Abstract
Purpose
CO2 leakage along the trocar (chimney effect) has been proposed to be an important factor underlying port-site metastasis after laparoscopic surgery. This study aimed to test this hypothesis by comparing the incidence of port-site metastasis between B-ultrasound-guided and laparoscopically-assisted hyperthermic intraperitoneal perfusion chemotherapy (HIPPC).
Materials and Methods
Sixty-two patients with malignant ascites induced by gastrointestinal or ovarian cancer were divided into two groups to receive either B-ultrasound-guided or laparoscopically-assisted HIPPC. Clinical efficacy was assessed from the objective remission rate (ORR), the Karnofsky Performance Status (KPS) score, and overall survival. The incidence of port-site metastasis was compared between the two groups.
Results
Patients in the B-ultrasound (n=32) and laparoscopy (n=30) groups were comparable in terms of age, sex, primary disease type, volume of ascites, and free cancer cell (FCC)-positive ascites. After HIPPC, there were no significant differences between the B-ultrasound and laparoscopy groups in the KPS score change, ORR, and median survival time. The incidence of port-site metastasis after HIPPC was not significantly different between the B-ultrasound (3 of 32, 9.36%) and laparoscopy (3 of 30, 10%) groups, but significantly different among pancreatic, gastric, ovarian, and colorectal cancer (33.33, 15.79, 10.00, and 0.00%, p<0.001).
Conclusion
The chimney effect may not be the key reason for port-site metastasis after laparoscopy. Other factors may play a role, including the local microenvironment at the trocar site and the delivery of viable FCCs (from the tumor or malignant ascites) to the trauma site during laparoscopic surgery.
Laparoscopic surgery is widely used for the treatment of a variety of benign disorders, such as gallbladder stones and inguinal hernia, and the advantages of this minimally invasive technique include less pain, quicker recovery, and shorter hospitalization time.12 In recent years, it has been proposed that laparoscopic procedures may also be a safe alternative to open surgery for the treatment of malignant diseases.345 However, concerns have been raised in light of numerous case reports documenting port-site recurrences after diagnostic laparoscopy or laparoscopic resection in patients with malignancies,678910 and these concerns have limited the use of laparoscopic techniques for the resection of intra-abdominal malignancies. Therefore, further studies of the factors contributing to port-site metastasis are needed to overcome this serious problem.11121314
The development of port-site metastases after laparoscopic surgery is likely multifactorial.15161718 One factor may be the leakage of CO2 along a trocar, the so-called “chimney effect." Initial experimental data suggested that cell aerosolization due to pneumoperitoneum and port-site contamination via the chimney effect may play a role.19202122 Several studies have shown that pneumoperitoneum increases the risk of port-site metastasis, compared to gasless laparoscopy.232425 Leakage around a trocar during laparoscopic procedures could result in a high local flow of free-floating tumor cells.26272829 Of course, leakage along trocar openings can be overcome simply by placing a purse-string suture around the trocar.13 However, the fact that a significantly higher incidence of port-site metastasis is observed at leakage sites than at intact purse-string sites suggests that leakage is not a major contributor to port-site metastases.13 Another factor that may increase the risk of tumor growth at the trocar site is local tissue trauma.16303132 The traumatized trocar wound appears to be a good medium for the implantation and growth of tumor cells, due to the abundance of growth factors in the traumatized tissue.121316303132 However, the presence of free viable tumor cells in the peritoneal cavity and transportation of these cells to the trocar wounds is required, and these hypotheses remain controversial. Although laparoscopic surgery causes less tissue trauma than open surgery, tumor recurrence in abdominal wounds has often been described after laparoscopy, whereas open surgery is associated with a lower incidence of tumor metastases at incision sites.67 This is difficult to explain based on the local tissue trauma theory alone. Clearly, the occurrence of tumor implantation and growth at port sites is a complex process involving many factors.
Hyperthermic intraperitoneal perfusion chemotherapy (HIPPC) has been shown to have good clinical efficacy for the treatment of peritoneal carcinomatosis.333435 Laparoscopically-assisted placement of perfusion tubes for HIPPC has also achieved satisfactory results in the treatment of malignant ascites not amenable to cytoreductive surgery.3334353637 On the basis of our successful experience using laparoscopically-assisted HIPPC,36 we have also achieved satisfactory outcomes using B-ultrasound-guided HIPPC for the treatment of malignant ascites secondary to gastric cancer (GC), colorectal cancer (CRC), ovarian cancer (OC), and pancreatic cancer (PC).3738 However, our study demonstrated that B-ultrasound-guided HIPPC could not avoid the problem of port-site metastasis, despite the fact that a CO2-pneumoperitoneum is not required for this technique. This implies that the chimney effect may be not a key factor underlying port-site metastasis.37
