Abstract
Purpose
To evaluate the effects of sex and anthropometry on clinical outcomes in patients who underwent percutaneous coronary intervention (PCI).
Materials and Methods
From three randomized trials (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation, Impact of intraVascular UltraSound guidance on outcomes of Xience Prime stents in Long lesions, Chronic Total Occlusion InterVention with drUg-eluting Stents), we compared 333 pairs of men and women matched by propensity scores, all of whom underwent intravascular ultrasound (IVUS)-guided PCI for complex lesions.
Results
For 12 months, the incidence of adverse cardiac events, defined as the composite of cardiac death, target lesion–related myocardial infarction, and target lesion revascularization, was not different between women and men (2.4% vs. 2.4%, p=0.939). Using multivariable Cox's regression analysis, post-intervention minimum lumen area [MLA; hazard ratio (HR)=0.620, 95% confidence interval (CI)=0.423–0.909, p=0.014] by IVUS was a predictor of adverse cardiac events. Height on anthropometry and lesions with chronic total occlusion were significantly related to post-intervention MLA. However, female sex was not independently associated with post-intervention MLA. In an age and sex-adjusted model, patients in the low tertile of height exhibited a greater risk for adverse cardiac events than those in the high tertile of height (HR=6.391, 95% CI=1.160–35.206, p=0.033).
Women tend to experience worse clinical outcomes than men after undergoing contemporary interventional therapies.123 Poorer clinical outcomes in women may be because women have higher risk profiles for delayed onset of disease, older age, smaller body surface area, and comorbidities at the time of clinical presentation of coronary artery disease.123 In addition, women reportedly exhibit higher procedural risk than men according to the National Cardiovascular Data Registry4 and a lower revascularization rate of lesions with chronic total occlusion (CTO) after coronary artery bypass graft surgery, based on the Canadian Multicenter CTO Registry.5 However, other studies have shown that after adjusting for confounding risk factors, sex-specific risk was limited, and adjusted rates of adverse cardiac events, including long-term mortality and revascularization, were similar between women and men.123 Accordingly, although sex differences may exist in a high-risk subset of coronary artery disease patients, sex-specific clinical outcomes have not been well established, partly because of the small sample of women in prospective trials.
Compared to men, women have smaller vessels,678 and a smaller target vessel size has been shown to be associated with a greater likelihood of target lesion revascularization.9 Meanwhile, however, women reportedly show a similar rate of target lesion revascularization after stent implantation, compared to men, despite smaller vessel sizes.1 Although differences in body size and clinical risk factors may explain this paradoxical finding, detailed associations among sex, anthropometric measurements, and procedural/clinical outcomes after percutaneous coronary intervention (PCI) have not yet been established.
In this study, we sought to investigate the effects of sex and anthropometric measurements on clinical outcomes after next-generation drug-eluting stent (DES) implantation for complex coronary lesions with long stenosis or CTO using intravascular ultrasound (IVUS).
Patients were identified from three randomized trials: REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation (RESET),1011 Impact of intraVascular UltraSound guidance on outcomes of Xience Prime stents in Long lesions (IVUS-XPL),12 and Chronic Total Occlusion InterVention with drUg-eluting Stents (CTO-IVUS).13 Unique identifiers of Clinical Trial Registration-URL: http://www.clinicaltrials.gov were as follows: NCT01145079 for RESET, NCT01308281 for IVUS-XPL, and NCT01563952 for CTO-IVUS. Briefly, the RESET trial tested the non-inferiority of 3-month dual antiplatelet therapy following Endeavor sprint zotarolimus-eluting stent (Medtronic Inc., Santa Rosa, CA, USA) implantation, compared with 12-month dual antiplatelet therapy after implantation of another available DES. In the pre-specified long lesion subset of this study, 543 patients were randomly assigned to either IVUS- or angiography-guided DES implantation groups.11 The IVUS-XPL trial investigated the usefulness of IVUS guidance during everolimus-eluting stent (Xience prime, Abbott Vascular, Santa Clara, CA, USA) implantation for long coronary lesions. A total of 1400 patients were randomly assigned to receive either IVUS- or angiography-guided stent implantation. The CTO-IVUS trial was undertaken to test the hypothesis that IVUS-guided CTO intervention would be superior to angiography-guided intervention. Four hundred two patients with CTO lesions were randomized to either IVUS- or angiography-guided intervention. Detailed protocols of these trials have been published previously.10111213 The study protocols of these trials were approved by the Institutional Review Board of each participating institution, and written consent was obtained from all patients.
