Abstract
Purpose
Traumatic events and adverse stressful experiences are major etiological factors in a wide variety of physical and mental disorders. Developing psychological instruments that can be easily administered and that have good psychometric properties have become an integral part for research and practice. This study investigated the reliability and validity of the Korean version of the Lifetime Stressor Checklist-Revised (LSC-R) in a consecutive sample of psychiatric outpatients. The LSC-R is a 30-item self-reporting questionnaire examining lifetime traumatic and non-traumatic stressors.
Materials and Methods
A final sample of 258 outpatients with anxiety or depressive disorders was recruited at the psychiatric department of a university-affiliated teaching hospital. Self-reported data included the Life Events Checklist (LEC), the Zung Self-Rating Depression and Anxiety Scales, and the Impact of Events Scale-Revised, in addition to the LSC-R. A convenience sample of 50 college students completed the LSC-R on two occasions separated by a three week-interval for test-retest reliability.
Results
Mean kappa for temporal stability was high (κ=0.651) and Cronbach alpha was moderate (α=0.724). Convergent validity was excellent with corresponding items on the LEC. Concurrent validity was good for symptoms of post-traumatic stress disorder, depression, and anxiety. An exploratory factor analysis revealed that 11 factors explained 64.3 % of the total variance.
The definition of traumatic events has changed over time. The Diagnostic and Statistical Manual for Mental Disorders-III-Revised (DSM-III-R),1 published in 1987, defined traumatic events as those happening “beyond normal human experiences.” However, subsequent epidemiological studies have consistently demonstrated that the vast majority of people have experienced traumatic events throughout their lifetime.23 Following DSM versions deleted this ambiguous and incorrect statement and established a more specific description of the trauma. The most recent DSM-5 definition involves an event that encompasses actual or threatened death, serious injury, sexual violence, or job-related repeated exposure.4
Experience of any traumatic event is the first consideration for diagnosis of posttraumatic stress disorder (PTSD), in which 15–25% of individuals therewith have experienced traumatic events.5 Meanwhile, other mental disorders can also occur after a traumatic experience, including depressive disorder, substance use disorders, anxiety disorders, eating disorders, somatization and conversion disorders, personality disorders, and psychosis. In each disease category, traumatic events are considered to be an etiological or at least a contributing factor.367891011
In addition to traumatic events defined in the DSM, there is a growing body of evidence that more broadly defined trauma, including adverse life experiences that can cause or contribute to later development of mental disorders and even physical illnesses. According to a large scale epidemiological study conducted in the United States, those who had an adverse childhood experience (ACE) had an increased risk of clinical disorders in adulthood. Alcohol use disorder, drug abuse, depression, and suicide attempts were 4–12 times higher in those with ACEs; smoking and sexually transmitted diseases were 2–4 times higher, and decreased physical activity and severe obesity were approximately 1.5 times more frequent.12 Surprisingly, ACEs were not only associated with mental and behavioral disorders, but also with increased risk for ischemic heart disease, cancer, chronic lung disease, and musculoskeletal disorders, especially in the case of lung cancer (3 times) and chronic obstructive pulmonary disease (2.6 times).121314 Moreover, there seems to a dose-dependent relationship between the number of lifetime adverse events and later development of mental or physical illnesses.1215
Taken together, screening for any negative or traumatic events experienced in the past at an early assessment phase is a crucial process at psychiatric and general medical facilities for diagnostic evaluation and treatment planning. To date, several instruments have been used for screening traumatic events and stressful events. One survey of 227 trauma experts revealed that a dozen self-report tools were being used for this purposes in clinical practice;16 however, only the Stressful Life Events Screening Questionnaire17 and the Traumatic Life Events Questionnaire18 had psychometric support at the time of the investigation. More recently, the Life Events Checklist (LEC) was added to the list.19 This precise scale was originally developed as an ancillary measure for screening potentially traumatic events (PTE) before the administration of the interview-based Clinician-Administered PTSD Scale.20 Although, this 17-item scale is easily and briefly administered, the downside of the LEC is that it is a yes/no checklist for life-time experiences of traumatic events and it does not question the duration, repetition, or nature of each traumatic event. Also, it has only two items that address adverse life events (“Any event with human suffering” and “Other”).19
The Lifetime Stressor Checklist-Revised (LSC-R) is a 30-item scale for screening and examining DSM-IV traumatic events and other stressful life events.2122 This measure has advantages over the LEC in that it provides a broader area of stressors and more detailed information about the incident including duration (beginning and end of the incident), actual or threatened death or severe injury, subjective reactions and level of distress at the time of trauma, and the negative effect on the person’s life in the past year.21
The present study was conducted to test the psychometric properties of the Korean translated version of the LSC-R in a clinical population. Specifically, we tested the validity of the Korean version of the LSC-R among psychiatric outpatients with anxiety disorders or depressive disorders at a university affiliated medical center.