In one of our previous studies, we compared treatment outcomes (surgery duration, cost, efficacy, and quality of life) between B-ultrasound-guided and laparoscopically-assisted HIPPC.37 In the present study, we used the same cohort of patients to make a preliminary comparison of the incidence of port-site metastasis between B-ultrasound-guided HIPPC and laparoscopically-assisted HIPPC, in order to reveal whether CO2 leakage (the chimney effect) is a major factor causing port-site metastasis after laparoscopic surgery.
The participants were from a prospective study of patients with peritoneal carcinomatosis exhibiting malignant ascites, treated in the Cancer Hospital of Guangzhou Medical University, China between March 2007 and August 2014.37 All patients had confirmed primary tumors. Written informed consent was obtained from all patients. The study was approved by the Medical Ethics Committee of the Cancer Hospital of Guangzhou Medical University (No. GZCH 200825).
The inclusion criteria for enrollment in the study were as follows: 1) age ≥18 years; 2) peritoneal carcinomatosis originating from GC, OC, PC, or CRC and diagnosed via computed tomography (CT), magnetic resonance imaging, serum tumor biomarker examination, ascites cytology, and/or laparotomy; and 3) malignant ascites confirmed via B-ultrasound and/or CT. Patients satisfying any of the following criteria were excluded: 1) minimal or no malignant ascites; 2) limited encapsulation of intraperitoneal effusions; 3) extensive abdominal adhesions due to multiple previous operations; and 4) complete intestinal obstruction.
The included patients were divided into two groups using a computer-generated random number table: a B-ultrasound group (patients treated with B-ultrasound-guided HIPPC) and a laparoscopy group (patients treated with conventional laparoscopically-assisted HIPPC).
B-ultrasound guided placement of catheters for chemotherapy was performed as described previously.3637 Pethidine hydrochloride (75 mg) and promethazine hydrochloride (25 mg) were administered via intramuscular injection prior to placement of the HIPPC catheters, with the patient in a supine position. Intravenous propofol was administered continuously at 3–8 mL/h, according to patient status.
All four abdominal quadrants were examined using B-ultrasound to select an optimal single puncture point in the region with the most ascites yet without adherence between the ab-dominal wall and tissues of the peritoneal cavity and without any signs of tumor or previous abdominal incision. After local administration of 0.5% lidocaine (as an anesthetic agent), a 1.2-cm incision was made at the puncture point using a scalpel, and a Hasson trocar (1.2 cm in diameter) was inserted into the peritoneal cavity.
Outflow catheters with multiple side holes (inner diameter 0.8 cm, outer diameter 1.0 cm, length 100 cm) were placed in the left and right lower quadrants of the intraperitoneal cavity. Infusion catheters (internal length 40–80 cm) were positioned in the left and right upper quadrants of the intraperitoneal cavity. The perfusion catheters were fixed to the abdominal wall using cutaneous sutures (Fig. 1A). The ascitic fluid was extracted as completely as possible.
Laparoscopic examination and chemotherapeutic catheter placement were as described previously.3637 Briefly, patients were placed in a supine position, and following conventional endotracheal anesthesia, a 1.2-cm incision was made using a scalpel at the intersection of the left midclavicular line and the transverse line positioned approximately two finger-widths below the umbilicus. The ascitic fluid was extracted as completely as possible. An artificial pneumoperitoneum was established via a closed procedure with a pressure of 15 mm Hg (1 mm Hg=0.133 kPa), and a trocar (1.2 cm diameter) was inserted into the abdominal cavity via the working port. Subsequently, a laparoscope (10 mm and 30°) was inserted via the trocar to examine the abdominal viscera and tumors. The site, size, and clinical stage of the tumor were examined laparoscopically.
Three new ports were prepared under laparoscopic guidance. On the right side, the second and third ports (both 1.2 cm long) were prepared at the intersections of the midclavicular line and the transverse lines positioned approximately two finger-widths above and below the umbilicus, respectively. On the left side, the fourth port (1.2 cm long) was prepared at the intersection of the midclavicular line and the transverse line positioned approximately two finger-widths below the umbilicus. Subsequently, trocars (1.2 cm diameter) were inserted into the abdominal cavity via the incisions, under laparoscopic guidance.
Perfusion catheters were placed in the left and right superior abdominal cavities via the third and fourth working ports, respectively. One drainage catheter was placed in the Douglas cavity, the lowest region in the pelvic cavity, via the second working port. The laparoscope was then placed in the inferior abdomen, and the trocar inserted completely. The laparoscope was then removed, and the perfusion catheter was placed in the Douglas cavity using the trocar for guidance (Fig. 1B).
HIPPC was performed as described previously, using our self-developed Bao Rui-Tiqiangreguanzhu (BR-TRG)-II-type high-precision hyperthermic intraperitoneal perfusion treatment system.363738 Our system has a precision of ±0.15℃ for temperature control and ±5% for flow control and has been approved by the State Food Drug Administration of China (approval no. 2009-3260924). Notably, the device was coupled to an automatic cooling apparatus.
