Abstract
Purpose
CD93 is receiving renewed attention as a biomarker of inflammation. We aimed to evaluate the potential for serum sCD93 to serve as a novel biomarker for allergic inflammation.
Materials and Methods
We enrolled 348 subjects with an allergic disease [allergic rhinitis (AR), chronic spontaneous urticaria (CSU), or bronchial asthma (BA)], including 14 steroid-naïve BA patients who were serially followed-up.
Results
The serum sCD93 levels (ng/mL) in patients with exacerbated AR (mean±standard deviation, 153.1±58.4) were significantly higher than in patients without AR (132.2±49.0) or with stable AR (122.3±42.1). Serum sCD93 levels in exacerbated CSU (169.5±42.8) were also significantly higher than those in non-CSU (132.4±51.6) and stable CSU (122.8±36.2). This trend was also seen in BA. Serum levels in patients with ICS-naïve BA (161.4±53.1) were significantly higher than those in healthy controls without BA (112.2±30.8), low- and medium-dose ICS users. Serum sCD93 levels in high-dose ICS users (72.2±20.6) were significantly lower than those in low- and medium-dose users. The serum sCD93 levels in steroid-naïve patients with BA (195.1±72.7) decreased after ICS use for 4 weeks (134.4±42.8) and 8 weeks (100.7±13.4), serially.
The prevalence of allergic diseases has been increasing worldwide. Bronchial asthma (BA) is a chronic inflammatory airway allergic disease. There are some objective biomarkers to diagnose asthma and to assess its severity, including forced expiratory volume in one second (FEV1), FEV1/forced vital capacity (FVC), fraction of exhaled nitric oxide, and sputum eosinophil and neutrophil counts.1,2,3,4 Other new markers, such as YKL-40 and clusterin, have recently received attention.56 However, evaluation of these parameters requires a patient to blow into a machine or to expectorate sputum. Due to the nature of asthma, many patients cannot perform these tests because of shortness of breath, absence of sputum, and non-compliance. In addition, allergic rhinitis (AR) and chronic spontaneous urticaria (CSU) have few biomarkers to diagnosis and evaluate their severity. Therefore, it is necessary to identify suitable serologic biomarkers of inflammation that may be easily evaluated in patients with allergic diseases.
CD93 is a cell surface protein that belongs to the newly discovered IXV family of transmembrane glycoproteins.7 CD93 is expressed on various cells involved in the inflammatory cascade and hematopoiesis. While CD93 was originally described as a complement 1q receptor that enhances phagocytosis and as a marker of developing B cells, CD93 is now recognized to be required for phagocytosis and immunity and to function as a novel regulator of inflammation.8910 Nonetheless, the molecular function of CD93 is still unknown. The regulatory role of CD93 in inflammation has been studied in various diseases. Soluble CD93 (sCD93) levels were significantly increased in the synovial fluid of rheumatoid arthritis patients.11 sCD93 expression in patients with systemic lupus erythematosus (SLE) is inversely correlated with prednisone dose.12 Overall, CD93 seems to be a therapeutic marker for inflammation, as serum levels are elevated during inflammation and decline following anti-inflammatory treatment. However, the clinical significance of serum sCD93 in allergic diseases, such as AR, CSU, and BA, has not been well studied.
We aimed to elucidate the clinical diagnostic value of sCD93 in various allergic diseases and to determine the suitability of sCD93 as a novel diagnostic and therapeutic biomarker.
We enrolled 414 subjects who were diagnosed with allergic diseases (at least one of these: AR, CSU, and BA) at the Allergy Asthma Center of the Severance Hospital in Seoul, Korea from May 2014 to September 2015. Among these subjects, 41 were excluded {15: recent severe allergic reaction, anaphylaxis; 19: ongoing immunotherapy dose-up; 4: activated status of another inflammatory disease [2: atopic dermatitis (AD); 1: rheumatoid arthritis, 1: Behcet's disease]; 3: severe cutaneous adverse drug reaction [2: toxic epidermal necrolysis, 1: Stevens-Johnson syndrome]}. Additionally, 25 patients refused the study. The 348 subjects enrolled in the cross sectional study were patients over the age of 19 who were admitted to one of the study clinics, were diagnosed with allergic diseases, and agreed to participate in this study, including submitting to all basic tests and the sCD93 blood test (Fig. 1).