First-time patients with anxiety or depressive disorders were recruited from a psychiatric outpatient unit at Hanyang University Guri Hospital by consecutive sampling (first come, first serve) during the two-year study period. Either a psychiatric nurse or a psychiatric specialist fully explained the purpose and process of the study and obtained written informed consents from each participant. This study was approved by the Institutional Review Board of the hospital. The inclusion criteria were 1) a current index diagnosis of either an anxiety or depressive disorder according to the Structured Clinical Interview for DSM-IV Axis I Disorders-Clinician Version,23 2) age between 18 and 65 years, and 3) the ability to read and write. The exclusion criteria were 1) intellectual disability, 2) cognitive or neurological diseases, and 3) serious medical condition. In addition, a convenience sample of 50 college students was recruited for test-retest reliability with an interval of three weeks.
The initial eligible subjects were 325 outpatients; 67 patients (29.6%) refused to participate in the research or did not complete the questionnaires, leaving a final of 258 participants. There were no significant differences regarding demographic data and diagnostic distribution between participants and refusers.
PTSD was the most common diagnosis (n=79, 30.6%), followed by major depressive disorder (n=76, 29.5%), panic disorder (n=34, 13.2%), generalized anxiety disorder (n=33, 12.8 %), obsessive-compulsive disorder (n=10, 3.9%), dysthymic disorder (n=9, 3.5%), other anxiety disorder (n=8, 3.1%), social anxiety disorder (n=8, 3.1%), and specific phobias (n=1, 0.4%). Mean age was 39.2 years old (SD=13.3); 65.5% were women; 55.8% were married; 62.8% were religious; 49.6% were high school graduates; and 38.8% were employed (Table 1).
Fifty college students as a convenient sample participated to test temporal stability of the scale, which they completed at two occasions, one at baseline and the other after three weeks. Agreement of endorsement between the time intervals was calculated with kappa statistics (degree of agreement beyond chance) where the value between 0.2–0.4 is considered fair, 0.4–0.6 moderate, 0.6–0.8 substantial, and above 0.8 almost perfect.
The LSC-R covers 29 items of traumatic or stress life events that may happen to the respondent and one item asking if any of these 29 events ever happened to someone close (Table 2). Each item asks about the experience or endorsement of the event in a yes or no format. When the answer is yes, subjects are instructed to complete two to five follow-up questions including 1) age when it started, 2) age when it ended, 3) perceived threat of death or serious injury at the time of trauma, 4) subjective reaction of fear, hopelessness or horror at the time of trauma, and 5) a rating of its negative impact in the past year on a Likert-type scale from 1 (not at all) to 5 (extremely).21 The LSC-R can be scored in three ways: 1) a total sum of endorsed items is used as scores ranging from 0 to 30 (overall life stressor score); 2) a total score based on multiplying subjective rating of the negative effect of each endorsed item (0–150); and 3) a total sum of endorsed items of DSM-IV Criteria A (criterion A stressors) (0–21). In this study, we used the first option for data analysis.