HIPPC therapy was conducted over three sessions. The first session was completed in the operating room under the original anesthesia, and post-placement of perfusion catheters, guided via B-ultrasound or laparoscopic assistance, was conducted on the same day. The second and third sessions were performed in the intensive care unit on consecutive days following the first session. A 0.9% saline solution (equivalent to the cavity volume, ≈3000 to 6500 mL) was added to the custom-made infusion bag and delivered via the infusion tubes over 90 min, at a flow rate of 450–600 mL/min. The in-flow temperature was 43°C, resulting in interior abdominal temperatures of 41.5–42.5°C. The hyperthermic intraperitoneal chemotherapeutic agents added to the perfusion fluid were: 1) cisplatin (50 mg/m2 of body surface) and doxorubicin (50 mg/m2 of body surface) for ascites originating from OC or 2) mitomycin-C (12.5 mg/m2 of body surface) for ascites originating from GC, PC, or CRC. The specified dosages were applied during all three HIPPC sessions.
Upon completion of the third session, the peritoneal perfusion liquid and ascites were drained, and the two infusion catheters and single outflow catheter were removed, with only a single outflow catheter retained for drainage on days 1–3. At 2 weeks after the final HIPPC, all patients underwent 4–6 cycles of systemic chemotherapy, according to the confirmed primary tumor type.
The following patient demographic and clinical characteristics were recorded: age, sex, origin of ascites (i.e., primary tumor type), volume of ascites, and the presence or absence of free cancer cells (FCCs) in the ascitic fluid. Treatment efficacy, postoperative complications, and incidence of port-site metastases were compared between the two groups by blinded observers. Patients were followed up for 21 months or until death. B-ultrasound or CT examinations were performed during follow-up at a frequency of at least once per month, and the amount of ascites and tumor progression were assessed at each examination. Clinical efficacy was divided into the following three grades, based on the modified World Health Organization criteria for efficacy assessment in malignant tumors:37 1) complete remission (CR), in which the ascites showed CR after a 4-week treatment; 2) partial remission (PR), in which the ascites was reduced by 50% after a 4-week treatment; and 3) no consequence (NC), in which the ascites was not obviously reduced or had increased after treatment. The objective remission rate (ORR) was determined as: ORR=CR+PR. Both the amount of ascites and survival time were assessed from patient follow-up examinations. The Karnofsky Performance Status (KPS) score was used as an indicator of functional impairment and prognosis. The detection and characterization of port-site metastases were achieved based on abdominal CT and histopathological and immunohistochemical examination of the resected tumor. If CT imaging detected nodules in previous trocar sites in the right or left quadrants of the abdominal wall or if the pathology of these masses revealed metastatic carcinoma with a degree of differentiation that was consistent with the primary tumor, immunohistochemistry was performed to confirm that these metastases were in fact from the primary tumor. These assessments were performed by blinded observers.
Data are presented as numbers and percentages, or as means±standard deviations. Comparisons of median survival between the B-ultrasound and laparoscopy groups, as well as between patients with different types of malignancy, were made using the Kaplan-Meier method and log-rank tests. Comparisons of quantitative data, including KPS scores, between the B-ultrasound and laparoscopy groups were conducted using Student's t-test. The chi-square test was used for comparisons of qualitative data, including the incidences of port-site metastases in the various groups. p values of less than 0.05 were considered to be statistically significant.
The characteristics of the study patients have been reported previously.37 A total of 62 patients with peritoneal carcinomatosis exhibiting malignant ascites (23 males and 39 females), with a median age of 51 years (ranging from 37 to 76 years), were enrolled. All patients had confirmed primary tumors, including GC (8 cases) or peritoneal carcinomatosis post-GC resection (11 cases), OC (10 cases) or peritoneal carcinomatosis from OC (10 cases), CRC (11 cases) or peritoneal carcinomatosis from CRC (9 cases), and PC (3 cases). All patients exhibited approximately 3000 to 6500 mL of ascites, measured after peritoneal drainage.
As reported previously,37 patients in both the B-ultrasound and laparoscopy groups did not differ significantly in terms of their demographic characteristics, primary disease types, volumes of ascites, and rates of FCC-positive ascites. The intraoperative course was uneventful in all patients in both treatment groups. No postoperative deaths or complications related to the HIPPC procedure were reported in either group.
As previously reported,37 clinical CR, PR, and NC were obtained in 84.38% (27 of 32), 9.38% (3 of 32), and 6.25% of patients (2 of 32), respectively, in the B-ultrasound group. The corresponding values in the laparoscopy group were 86.67% (26 of 30), 6.67% (2 of 30), and 6.67% (2 of 30), respectively. The ORR was 93.75% in the B-ultrasound group and 93.34% in the laparoscopy group (p>0.05), indicating that the clinical efficacy of the treatment was similar in the two groups (Table 1).
As previously reported,37 the mean KPS score in the B-ultrasound group increased significantly from 54.06 before treatment to 77.19 after HIPPC (p<0.001). Similarly, the mean KPS score in the laparoscopy group was significantly elevated from 54.09 before treatment to 76.73 after HIPPC (p<0.001). The change in KPS score was not significantly different between the two groups (23.13% vs. 22.64%, p>0.05), indicating that the two HIPPC procedures resulted in a similar improvement in patient quality of life.