Among the 348 patients, we selected steroid-naïve patients who were first diagnosed with BA at this visit and who required inhaled corticosteroid (ICS) treatment to define the effects of steroids on serum sCD93. A total of 313 patients were not eligible for the cohort study, because they were not diagnosed with BA, did not require ICS treatment, or were already using a steroid-containing inhaler. Fourteen patients who were eligible for the cohort study refused participation in this study, and 7 patients who agreed to participate were lost to follow-up. The 14 patients enrolled in the cohort study, which was serially followed-up, were treated with ICS, and their serum sCD93 levels were assessed after 4 or 8 weeks of ICS use (Fig. 1). They were prescribed by the low- or medium-dose of ICS according to the doctor's judgment.
BA was diagnosed by an allergy specialist based on clinical guidelines using a bronchodilator test and/or bronchial provocation test.13 AR,14 allergic conjunctivitis,15 AD,16 and CSU17 were diagnosed based on international guidelines. No systemic steroids therapy in past 8 weeks was given in AR, BA, and CSU groups.
This study was approved by the Institutional Review Board of Yonsei University College of Medicine (approval number: 4-2013-0397). All enrolled patients provided written informed consent.
All 348 patients enrolled in the cross sectional study underwent basic tests, including blood and sputum tests and a lung function test. The blood collection in exacerbated group was performed before steroids uses. First, a complete blood count was performed using an automated analyzer to determine blood eosinophil and neutrophil counts. Next, the eosinophil and neutrophil percentages in induced sputum were measured. The obtained sputum was centrifuged, and the supernatant was collected. Samples were diluted in phosphate-buffered saline and centrifuged at 450 rpm for 6 min to prepare cytology slides. After staining the slides with Wright's stain, a differential count was performed using a light microscope as reported previously.5 Lastly, FEV1 and FEV1/FVC were evaluated by pulmonary function test using commercially available equipment (MS-IOS; Masterlab-IOS, Jaeger, Wurzburg, Germany). All of these tests were conducted within 1 week of the date of blood collection for sCD93 measurement. The 14 patients who were enrolled in the cohort study were subjected to a repeat of all the tests, including a serum sCD93 level test, after 4 weeks or 8 weeks of ICS use. ICS was prescribed by an allergy specialist.
Blood samples were collected from all of the study participants and were centrifuged for 10 minutes at 3000 rpm at 15℃. The sCD93 levels in the supernatants (serum) were estimated using an enzyme-linked immunosorbent assay kit (Affymetrix eBioscience, Vienna, Austria) according to the manufacturer's instructions. The detection range for sCD93 was 3.3–400 ng/mL. All samples were measured in duplicate, and the results were expressed as ng/mL in serum.
Exacerbated allergic disease was defined as acute aggravation of allergic disease symptoms requiring increases or other changes in the medication regimen to relieve aggravated symptoms [exacerbated AR (eAR): sneezing, rhinorrhea, and nasal obstruction; exacerbated CSU (eCSU): number of hives and pruritus; exacerbated BA (eBA): cough, chest tightness, and dyspnea]. Stable allergic disease was defined by a stable status of the allergic disease, without any aggravated symptoms requiring changes in the medication regimen [stable AR (sAR); stable CSU (sCSU); stable BA (sBA)].
The dose of ICS use was assessed within 1 week of the date of blood collection for sCD93 measurement. Study participants were categorized according to ICS use as non-users, low-dose users, medium-dose users, and high-dose users based on the Global Initiative for Asthma guidelines.18
The levels of sCD93 were normally distributed, as defined by the Kolmogorov-Smirnov and Shapiro-Wilk tests. Then, we used the two-sample t-test (independent sample t-test) and analysis of variance, followed by a post-hoc Bonferroni test, to compare the sCD93 levels among the subgroups, including the comparison of serial sCD93 levels in steroid-naïve patients. Pearson's correlation was used to define the correlation between sCD93 levels and the assessed parameters. All statistical analyses were performed with SAS version 9.2 (SAS Institute Inc., Cary, NC, USA), and significance was defined as p<0.05.
The mean age of the 348 subjects enrolled in the cross sectional study was 44.0±16.9 (mean±standard deviation). Females were predominant (61.8%). Almost all of the patients had additional allergic diseases, including AR (84.4%) and BA (66.3%). The mean sCD93 level in 389 subjects was 132.6±50.0 ng/mL (Table 1).