The LSC-R showed good convergent and criterion validity with PTSD symptoms in HIV infected women24 and in those with methadone maintenance treatment.25 In regard to a test-retest reliability study, a modified version of the LSC-R showed an average κ value of 0.59 among 186 women with comorbid substance use and other mental disorders within a period of one week.26
After approval from the original authors, two bilingual mental health professionals translated the LSC-R into Korean. A translation - back translation procedure was not performed.
The LEC is a self-reported questionnaire that screens for 17 PTEs over the patient’s lifetime.19 Each item consists of a yes-or-no checklist for five levels of responses: “happened to me,” “witnessed it,” “learned about it,” “not sure,” and “does not apply,” and two items ask about events happening to others. To converge with the response style of the LSC-R, only the direct experience category was used for analysis in this study. The Korean version used in this study demonstrated acceptable internal consistency and temporal stability, as well as good convergent validity with PTSD, depressive, and anxiety symptoms with a six factor structure, accounting for 57% of variance among psychiatric outpatients.27
The Impact of Event Scale-Revised (IES-R) is a representative self-report tool to evaluate DSM-IV PTSD symptoms.28 Each item asks the respondent how much the person is bothered by the symptom in the past week and indicates a response on a 5-point Likert-type scale from not at all (0) to extremely (4 points). The Korean version of the IES-R displayed good reliability indices and internal consistency (Cronbach alpha=0.83), as well as two week test-retest reliability (r=0.89). It also correlated with other measures of PTSD, depression, and anxiety symptoms among 105 individuals with traumatic events.29
The Zung Self-Rating Depression Scale is a useful tool for screening for depression and measuring affective, physiological, and psychological aspects of depression. This 20-item questionnaire consists of each item in a Likert type response format, ranging from 1 (a little of the time) to 4 (most of the time) points. Thus, total scores can range from 20 to 80.30
The Korean version attained good reliability among 334 adults from the general population with a Cronbach alpha value of 0.84 and test-retest correlation of 0.82 within a five-week interval.31
The Zung Self-Rating Anxiety Scales consists of 20 questions covering different aspects of anxiety, including emotional and somatic anxiety, on a scale with four responses ranging from 1 (almost never) to 4 (all the time) and a total score ranging from 20–80. Reversed items are five.32
Internal consistency of the Korean version had a Cronbach alpha of 0.96 and the 5-week test-retest correlation was 0.98 among 96 patients with an anxiety disorder. The Korean version also showed excellent discriminant validity between patients with anxiety disorder and the normal control group.33
For reliability analysis, three week test-retest reliability was assessed with Cohen’s kappa calculation34 and the internal consistency was evaluated with Cronbach alpha. For the validity analysis, either Spearman or Kendall rank correlation was performed depending on the nature of the variables. Additionally, we performed an exploratory principle component analysis (PCA) with varimax rotation to assess the factorial validity of the scale. The number of factors was determined by the size of the eigenvalues and the amount of variance explained.
To transform the original dichotomous responses into continuous variables, perceived distress from the corresponding event in the range of one to five was used for weighting. For example, when the respondent endorse the experience and distress score during the past year was four, the score four (1×4).
All statistical analyses were conducted with IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY, USA) and the alpha level was set at 0.05 bidirectionally.
For college students, the death of someone close was the most commonly endorsed event (48.0%), followed by the sudden death of someone close (24.0%), witnessing family violence (24.0%), witnessing a serious accident (22.0%), and serious disaster (20.0%). For psychiatric patients, witnessing family violence was most common (42.6%), followed by the sudden death of someone (41.9%), death of someone close (40.7%), and serious financial problems (38.4%) (Table 2).
The three-week temporal stability of the LSC-R is shown in Table 2. The mean value k of 27 items with at least one participant’s endorsement was 0.651. Twenty-two items had an acceptable range of κ (i.e.,>0.4); however, being in foster care (item 6), serious financial problems (item 9), serious physical or mental illness (item 10), emotional neglect, (item 11), and physical assault (item 23) showed Kappa below 0.4 (Table 2).