All patients completed follow-up (up to 21 months or death). In the B-ultrasound group, 29 of 32 patients died, and survival times ranged from 2 to 30 months with a median survival of 9 months; the remaining three patients were still alive at the 21-month follow-up examination. In the laparoscopy group, 27 of 30 patients died, and survival times ranged from 2 to 20 months with a median survival of 8 months; the remaining three patients were still alive at 21 months. There were no significant differences in median survival time (9 months vs. 8 months) between the two treatment groups (p>0.05). Notably, patients with differing cancer types (PC, GC, OC, and CRC) had significantly different survival times (11 months vs. 6 months vs. 17 months vs. 9 months, p=0.01) (Table 2).
The overall incidence of port-site metastasis was 9.68% (6 of 62). The six patients with port-site metastasis exhibited subcutaneous nodules corresponding to the port site 1–3 months after surgery. CT showed a new subcutaneous mass around the abdominal port site (Fig. 2). The patients exhibiting port-site metastasis included one patient with GC whose ascites recurred 3 months after B-ultrasound-guided HIPPC (Fig. 3). In three patients, histological analysis of a transcutaneous biopsy of the port-site mass confirmed port-site metastasis and established that the pathological type and degree of tumor differentiation was the same as that of the primary tumor (Fig. 4). Tumor biomarker expression (carcinoembryonic antigen) of the port-site mass was shown via immunohistochemistry to be the same as that of the primary tumor (Fig. 5).
Port-site metastasis was found in three patients in each of the B-ultrasound and laparoscopy groups, and the incidence of port-site metastasis was not significantly different between the two groups (9.36% vs. 10.00%, p>0.05) (Table 2). In the laparoscopy group, the survival times of the three patients with port-site metastasis ranged from 2 to 7 months, with a median survival of 3 months. In the B-ultrasound group, the survival times of the three patients with port-site metastasis ranged from 3 to 6 months, with a median survival of 3 months. There was no significant difference between the two groups in terms of the median survival time (3 months vs. 3 months) of patients with port-site metastasis (p>0.05).
Notably, the rates of FCC-positive ascites differed significantly between the various primary cancer types (PC, 100.00%; GC, 78.95%; OC, 70.00%; CRC, 20.00%; p<0.05) (Table 2). The incidence of port-site metastasis also differed significantly between the various cancer types and correlated with the rate of FCC-positive ascites (PC, 33.33%; GC, 15.79%; OC, 10.00%; CRC, 0.00%; p<0.001) (Table 2). As might be expected, patient prognosis for the various cancer types correlated with the incidence of port-site metastasis and the rate of FCC-positive ascites, with the exception of OC (Table 2).
The use of HIPPC in the treatment of malignant ascites induced by peritoneal carcinomatosis has been reported to improve patient quality of life and prolong survival.333435 The main findings of our previous study were that the clinical efficacies of B-ultrasound-guided HIPPC and laparoscopically-assisted HIPPC, assessed from the ORR, KPS score, and overall survival, were comparable. In the present study, the incidence of port-site metastasis was found to be similar in the B-ultrasound and laparoscopy groups, although it varied depending on the primary tumor type. Taken together, these data indicate that B-ultrasound-guided HIPPC is a useful alternative to laparoscopically-assisted HIPPC.
The incidence of port-site metastasis after diagnostic laparoscopy or laparoscopic resection is difficult to establish.8911 Several review articles have described unacceptably high levels of more than 10%, while others have estimated the incidence to range from 3.3% to 5.3%.3032 In the present study, the incidence of port-site metastasis following B-ultrasound-guided and laparoscopically-assisted HIPPC was 9.68%, much higher than that reported previously in the literature. The high rate of FCC-positive ascites (58.10%) observed in the present study may be relevant to the high incidence of port-site metastasis. Viable FCCs in the peritoneal cavity and their transportation to the trocar wounds are key to port-site metastasis. The high level of viable tumor cells, possibly including tumor stem cells, in the ascitic fluid of the patients in our study may have contributed to the high incidence of port-site metastasis. Several investigations have shown that a deficient supply of blood and oxygen in ascites provides favorable conditions for the growth and survival of tumor stem cells.3940 Indeed, the presence of malignant ascites during and after surgery has been reported to increase the risk of port-site metastasis.12 Another reason may be that tumor cells in the ascitic fluid flow easily into the port site during the B-ultrasound-guided or laparoscopically-assisted placement of catheters for HIPPC. The delivery of FCCs to the trauma site may promote their implantation at the port site. Thus, one of the key factors underlying port-site metastasis may be the implantation of viable tumor cells (present in the ascitic fluid) in the trocar wounds during surgery. Allardyce, et al.14 found more tumor cells at operating ports than at assisting ports, implying that wound implantation was caused by contamination of the instruments. Meta-static growth at port sites used for specimen extraction suggests that contamination due to direct contact with the resected specimen may be responsible.17