Of 1129 patients (333 women and 796 men) who underwent IVUS-guided intervention, women were older than men. In addition, there were significant differences in the frequencies of hypertension, dyslipidemia, current smoking, multi-vessel disease, and CTO lesions between women and men (Supplementary Table 1, only online). Accordingly, we performed propensity score matching to adjust for significant differences in clinical and angiographic characteristics in the women and men. After matching propensity scores for 333 women and 796 men, 333 matched pairs were selected for analysis.
Next-generation DESs composed of everolimus-, zotarolimus-, and biolimus-eluting stents were implanted according to standard techniques. If a lesion could not be covered with a single stent, overlapping stents were used. Stent diameter and length were based on online IVUS measurements. Adjunct high-pressure dilation was performed at the discretion of the operators, based on the IVUS findings. Although IVUS could be performed at any step of DES implantation, post-intervention IVUS examination was mandatory.111213 One of two commercially available IVUS systems [Atlantis or I-Lab (Boston Scientific Corp/SCIMED, Minneapolis, MN, USA) or Eagle Eye (Volcano Therapeutics, Rancho Cordova, CA, USA)] was used.
Pre-PCI, all patients received at least 75 mg of aspirin. A loading dose of 300 mg of clopidogrel was administered at least 12 hours pre-PCI.10111213 However, if the loading dose of clopidogrel was not administered 12 hours in advance, the patient received a 600 mg loading dose of clopidogrel in the catheterization laboratory prior to PCI.101112 Unfractionated heparin was administered to maintain an activated clotting time >250 seconds. Use of glycoprotein IIb/IIIa inhibitors was left to the operator's discretion. After stent implantation, aspirin (100 mg, daily) was prescribed indefinitely; the duration of clopidogrel administration (75 mg, daily) depended on the randomized assignments in the RESET and IVUS-XPL trials.1112 In the CTO-IVUS trial, clopidogrel was used for at least 12 months.13
At the time of the index procedure, height and body weight were measured using a digital scale in all patients. Body surface area (m2) was calculated using the Mosteller formula: √[weight (kg)×height (cm)/3600],14 and body mass index (kg/m2) was calculated from the following formula: weight (kg)/[height (m)]2. Lean body mass (kg) was calculated using the James formula as follows: [1.1×weight (kg)]-{128×[weight (kg)/height (cm)]2} for men; [1.07×weight (kg)]-{148×[weight (kg)/height (cm)]2} for women.15 Fat mass (kg) was calculated as lean body mass subtracted from body weight.
Angiographic and IVUS measurements were performed by analysts who were blinded to patient information and treatment assignments in an independent core laboratory at the Cardiovascular Research Center, Seoul, Korea. Quantitative coronary angiography analysis was performed using an off-line quantitative coronary angiographic system [Cardiovascular Angiographic Analysis System (CAAS), Pie Medical Instruments, Maastricht, the Netherlands]. Using a guiding catheter for magnification-calibration, the diameters of reference vessels (the average of the proximal and distal reference lumen diameters), the minimal luminal diameter, and the percent diameter stenosis were measured before and after DES implantation from diastolic frames in a single, matched view showing the smallest minimal luminal diameter.
Standardized planimetry of the lumen, stent, and vessel cross-sectional area was performed using planimetry software (Echoplaque, INDEC Systems, Santa Clara, CA, USA) in accordance with the IVUS guidelines of the American College of Cardiology.16 Target lesions and both proximal and distal reference segments were assessed quantitatively. The post-intervention target lesion site was the image slice with the minimal lumen area (MLA). Proximal and distal reference segments were the most normal-looking segments within 5 mm proximal and distal to the target lesion.
Post-PCI clinical assessments were performed in-hospital and at 1, 3, 6, and 12 months after discharge either by clinic visit or telephone interview. Clinical events were defined according to the Academic Research Consortium.17 All deaths were considered cardiac deaths unless a definite non-cardiac cause could be established.17 Target lesion-related myocardial infarction during the 1-year follow-up after hospital discharge was defined as the presence of clinical symptoms, electrocardiographic changes, or abnormal imaging findings of myocardial infarction, combined with an increase in the creatine kinase myocardial band fraction above the upper normal limits or an increase in troponin-T/troponin-I to greater than the 99th percentile of the upper normal limit. The territory of the myocardial infarction was supplied by the coronary artery containing the stented lesions.1217 Ischemia-driven target lesion revascularization was defined as a repeat PCI or bypass surgery of the target lesion with either of the following: 1) angiographic diameter stenosis ≥50% by quantitative coronary angiographic analysis with documented evidence of a positive stress test or 2) angiographic diameter stenosis ≥70% irrespective of documented evidence of a positive stress test.17