We classified all the subjects into three groups according to the status of allergic disease. In AR, 28.4% and 56.0% of all subjects were classified into eAR and sAR, respectively. 54 subjects (15.5%) did not have AR and were defined as control. In CSU, eCSU, and sCSU occupied 4.0% and 13.8%, respectively. Almost subjects (82.2%) did not have CSU and were defined as control. In BA, 33.6% were controls, and 21.8% and 44.5% were classified as eBA and sBA, respectively (Table 2). The serum sCD93 levels in eAR cases (n=99, 153.1±58.4 ng/mL, mean±standard deviation) were significantly higher than those in controls who were never diagnosed with AR (n=54, 132.2±49.0 ng/mL) or sAR (n=195, 122.3±42.1 ng/mL). Serum sCD93 levels in controls and in sAR cases showed no significant difference (Fig. 2A). The serum sCD93 levels in eCSU cases (n=14, 169.5±42.8 ng/mL) were significantly higher than those in controls who were never diagnosed with CSU (n=286, 132.4±51.6 ng/mL) or sCSU (n=48, 122.8±36.2 ng/mL). Serum sCD93 levels in sCSU cases were not significantly different from those of controls (Fig. 2B). The serum sCD93 levels in eBA cases (n=76, 146.6±61.4 ng/mL) were significantly higher than those in controls who were never diagnosed with BA (n=117, 133.0±44.5 ng/mL) or sBA (n=155, 125.4±46.5 ng/mL). Serum sCD93 levels in sBA cases were similar to those in controls (Fig. 2C). Serum sCD93 levels were higher in patients with exacerbated allergic diseases than in those whose diseases were stable.
When we selected pure allergic disease and pure control group, the results are not far distinct. Only 2 patients who had neither AR, BA, nor CSU were included in the pure control group (sCD93 level=170.0±28.8). In patients in AR who had neither BA nor CSU, sCD93 levels in sAR (n=47, 113.9±30.9 ng/mL) were significantly lower than those in eAR (n=24, 162.1±53.6 ng/mL). BA showed insignificant results. In patients in CSU who had neither AR nor BA, sCD93 levels in sCSU (n=14, 115.5±34.2 ng/mL) was lower than those in eAR (n=5, 154.6±38.3 ng/ mL), without statistical significance (Supplementary Fig. 1, only online).
In Pearson's correlation analysis, there was no significant correlation between sCD93 levels and sputum eosinophil, sputum neutrophil, or serum eosinophil counts or FEV1, and FEV1/FVC. Although blood neutrophils showed statistically significant p values (=0.039), Pearson's coefficients were close to zero (=-0.11) (data not shown).
We analyzed serum sCD93 levels in BA patients according to ICS dose. We excluded eAR and eCSU patients to eliminate confounding factors. The serum sCD93 levels in non-ICS users with BA (n=28, 161.4±53.1 ng/mL, mean±standard deviation) were significantly higher than those in healthy controls who had never been diagnosed with BA (n=68, 112.2±30.8 ng/mL), low-dose ICS users (n=45, 125.7±42.0 ng/mL), and medium-dose ICS users (n=62, 113.5±35.5 ng/mL). The serum sCD93 levels in high dose ICS users (n=8, 72.2±20.6 ng/mL) were significantly lower than those in others. The serum sCD93 levels in the controls, low-dose ICS users, and medium-dose ICS users were not significantly different (Fig. 3).
In the cohort study, we analyzed the levels serum sCD93 serially in 14 steroid-naïve patients with BA who required ICS treatment. The mean patient age was 38.9±14.0 (mean±standard deviation) years. Females were predominant (64.3%). Almost patients had AR (78.6%). The mean value of sputum eosinophils (%) increased (16.3±19.8%), and the mean value of FEV1 showed a modest decrease (80.0±33.3%) following ICS treatment (Table 3).
The baseline serum sCD93 levels (ng/mL) in steroid-naïve BA patients (n=14, 195.1±72.7, mean±standard deviation) significantly decreased after 4 weeks of ICS use (n=12, 134.4±42.8) and 8 weeks of ICS use (n=6, 100.7±13.4) (p<0.05). Although the serum sCD93 levels at 8 week of treatment were lower than those at 4 weeks, this difference was not statistically significant (Fig. 4).
Our cross sectional study suggested that the serum sCD93 levels in patients with exacerbated allergic diseases (AR, CSU, and BA) are higher than in those with stable diseases. Furthermore, we confirmed that ICS doses used in patients with BA were inversely correlated with serum sCD93 levels. We then hypothesized that sCD93 levels could be affected by ICS use. In a cohort study used to confirm this hypothesis, we found that sCD93 levels significantly decreased after ICS treatment. This suggested that serum sCD93 might be worth further study as a potential novel diagnostic and therapeutic marker for allergic disease, especially asthma.
