Abstract
Purpose
Materials and Methods
Results
Figures and Tables
 | Fig. 1Expressions of miR-34a/b/c in TNBC patients and HCs. (A) miR-34a. (B) miR-34b. (C) miR-34c. TNBC, triple-negative breast cancer; HC, health control; miR-34, microRNA-34. |
 | Fig. 2Kaplan-Meier curve analysis of miR-34a/b/c for overall survival. (A) miR-34a. (B) miR-34b. (C) miR-34c. miR-34, microRNA-34. |
Table 1
Demographic, Clinical, and Pathological Characteristic of TNBC Patients at Baseline

Table 2
Univariate and Multivariate Cox Proportional Hazards Regression Analysis of Risk Factors for Overall Survival in TNBC Patients
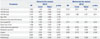
TNBC, triple-negative breast cancer; HR, hazard ratio; CI, confidence interval; miR-34, microRNA-34.
Data are presented as HR, 95% CI and p value. A p value <0.05 was considered statistically significant. Significance was determined by univariate Cox proportional hazards regression analysis, and all factors with a p value <0.1 were further analyzed by multivariate Cox proportional hazards regression.
Table 3
Risk Factors Analysis for Overall Survival in TNM Stage I–III Patients

HR, hazard ratio; CI, confidence interval; miR-34, microRNA-34.
Data are presented as HR, 95% CI and p value. A p value <0.05 was considered statistically significant. Significance was determined by univariate Cox proportional hazards regression analysis, and all factors with a p value <0.1 were further analyzed by multivariate Cox proportional hazards regression.
Table 4
Risk factors Analysis for Overall Survival in TNM Stage IV Patients

HR, hazard ratio; CI, confidence interval; miR-34, microRNA-34.
Data are presented as HR, 95% CI and p value. A p value <0.05 was considered statistically significant. Significance was determined by univariate Cox proportional hazards regression analysis, and all factors with a p value <0.1 were further analyzed by multivariate Cox proportional hazards regression.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download