Statistical analysis was performed using SPSS (version 18.0.0, SPSS Inc., Chicago, IL, USA) and R (version 2.8.0, R Foundation for Statistical Computing, Vienna, Austria) software. Propensity scores were estimated by fitting a logistic regression model using the following variables for women and men: age, hypertension, diabetes mellitus, dyslipidemia, current smoking, clinical presentation of acute myocardial infarction, angiographic multi-vessel disease, and lesions with CTO. Propensity score matching was performed using nearest neighbor matching without calipers. The Hansen and Bowers balance test p-value was 0.913, indicating good covariate balance. The C-statistic for the model was 0.567. Categorical variables are reported as numbers and percentages and were compared using the χ2 test or Fisher's exact test. Continuous variables are reported as means±standard deviations or medians (interquartile ranges). Differences between women and men were analyzed with Student's t test or the Mann-Whitney U test (if data were skewed), and those among the tertiles of patients' height were analyzed by one-way analysis of variance or the Kruskal-Wallis test (if data were skewed). Adverse cardiac events at 12 months were compared using Cox's regression analysis stratified by enrolled trials. To determine independent predictors of adverse cardiac events, multivariable Cox's regression analysis with a stepwise method was performed and stratified by trials. Multivariable linear regression model using a stepwise method was applied to evaluate associations between anthropometric measurements and post-intervention MLA as assessed by IVUS. All p-values were two-sided, and a p-value <0.05 was considered statistically significant.
Table 1 shows the clinical, procedural, and IVUS characteristics of the 666 patients who were matched by propensity scores. Compared to men, women were shorter in stature, weighed less, and had a smaller body surface area and lower lean body mass. Fat mass, however, was greater in women than in men. Body mass index was not different between women and men. Pre- and post-intervention reference vessel diameters by quantitative coronary angiographic analysis were smaller in women. In post-intervention IVUS analysis, MLA at the target lesions, as well as the lumen and external reference membrane area at the proximal and distal reference segments, were also significantly smaller in women than men.
PCI-related outcomes at 12 months are shown in Table 2. The incidence of adverse cardiac events, including cardiac death, target lesion-related myocardial infarction, and ischemia-driven target lesion revascularization, was not significantly different between women and men. The only significant predictor of adverse cardiac events was post-intervention MLA by IVUS [hazard ratio (HR)=0.620, 95% confidence interval (CI)=0.423–0.909, p=0.014], not female sex (Supplementary Table 2 and 3, only online).
Fig. 1 shows the associations between anthropometric measurements and post-intervention MLA evaluated by IVUS. While height, weight, body surface area, and lean body mass were significantly associated with post-intervention MLA, body mass index, and fat mass were not. The final multivariable linear regression analysis revealed that height (coefficient=0.041, 95% CI=0.025–0.057, p<0.001) and CTO lesions (coefficient=-0.622, 95% CI=-1.077–-0.167, p=0.008) were independently associated with post-intervention MLA as assessed by IVUS (Supplementary Table 4, only online).
Clinical, procedural, and IVUS characteristics were compared according to tertiles of patient height, as shown in Table 3. Compared to the intermediate or high tertile patients, those in the low tertile of height were older and mostly female. Although their weight, body surface area, and lean body mass were the smallest, patients in the low tertile of height had a greater body mass index and fat mass than intermediate or high tertile patients. Post-intervention IVUS showed that the external elastic membrane and lumen area of the reference segment, as well as a MLA of target lesions, were smallest in patients in the low tertile of height. In an adjusted (age and sex) model, patients in the low tertile of height were at greater risk for adverse cardiac events at 12 months than those in the high tertile of height (HR=6.391, 95% CI=1.160–35.206, p=0.033) (Fig. 2).
In this IVUS study, sex was not independently associated with adverse cardiac events at 12 months after next-generation DES implantation for lesions with long stenosis or CTO. After next-generation DES implantation, the only significant predictor of adverse cardiac events was post-intervention MLA as evaluated by IVUS. Although women had smaller-sized reference vessels and post-intervention MLA than men, independent factors that affected post-intervention MLA were height and CTO lesions. Compared to patients in the high tertile of height, those in the low tertile of height were at greater risk of adverse cardiac events at 12 months.
Compared to men, women have smaller coronary arteries, regardless of body surface area.678 These findings were based on angiography and autopsy,67 and a previous IVUS study also demonstrated the presence of these characteristics, explaining the increased susceptibility of women to vessel occlusion.8 However, despite the intrinsic effect of sex on coronary dimensions, little is known about sex differences in clinical outcomes, such as mortality or target lesion revascularization.123 In the present study, we evaluated complex lesions based on the hypothesis that adverse cardiac events could differ significantly in incidence between males and females. Similar to previous studies,678 we found that the vessel size of lesions with long stenosis or CTO was smaller in women than in men, and this feature of women was consequently associated with a smaller post-intervention MLA of the target lesion. However, sex was not associated with adverse clinical outcomes at 12 months post-intervention, and furthermore, its associations with post-intervention MLA were attenuated after adjusting for anthropometric variables. Accordingly, our results suggest that there is no sex-specific risk for procedural or clinical outcomes in coronary artery disease patients with complex lesions.