CD93 is both a regulator and indicator of inflammation in various inflammatory diseases, including peritonitis, SLE, and RA.111219 In addition, several studies have revealed that CD93 is associated with inflammation and immunity in heart disease and cancer.2021 Only two previous study assessed CD93 levels in asthmatic patients.2223 Baines, et al.22 showed that CD93 mRNA levels were correlated with neutrophilia in sputum samples of asthma patients on a low antioxidant diet (p=0.04). However, CD93 was evaluated in sputum rather than serum in this previous study, the number of patients was small (n=10), and asthma severity and other clinical conditions were not evaluated. Sigari, et al.23 showed the role of sCD93 as a novel biomarker in asthma exacerbation; however, the effects of antiinflammatory drugs were not considered. We have clarified the roles of sCD93 in asthma, and for the first time, in various allergic diseases, including AR and CSU.
The prevalence of allergic diseases is increasing worldwide, and useful biomarkers that can easily be applied to clinical practice are insufficient. Although there are several methods to obtain airway samples, including collecting sputum and exhaled air, there are few biomarkers for BA that can be easily assessed in clinics. In AR, the available diagnostic tools, rhinoscopy and allergic skin test, are expensive, time consuming, and invasive. CSU can be defined only by symptoms and clinical manifestations. This study revealed that serum sCD93 might serve as a novel biomarker for these allergic diseases.
This study revealed a correlation between sCD93 levels and ICS dose in patients. This result is in agreement with a previous study, where an inverse correlation was observed between CD93 expression and prednisone dose in SLE patients.12 However, the lower levels of serum sCD93 in high-dose ICS users than healthy controls who have never diagnosed as BA should be further studied.
The serum sCD93 levels in patients with stable allergic diseases were similar to those in healthy controls without allergic disease. In contrast, we found that steroid-naïve patients who were diagnosed with BA for the first time at this visit showed higher serum sCD93 levels than healthy controls who were never diagnosed with BA. Therefore, we suspect that the medications, including not only steroids but also anti-histamines, that the patients took to control their symptoms affected serum sCD93 levels. These effects should be studied further.
We have some limitations. The cross sectional study was an observational study, so we could not determine whether the medication reduced the serum sCD93 levels. Although we conducted a cohort study to address this possibility, it included too few steroid-naïve subjects with BA. However, this small number of subjects revealed significantly decreasing sCD93 levels over 8 weeks of treatment. This study was designed to evaluate the potential for sCD93 to serve as a diagnostic and therapeutic marker for asthma. We did not elucidate the underlying mechanism or determine whether sCD93 or ICS usage was the cause or effect of this phenomenon. We propose that there might be a significant correlation between sCD93 levels and inflammation in asthmatic patients, as well as in other inflammatory diseases. We are not sure whether sCD93 plays a significant role in the T helper 2 pathway, which is considered important in allergic diseases. The sCD93 might be involved in inflammation irrelevant to T helper pathway. In the present situation, with very few validated serologic biomarkers for allergic diseases, especially asthma, sCD93 may prove to be a useful biomarker in the evaluation of allergic disease. Last, the therapeutic protocols in the cohort study varied. The duration and dose of ICS was determined by doctor's judgment. An objective and fair criteria for therapeutic protocol should be applied. In addition, comparisons of sCD93 levels according to the status of asthma control might be more informative.
This is the first study to evaluate CD93 as a biomarker for various allergic diseases according to exacerbation and treatment. Although further studies are needed to determine the mechanisms by which sCD93 participates in the development and progression of allergic diseases, the studies presented here validate the use of sCD93 as a novel biomarker in allergic diseases, especially asthma.
Figures and Tables
Fig. 2
Changes in serum sCD93 levels in patients with AR (A), CSU (B), and BA (C) and disease exacerbation. The data are shown as the mean±standard error of the mean in the graph. *p<0.05. AR, allergic rhinitis; sAR, stable AR; eAR, exacerbated AR; CSU, chronic idiopathic urticaria; sCSU, stable CSU; eCSU, exacerbated CSU; BA, bronchial asthma; sBA, stable BA; eBA, exacerbated BA; sCD93, soluble CD93.

