 7–12 years. Scatter plot showing lack of correlation between maternal BDI-II score and patient CDI score (p=0.99, r=0.00, n=13). Comparisons were made using the Pearson correlation. Each point represents an individual patient. BDI-II, Beck Depression Inventory-II; CDI, Children's Depression Inventory.

Fig. 3
Correlation between maternal BDI-II score and BDI-II score of patients aged 13–17 years. Scatter plot showing a significant positive correlation between maternal BDI-II score and patient BDI-II score (p<0.01, r=0.595, n=25). Comparisons were made using the Pearson correlation. Each point represents an individual patient. BDI-II, Beck Depression Inventory-II.
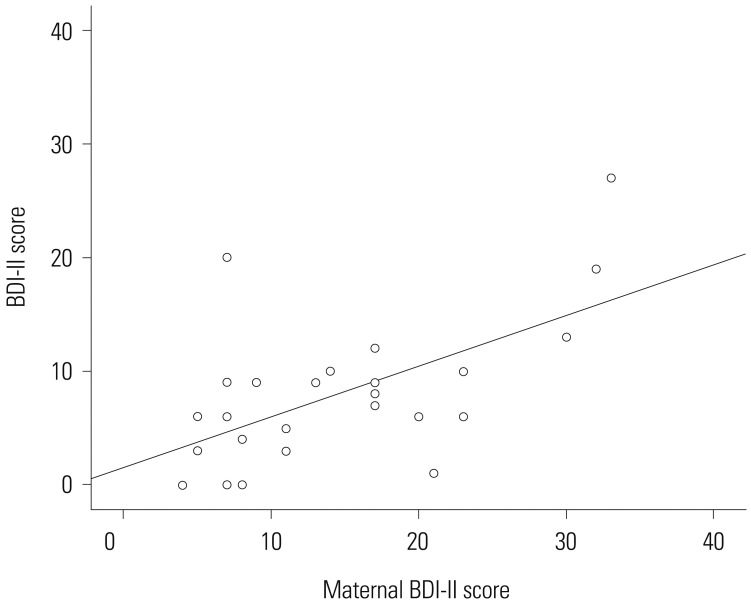
Table 1
Demographic and Clinical Characteristics of Patients and Their Mothers (n=85)
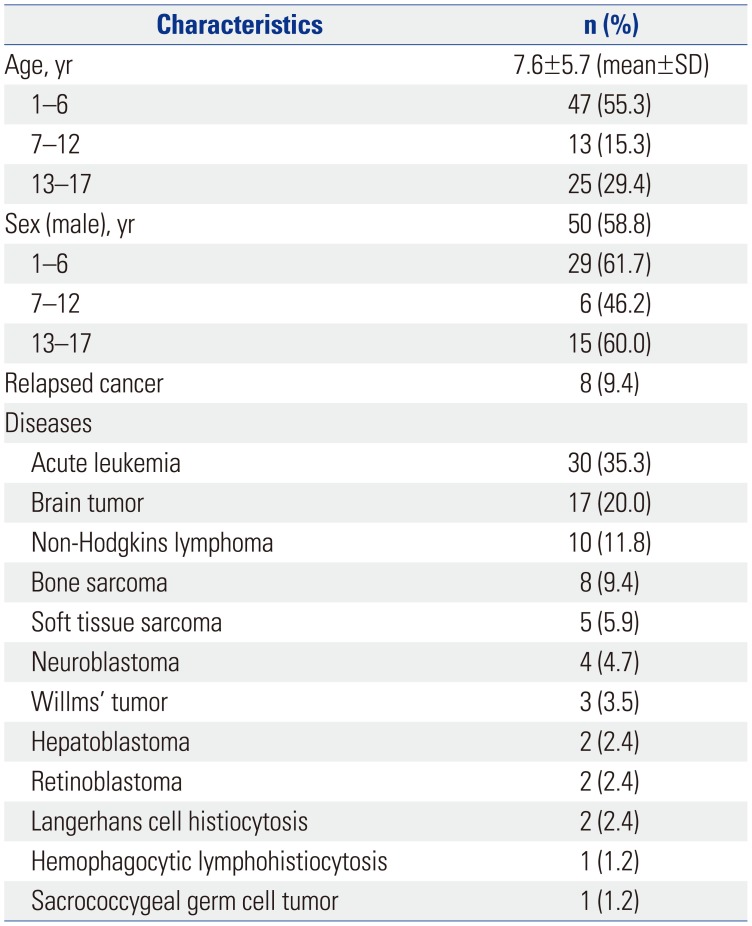
Table 2
Emotional Distress of Patients and Their Mothers (n=85)
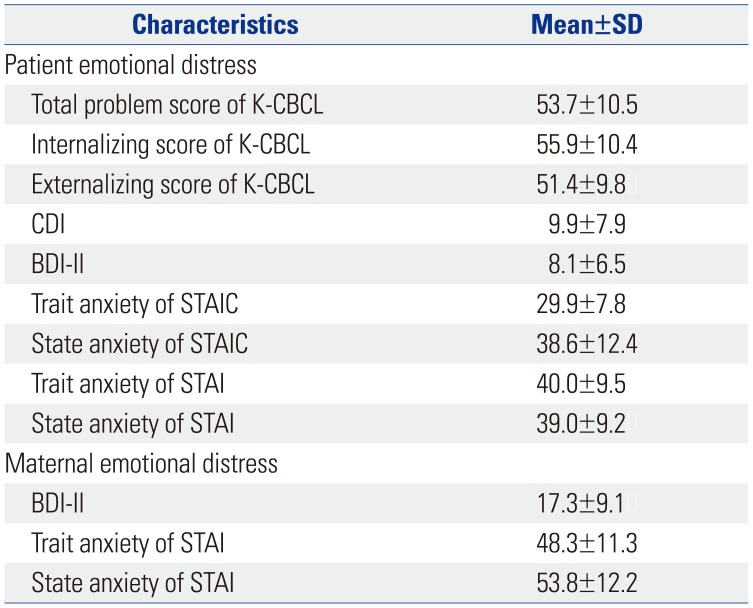
Table 3
Correlations between Patient Emotional Distress and Patient or Maternal Factors (n=85)




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download