Previous cohort studies have consistently shown that overweight or obese patients with coronary artery disease exhibit better survival and lower cardiovascular events than normal weight patients.181920 However, it is controversial whether this obesity paradox is a real phenomenon, and the mechanisms responsible for this reversed association are still unknown.181920 Recently, an IVUS study suggested that a high body mass index was associated with a larger post-intervention stent area.21 However, confounders were not fully adjusted for, and other anthropometric variables, with the exception of body mass index, were not evaluated.21 In the present study, height, weight, body surface area, and lean body mass were associated with post-intervention MLA; body mass index and fat mass were not. Thus, tall and heavier patients might have a larger MLA after PCI than short and relatively thin patients, despite similar body mass indexes. Because height and weight contribute to body mass index in opposite ways, the lack of association between body mass index and post-intervention MLA suggests that a more important determinant of cardiovascular risk based on body mass index may be height, rather than weight.22 In addition, the present study suggests that body mass index does not reflect obesity accurately, because it did not differentiate lean mass from body fat. This finding is consistent with the suggestion of a previous study,18 and raises the question of whether body mass index is truly associated with cardiovascular events. Most previous studies have only used body mass index as a measure of obesity.18
Among the anthropometric variables measured in this study, height was most closely correlated to post-intervention MLA, and patients with a short stature tended to have more adverse events after PCI than taller patients. Although negative and even controversial studies have been published, a meta-analysis and two large population-based studies have shown an inverse association between height and coronary artery disease.232425 In the meta-analysis, the mean relative risk of cardiovascular morbidity and mortality was 1.46 in individuals in the shortest height category, compared to those in the tallest category, regardless of sex.23 Although the mechanisms underlying this inverse association are unclear, a large study recently demonstrated a significant association between height-associated single nucleotide polymorphisms and coronary artery disease.26 This link was partly explained by the association between shorter height and adverse lipid profiles.26 In addition to biological mechanisms, the theory of coronary vessel caliber may explain the inverse association between height and coronary artery disease. In the Coronary Artery Surgery Study (CASS), surgical mortality was inversely associated with the average diameter of the grafted coronary arteries in both men and women.27 Similarly, the present study showed a close relationship between height and post-intervention MLA that was a predictor for future adverse cardiac events.
Our study may have been underpowered to compare the effects of sex and anthropometric measurements on PCI outcomes because of the small sample size. Especially, the events of cardiac death or myocardial infarction rarely occurred, thus limiting the effects of sex on these outcomes. Because patients were drawn from the Korean population, the findings may not be generalizable to other ethnic groups. However, similar tendencies to those observed in other ethnic groups regarding PCI outcomes and the obesity paradox have been reported in the Korean population.282930 Lean body mass was not actually measured. Finally, the included trials' heterogeneity, such as inclusion/exclusion criteria and treatment strategies, may potentially affect the present results.
Sex was not found to be associated with post-intervention MLA as evaluated by IVUS and 12-month adverse cardiac events after next-generation DES implantation for lesions with long stenosis or CTO. However, height independently affected the post-intervention MLA of complex target lesions, and short stature may be associated with worse outcomes after PCI.
Figures and Tables
 | Fig. 1Associations among anthropometric measurements and post-intervention minimum lumen area (MLA) as evaluated by intravascular ultrasound. While height, weight, body surface area, and lean body mass were significantly associated with post-intervention MLA, body mass index and fat mass were not. Black dots indicate women and white dots indicate men. |
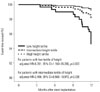 | Fig. 2Adjusted event-free survival curve for the composite of cardiac death, target lesion–related myocardial infarction, and ischemia-driven target lesion revascularization, grouped by height tertile. The adjustment included age and sex, and the adjusted hazard ratio (HR) was relative to patients in the high tertile of height. CI, confidence interval. |
Table 1
Baseline, Procedural, and IVUS Characteristics by Sex