Fig. 3
Serum sCD93 levels according to ICS dose. The data are shown as the mean±standard error of the mean in the graph. *p<0.05 compared to the other groups. ICS, inhaled corticosteroids; BA, bronchial asthma; Control, healthy control without BA; None, non-ICS-users with BA; Low, low-dose ICS users; Med, medium-dose ICS users; High, high-dose ICS users; sCD93, soluble CD93.
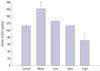
Fig. 4
Serial serum sCD93 levels during treatment with ICS in steroid-naïve patients with BA. *p<0.05 between groups. ICS, inhaled corticosteroids; BA, bronchial asthma; sCD93, soluble CD93.

Table 1
Clinical Characteristics of Cross Sectional Study Subjects

Table 2
Prevalence of Exacerbated and Stable Allergic Disease

Table 3
Clinical Characteristics and Laboratory Findings of Cohort Study Subjects

ACKNOWLEDGEMENTS
This work was supported by the National Research Foundation of Korea(NRF) grant funded by the Korea government (Ministry of Science, ICT & Future Planning) (No. 2015R1C1 A1A02036533).
References
1. Paro-Heitor ML, Bussamra MH, Saraiva-Romanholo BM, Martins MA, Okay TS, Rodrigues JC. Exhaled nitric oxide for monitoring childhood asthma inflammation compared to sputum analysis, serum interleukins and pulmonary function. Pediatr Pulmonol. 2008; 43:134–141.

2. Haccuria A, Michils A, Michiels S, Van Muylem A. Exhaled nitric oxide: a biomarker integrating both lung function and airway inflammation changes. J Allergy Clin Immunol. 2014; 134:554–559.

3. Moore WC, Hastie AT, Li X, Li H, Busse WW, Jarjour NN, et al. Sputum neutrophil counts are associated with more severe asthma phenotypes using cluster analysis. J Allergy Clin Immunol. 2014; 133:1557–1563.

4. Bandyopadhyay A, Roy PP, Saha K, Chakraborty S, Jash D, Saha D. Usefulness of induced sputum eosinophil count to assess severity and treatment outcome in asthma patients. Lung India. 2013; 30:117–123.

5. Lee JH, Park KH, Park JW, Hong CS. YKL-40 in induced sputum after allergen bronchial provocation in atopic asthma. J Investig Allergol Clin Immunol. 2012; 22:501–507.
6. Kwon HS, Kim TB, Lee YS, Jeong SH, Bae YJ, Moon KA, et al. Clusterin expression level correlates with increased oxidative stress in asthmatics. Ann Allergy Asthma Immunol. 2014; 112:217–221.