There is evidence that a direct influence of CO2 on tumor growth is a key factor underlying port-site metastasis after laparoscopic surgery. Jacobi, et al.20 showed that insufflation of CO2 promoted tumor growth in a rat model when compared to helium or controls. Using a rat model of laparoscopy, Tseng, et al.13 also found enhanced tumor growth in a CO2 insufflation group compared to a gasless group. However, Hubens, et al.21 failed to demonstrate any effect of a CO2 pneumoperitoneum on tumor cell implantation or growth. The observation that a purse-string suture around the trocar can increase the incidence of port-site metastasis suggests that leakage contributes less to tumor growth than tissue trauma induced by the purse-string suture.13 A purse-string suture may itself induce tissue trauma that enhances tumor adherence and growth.13 In our study, the incidence of port-site metastasis was not significantly different between the B-ultrasound and laparoscopy groups. Given that a CO2 pneumoperitoneum is required for the latter yet not for the former, this suggests that the chimney effect may not be a major factor underlying the occurrence of port-site metastasis.
Several researchers have proposed that the microenvironment of the port site could be an important factor in tumor growth and that local factors at the port-site may play an important role in the mechanism of port-site metastasis.2032 A microenvironment conducive to cancer cell growth likely facilitates port-site metastasis, and tissue trauma and local peritoneal factors may be as important as cell aerosolization. Local peritoneal immunity has been recognized as having an important influence on cell anchorage and proliferation. The study of Tseng, et al.13 investigated the effects of tissue trauma and suggested that local peritoneal factors induced by the trocar could promote port-site metastasis. Paracentesis is an efficient technique for attenuating the symptoms induced by malignant ascites; although paracentesis tubes are much smaller than HIPPC catheters, our clinical experience is that metastasis to sites around the puncture holes is much more common after paracentesis than after laparoscopy-assisted HIPPC (data not shown). In the current study, B-ultrasound-guided HIPPC and laparoscopy-assisted HIPPC exhibited a comparable incidence of port-site metastasis; both techniques used 1.2-cm incisions and a 1.2-cm diameter trocar. Thus, we believe that the microenvironment around the trocar sites may promote the implantation of tumor cells at the port sites.
Cancers differ in their malignant potential and ability to metastasize. Therefore, the incidence of port-site metastasis would also be expected to vary between different types of tumors. In this study, the incidence of post-HIPPC port-site metastasis differed between the various primary tumor types and correlated with the rate of FCC-positive ascites that was observed for the various cancer types. These observations indicate that the incidence of port-site metastasis for different tumor types parallels the incidence of FCC-positive ascites, suggesting that these tumors vary in their ability to metastasize to port sites.
Our study is not without its limitations. The current study enrolled a relatively small patient cohort that may not be representative of the general patient population; additional investigations in larger cohorts are thus required. Furthermore, although the presence of FCCs in ascitic fluid appeared to correlate with port-site metastasis, this association was not specifically investigated (for example, with regression analysis). Additionally, the roles of other factors, such as the microenvironment at the trocar site, were not assessed in any detail.
In conclusion, CO2 leakage around the trocar (chimney effect) caused by an artificial pneumoperitoneum during laparoscopic surgery may not be a key mechanism underlying port-site metastasis. The delivery of FCCs from the tumor or malignant ascites to the site of trauma, as well as the local microenvironment at the trocar site, may promote the implantation of tumor cells at port sites.
Figures and Tables
 | Fig. 1Placement sites for the infusion and outflow catheters, for B-ultrasound-guided HIPPC (A) and laparoscopically-assisted HIPPC (B). a mark the two infusion catheters, b mark the two outflow catheters, and the white clips mark the loop circuit for HIPPC preparation. HIPPC, hyperthermic intraperitoneal perfusion chemotherapy. |
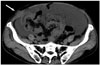 | Fig. 3Abdominal CT scan (axial) in a patient with gastric cancer exhibiting port-site metastasis (arrow) and recurrence of ascites 3 months after B-ultrasound-guided hyperthermic intraperitoneal perfusion chemotherapy. |
 | Fig. 4Histopathological examination of a resected tumor (hematoxylin and eosin staining, ×400). The metastatic nodule resected from the abdominal wall was a well-differentiated adenocarcinoma; the pathological type and degree of differentiation were the same as those of the primary tumor. |
 | Fig. 5Immunohistochemical assessment of a metastatic nodule in the abdominal wall (hematoxylin and eosin staining, ×100). The carcinoembryonic antigen expression of the metastatic nodule was the same as that of the primary tumor. |
Table 1
Comparison of Clinical Efficacy in Patients with Malignant Ascites Treated with B-Ultrasound-Guided or Laparoscopically-Assisted HIPPC