Table 2
Adverse Cardiac Events at 12 Months

Table 3
Baseline, Procedural, and IVUS Characteristics According to Height Tertile

ACKNOWLEDGEMENTS
This study was supported by a grant from the Korea Healthcare Technology Research & Development Project, Ministry for Health & Welfare, Republic of Korea (Nos. A085136 and HI15C1277), the Mid-career Researcher Program through NRF grant funded by the MEST, Republic of Korea (No. 2015R1A2A2A01002731), and the Cardiovascular Research Center, Seoul, Korea.
References
1. Lansky AJ, Hochman JS, Ward PA, Mintz GS, Fabunmi R, Berger PB, et al. Percutaneous coronary intervention and adjunctive pharmacotherapy in women: a statement for healthcare professionals from the American Heart Association. Circulation. 2005; 111:940–953.

2. Singh M, Rihal CS, Gersh BJ, Roger VL, Bell MR, Lennon RJ, et al. Mortality differences between men and women after percutaneous coronary interventions. A 25-year, single-center experience. J Am Coll Cardiol. 2008; 51:2313–2320.

3. Berger JS, Elliott L, Gallup D, Roe M, Granger CB, Armstrong PW, et al. Sex differences in mortality following acute coronary syndromes. JAMA. 2009; 302:874–882.

4. Anderson ML, Peterson ED, Brennan JM, Rao SV, Dai D, Anstrom KJ, et al. Short- and long-term outcomes of coronary stenting in women versus men: results from the National Cardiovascular Data Registry Centers for Medicare & Medicaid services cohort. Circulation. 2012; 126:2190–2199.

5. Wolff R, Fefer P, Knudtson ML, Cheema AN, Galbraith PD, Sparkes JD, et al. Gender differences in the prevalence and treatment of coronary chronic total occlusions. Catheter Cardiovasc Interv. 2016; 87:1063–1070.

6. Roberts CS, Roberts WC. Cross-sectional area of the proximal portions of the three major epicardial coronary arteries in 98 necropsy patients with different coronary events. Relationship to heart weight, age and sex. Circulation. 1980; 62:953–959.

7. Dodge JT Jr, Brown BG, Bolson EL, Dodge HT. Lumen diameter of normal human coronary arteries. Influence of age, sex, anatomic variation, and left ventricular hypertrophy or dilation. Circulation. 1992; 86:232–246.

8. Sheifer SE, Canos MR, Weinfurt KP, Arora UK, Mendelsohn FO, Gersh BJ, et al. Sex differences in coronary artery size assessed by intravascular ultrasound. Am Heart J. 2000; 139:649–653.

9. Elezi S, Dibra A, Mehilli J, Pache J, Wessely R, Schömig A, et al. Vessel size and outcome after coronary drug-eluting stent placement: results from a large cohort of patients treated with sirolimus- or paclitaxel-eluting stents. J Am Coll Cardiol. 2006; 48:1304–1309.
10. Kim BK, Hong MK, Shin DH, Nam CM, Kim JS, Ko YG, et al. A new strategy for discontinuation of dual antiplatelet therapy: the RESET Trial (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation). J Am Coll Cardiol. 2012; 60:1340–1348.
11. Kim JS, Kang TS, Mintz GS, Park BE, Shin DH, Kim BK, et al. Randomized comparison of clinical outcomes between intravascular ultrasound and angiography-guided drug-eluting stent implantation for long coronary artery stenoses. JACC Cardiovasc Interv. 2013; 6:369–376.