7. Greenlee MC, Sullivan SA, Bohlson SS. CD93 and related family members: their role in innate immunity. Curr Drug Targets. 2008; 9:130–138.

8. Nepomuceno RR, Henschen-Edman AH, Burgess WH, Tenner AJ. cDNA cloning and primary structure analysis of C1qR(P), the human C1q/MBL/SPA receptor that mediates enhanced phagocytosis in vitro. Immunity. 1997; 6:119–129.

9. Norsworthy PJ, Fossati-Jimack L, Cortes-Hernandez J, Taylor PR, Bygrave AE, Thompson RD, et al. Murine CD93 (C1qRp) contributes to the removal of apoptotic cells in vivo but is not required for C1q-mediated enhancement of phagocytosis. J Immunol. 2004; 172:3406–3414.

10. Greenlee-Wacker MC, Galvan MD, Bohlson SS. CD93: recent advances and implications in disease. Curr Drug Targets. 2012; 13:411–420.

11. Jeon JW, Jung JG, Shin EC, Choi HI, Kim HY, Cho ML, et al. Soluble CD93 induces differentiation of monocytes and enhances TLR responses. J Immunol. 2010; 185:4921–4927.

12. Moosig F, Fähndrich E, Knorr-Spahr A, Böttcher S, Ritgen M, Zeuner R, et al. C1qRP (CD93) expression on peripheral blood monocytes in patients with systemic lupus erythematosus. Rheumatol Int. 2006; 26:1109–1112.

13. Boulet LP, FitzGerald JM, Reddel HK. The revised 2014 GINA strategy report: opportunities for change. Curr Opin Pulm Med. 2015; 21:1–7.
14. Bousquet J, Reid J, van Weel C, Baena Cagnani C, Canonica GW, Demoly P, et al. Allergic rhinitis management pocket reference 2008. Allergy. 2008; 63:990–996.

15. Bielory L, Meltzer EO, Nichols KK, Melton R, Thomas RK, Bartlett JD. An algorithm for the management of allergic conjunctivitis. Allergy Asthma Proc. 2013; 34:408–420.

16. Eichenfield LF, Tom WL, Chamlin SL, Feldman SR, Hanifin JM, Simpson EL, et al. Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014; 70:338–351.
17. Zuberbier T, Aberer W, Asero R, Bindslev-Jensen C, Brzoza Z, Canonica GW, et al. The EAACI/GA(2) LEN/EDF/WAO Guideline for the definition, classification, diagnosis, and management of urticaria: the 2013 revision and update. Allergy. 2014; 69:868–887.

18. Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008; 31:143–178.

19. Greenlee-Wacker MC, Briseño C, Galvan M, Moriel G, Velázquez P, Bohlson SS. Membrane-associated CD93 regulates leukocyte migration and C1q-hemolytic activity during murine peritonitis. J Immunol. 2011; 187:3353–3361.

20. Mälarstig A, Silveira A, Wågsäter D, Öhrvik J, Bäcklund A, Samnegård A, et al. Plasma CD93 concentration is a potential novel biomarker for coronary artery disease. J Intern Med. 2011; 270:229–236.

21. Daino K, Ugolin N, Altmeyer-Morel S, Guilly MN, Chevillard S. Gene expression profiling of alpha-radiation-induced rat osteosarcomas: identification of dysregulated genes involved in radiation-induced tumorigenesis of bone. Int J Cancer. 2009; 125:612–620.

SUPPLEMENTARY MATERIAL
Supplementary Fig. 1
Serum sCD93 levels in patients with exacerbated and stable allergic disease when we selected pure allergic disease. *p<0.05 between groups. AR, allergic rhinitis; sAR, stable AR; eAR, exacerbated AR; BA, bronchial asthma; sBA, stable BA; eBA, exacerbated BA; CSU, chronic idiopathic urticaria; sCSU, stable CSU; eCSU, exacerbated CSU; sCD93, soluble CD93.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download