Table 2
Comparison of the Incidence of Port-Site Metastasis between Different Tumor Types

ACKNOWLEDGEMENTS
This study was supported by the Breakthroughs in Key Areas of Guangdong and Hong Kong Projects (No. 2006Z1-E6041), and by the Guangdong Provincial Science and Technological Programs (No. 2009A030301013).
References
1. Holloway RW, Ahmad S, DeNardis SA, Peterson LB, Sultana N, Bigsby GE 4th, et al. Robotic-assisted laparoscopic hysterectomy and lymphadenectomy for endometrial cancer: analysis of surgical performance. Gynecol Oncol. 2009; 115:447–452.

2. Young-Fadok T, Talac R, Nelson H. Laparoscopic colectomy for cancer; the need for trials. Semin Colon Rectal Surg. 1999; 19:94–101.
3. Kim JW, Kim WS, Cheong JH, Hyung WJ, Choi SH, Noh SH. Safety and efficacy of fast-track surgery in laparoscopic distal gastrectomy for gastric cancer: a randomized clinical trial. World J Surg. 2012; 36:2879–2887.

4. Fagotti A, Vizzielli G, Costantini B, Lecca A, Gallotta V, Gagliardi ML, et al. Learning curve and pitfalls of a laparoscopic score to describe peritoneal carcinosis in advanced ovarian cancer. Acta Obstet Gynecol Scand. 2011; 90:1126–1131.