12. Hong SJ, Kim BK, Shin DH, Nam CM, Kim JS, Ko YG, et al. Effect of intravascular ultrasound-guided vs angiography-guided everolimus-eluting stent implantation: the IVUS-XPL randomized clinical trial. JAMA. 2015; 314:2155–2163.

13. Kim BK, Shin DH, Hong MK, Park HS, Rha SW, Mintz GS, et al. Clinical impact of intravascular ultrasound-guided chronic total occlusion intervention with zotarolimus-eluting versus biolimus-eluting stent implantation: randomized study. Circ Cardiovasc Interv. 2015; 8:e002592.
15. Hallynck TH, Soep HH, Thomis JA, Boelaert J, Daneels R, Dettli L. Should clearance be normalised to body surface or to lean body mass? Br J Clin Pharmacol. 1981; 11:523–526.

16. Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, et al. American college of cardiology clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound studies (IVUS). A report of the American college of cardiology task force on clinical expert consensus documents. J Am Coll Cardiol. 2001; 37:1478–1492.

17. Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007; 115:2344–2351.
18. Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006; 368:666–678.

19. Hastie CE, Padmanabhan S, Slack R, Pell AC, Oldroyd KG, Flapan AD, et al. Obesity paradox in a cohort of 4880 consecutive patients undergoing percutaneous coronary intervention. Eur Heart J. 2010; 31:222–226.

20. Lancefield T, Clark DJ, Andrianopoulos N, Brennan AL, Reid CM, Johns J, et al. Is there an obesity paradox after percutaneous coronary intervention in the contemporary era? An analysis from a multicenter Australian registry. JACC Cardiovasc Interv. 2010; 3:660–668.

21. Kang SJ, Mintz GS, Witzenbichler B, Metzger DC, Rinaldi MJ, Duffy PL, et al. Effect of obesity on coronary atherosclerosis and outcomes of percutaneous coronary intervention: grayscale and virtual histology intravascular ultrasound substudy of assessment of dual antiplatelet therapy with drug-eluting stents. Circ Cardiovasc Interv. 2014; 8:e001392.
22. Karhunen PJ, Meinander T. Coronary artery disease: complex association between height and CHD-size matters. Nat Rev Cardiol. 2015; 12:385–386.

23. Paajanen TA, Oksala NK, Kuukasjärvi P, Karhunen PJ. Short stature is associated with coronary heart disease: a systematic review of the literature and a meta-analysis. Eur Heart J. 2010; 31:1802–1809.

24. Emerging Risk Factors Collaboration. Adult height and the risk of cause-specific death and vascular morbidity in 1 million people: individual participant meta-analysis. Int J Epidemiol. 2012; 41:1419–1433.
25. Rosenberg MA, Lopez FL, Bůžková P, Adabag S, Chen LY, Sotoodehnia N, et al. Height and risk of sudden cardiac death: the atherosclerosis risk in communities and cardiovascular health studies. Ann Epidemiol. 2014; 24:174–179.e2.

26. Nelson CP, Hamby SE, Saleheen D, Hopewell JC, Zeng L, Assimes TL, et al. Genetically determined height and coronary artery disease. N Engl J Med. 2015; 372:1608–1618.

27. Fisher LD, Kennedy JW, Davis KB, Maynard C, Fritz JK, Kaiser G, et al. Association of sex, physical size, and operative mortality after coronary artery bypass in the Coronary Artery Surgery Study (CASS). J Thorac Cardiovasc Surg. 1982; 84:334–341.

28. Choi YJ, Kim JB, Cho SJ, Cho J, Sohn J, Cho SK, et al. Changes in the practice of coronary revascularization between 2006 and 2010 in the Republic of Korea. Yonsei Med J. 2015; 56:895–903.

SUPPLEMENTARY MATERIALS
Supplementary Table 2
Multivariable Cox's Regression Analysis to Find Predictors of Adverse Cardiac Events




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download