5. Lanowska M, Mangler M, Spek A, Grittner U, Hasenbein K, Chiantera V, et al. Radical vaginal trachelectomy (RVT) combined with laparoscopic lymphadenectomy: prospective study of 225 patients with early-stage cervical cancer. Int J Gynecol Cancer. 2011; 21:1458–1464.

6. Curet MJ, Putrakul K, Pitcher DE, Josloff RK, Zucker KA. Laparoscopically assisted colon resection for colon carcinoma: perioperative results and long-term outcome. Surg Endosc. 2000; 14:1062–1066.

7. Zmora O, Weiss EG. Trocar site recurrence in laparoscopic surgery for colorectal cancer. Myth or real concern? Surg Oncol Clin N Am. 2001; 10:625–638.
8. Berretta R, Rolla M, Patrelli TS, Gramellini D, Fadda GM, Nardelli GB. Incidence of port-site metastasis after laparoscopic management of borderline ovarian tumors: a series of 22 patients. Eur J Gynaecol Oncol. 2009; 30:300–302.
9. Zivanovic O, Sonoda Y, Diaz JP, Levine DA, Brown CL, Chi DS, et al. The rate of port-site metastases after 2251 laparoscopic procedures in women with underlying malignant disease. Gynecol Oncol. 2008; 111:431–437.

10. Eng MK, Katz MH, Bernstein AJ, Shikanov S, Shalhav AL, Zorn KC. Laparoscopic port-site metastasis in urologic surgery. J Endourol. 2008; 22:1581–1585.

11. Kruitwagen RF, Swinkels BM, Keyser KG, Doesburg WH, Schijf CP. Incidence and effect on survival of abdominal wall metastases at trocar or puncture sites following laparoscopy or paracentesis in women with ovarian cancer. Gynecol Oncol. 1996; 60:233–237.

12. Agostini A, Robin F, Aggerbeck M, Jaïs JP, Blanc B, Lécuru F. Influence of peritoneal factors on port-site metastases in a xenograft ovarian cancer model. BJOG. 2001; 108:809–812.

13. Tseng LN, Berends FJ, Wittich P, Bouvy ND, Marquet RL, Kazemier G, et al. Port-site metastases. Impact of local tissue trauma and gas leakage. Surg Endosc. 1998; 12:1377–1380.
14. Allardyce RA, Morreau P, Bagshaw PF. Operative factors affecting tumor cell distribution following laparoscopic colectomy in a porcine model. Dis Colon Rectum. 1997; 40:939–945.

15. Ziprin P, Ridgway PF, Peck DH, Darzi AW. The theories and realities of port-site metastases: a critical appraisal. J Am Coll Surg. 2002; 195:395–408.
16. Wang PH, Yuan CC, Lin G, Ng HT, Chao HT. Risk factors contributing to early occurrence of port site metastases of laparoscopic surgery for malignancy. Gynecol Oncol. 1999; 72:38–44.

17. Whelan RL, Lee SW. Review of investigations regarding the etiology of port site tumor recurrence. J Laparoendosc Adv Surg Tech A. 1999; 9:1–16.

18. Iwanaka T, Arya G, Ziegler MM. Mechanism and prevention of port-site tumor recurrence after laparoscopy in a murine model. J Pediatr Surg. 1998; 33:457–461.

19. Hewett PJ, Thomas WM, King G, Eaton M. Intraperitoneal cell movement during abdominal carbon dioxide insufflation and laparoscopy. An in vivo model. Dis Colon Rectum. 1996; 39:10 Suppl. S62–S66.
20. Jacobi CA, Sabat R, Böhm B, Zieren HU, Volk HD, Mûller JM. Pneumoperitoneum with carbon dioxide stimulates growth of malignant colonic cells. Surgery. 1997; 121:72–78.

21. Hubens G, Pauwels M, Hubens A, Vermeulen P, Van Marck E, Eyskens E. The influence of a pneumoperitoneum on the peritoneal implantation of free intraperitoneal colon cancer cells. Surg Endosc. 1996; 10:809–812.

22. Canis M, Botchorishvili R, Wattiez A, Mage G, Pouly JL, Bruhat MA. Tumor growth and dissemination after laparotomy and CO2 pneumoperitoneum: a rat ovarian cancer model. Obstet Gynecol. 1998; 92:104–108.

23. Mathew G, Watson DI, Rofe AM, Ellis T, Jamieson GG. Adverse impact of pneumoperitoneum on intraperitoneal implantation and growth of tumour cell suspension in an experimental model. Aust N Z J Surg. 1997; 67:289–292.

24. Gutt CN, Riemer V, Kim ZG, Jacobi CA, Paolucci V, Lorenz M. Impact of laparoscopic colonic resection on tumour growth and spread in an experimental model. Br J Surg. 1999; 86:1180–1184.

25. Allendorf JD, Bessler M, Kayton ML, Oesterling SD, Treat MR, Nowygrod R, et al. Increased tumor establishment and growth after laparotomy vs laparoscopy in a murine model. Arch Surg. 1995; 130:649–653.

26. Yamaguchi K, Hirabayashi Y, Shiromizu A, Shiraishi N, Adachi Y, Kitano S. Enhancement of port site metastasis by hyaluronic acid under CO2 pneumoperitoneum in a murine model. Surg Endosc. 2001; 15:504–507.

27. Watson DI, Mathew G, Ellis T, Baigrie CF, Rofe AM, Jamieson GG. Gasless laparoscopy may reduce the risk of port-site metastases following laparascopic tumor surgery. Arch Surg. 1997; 132:166–168.

28. Bouvy ND, Giuffrida MC, Tseng LN, Steyerberg EW, Marquet RL, Jeekel H, et al. Effects of carbon dioxide pneumoperitoneum, air pneumoperitoneum, and gasless laparoscopy on body weight and tumor growth. Arch Surg. 1998; 133:652–656.

29. Bouvy ND, Marquet RL, Jeekel H, Bonjer HJ. Impact of gas(less) laparoscopy and laparotomy on peritoneal tumor growth and abdominal wall metastases. Ann Surg. 1996; 224:694–700.

30. Murthy SM, Goldschmidt RA, Rao LN, Ammirati M, Buchmann T, Scanlon EF. The influence of surgical trauma on experimental metastasis. Cancer. 1989; 64:2035–2044.

31. Little D, Regan M, Keane RM, Bouchier-Hayes D. Perioperative immune modulation. Surgery. 1993; 114:87–91.
32. Sporn MB, Roberts AB. Peptide growth factors and inflammation, tissue repair, and cancer. J Clin Invest. 1986; 78:329–332.

33. Facchiano E, Scaringi S, Kianmanesh R, Sabate JM, Castel B, Flamant Y, et al. Laparoscopic hyperthermic intraperitoneal chemotherapy (HIPEC) for the treatment of malignant ascites secondary to unresectable peritoneal carcinomatosis from advanced gastric cancer. Eur J Surg Oncol. 2008; 34:154–158.

34. Garofalo A, Valle M, Garcia J, Sugarbaker PH. Laparoscopic intraperitoneal hyperthermic chemotherapy for palliation of debilitating malignant ascites. Eur J Surg Oncol. 2006; 32:682–685.

35. Valle M, Van der Speeten K, Garofalo A. Laparoscopic hyperthermic intraperitoneal peroperative chemotherapy (HIPEC) in the management of refractory malignant ascites: a multi-institutional retrospective analysis in 52 patients. J Surg Oncol. 2009; 100:331–334.

36. Ba MC, Cui SZ, Lin SQ, Tang YQ, Wu YB, Wang B, et al. Chemotherapy with laparoscope-assisted continuous circulatory hyperthermic intraperitoneal perfusion for malignant ascites. World J Gastroenterol. 2010; 16:1901–1907.

37. Ba MC, Long H, Cui SZ, Tang YQ, Wu YB, Zhang XL, et al. Multivariate comparison of B-ultrasound guided and laparoscopic continuous circulatory hyperthermic intraperitoneal perfusion chemotherapy for malignant ascites. Surg Endosc. 2013; 27:2735–2743.

38. Cui S, Ba M, Tang Y, Liu J, Wu Y, Wang B, et al. B ultrasound-guided hyperthermic intraperitoneal perfusion chemotherapy for the treatment of malignant ascites. Oncol Rep. 2012; 28:1325–1331.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download