Internal consistency of the 30 items of the LSC-R was within acceptable limit (Cronbach alpha=0.724).
The convergent validity of the LSC-R was assessed with correlation with corresponding items on the LEC (Table 3). We recoded some items of the LSC-R into clusters of trauma types because items on the LEC are more inclusive; sexual trauma in the LSC-R (any of No. 25, 26, 27, or 28) was significantly correlated with sexual abuse and unwanted sexual experience; physical trauma (any of No. 21, 22, or 23) with physical assault and being attacked by a weapon; a serious disaster (No. 1) among natural disaster, fire, or explosion with witnessing an accident (No. 2) among traffic accidents, other accidents, and toxin exposure; serious accident (No. 3) among traffic accident, other accident, and toxin exposure; sudden death of someone close (No. 17) with death of a loved one; death of someone close (No. 18) with the death of someone close.
The overall score of LSC-R (total number of traumatic events) was significantly correlated with the total score of the LEC (r=0.514, p<0.001), depression (r=0.274, p<0.001), anxiety (r=0.318, p<0.01), PTSD symptom (r=0.415, p<0.001), symptom severity (r=0.376, p<0.001), and economic levels (r=−0.162, p<0.05) (Table 4). However, the LSC-R score was not significantly correlated with sociodemographic variables, such as gender (Spearman’s rho=0.060, p=0.334), age (Spearman’s rho=−0.008, p=0.896), and educational level (Spearman’s rho=−0.059, p=0.349).
Principal component analysis with a varimax rotation was conducted with 30-items of the LSC-R based on a principle of an Eigen-value being larger than one. The analysis extracted 11 factors that explained 64.3% of the total variance. (Table 5): Factor 1, interpersonal trauma (No. 22, 19, 11, 23, and 24); Factor 2, separation (No. 14, 8, and 13); Factor 3, accident or robbery (No. 3, 2, and 21); Factor 4, child sexual violence (No. 27 and 25); Factor 5, loss or familial burden (No. 18, 17, and 16); Factor 6, the financial crisis (No. 9, 1, and 10); Factor 7, adult sexual violence (No. 28 and 26); Factor 8, parental separation (No. 7); Factor 9, handicap of child and physical neglect (No. 15 and 12); Factor 10, learning about the trauma (No. 30); and Factor 11, imprisonment (No. 5 and 4). Items 20 (witnessing robber, mugging, or attack) and 29 (other) had cross-loadings.
In this study, the Korean version of the LSC-R showed sound psychometric properties among outpatients with anxiety or depressive disorders. To our knowledge, this study is the first to examine the factor structure of the LSC-R. We extracted 11 factors representing trauma types, time of experience (child vs. adulthood), and mode of exposure. It is interesting to note that Factor 1 included five diverse types of interpersonal trauma: child physical abuse, witnessing family violence, emotional neglect, adult physical assault, and sexual harassment.
This cluster demonstrated the textbook repetition of interpersonal violence throughout the lifespan, recently known as cumulative abuse or polyvictimization.35 It is interesting to note that sexual harassment clustered within this category of physical and emotional violence rather than child or adult sexual violence. One study of African American female veterans identified a cluster of women whose experience of sexual harassment was more strongly associated with intimate partner violence than sexual violence.36 In fact, the percentage of women belonging to this category was higher than those who had experienced sexual revictimization (26% vs. 22%). In addition, in a study of male and female US veterans, sexual harassment was associated with all types of childhood abuse: sexual, physical, and emotional abuse.37 Our finding also supported the importance of comprehensive lifetime trauma assessment in multiple forms.
Factor 6, financial crisis, involved serious financial problems, serious disaster, and serious physical or mental illness. It is likely that injury/illness and loss of job/personal properties from serious disasters caused by an economic crisis. Financial distress is the most notable post-disaster stressor among older adults after a natural disaster.38
Second, the three-week test-retest reliability for individual items was adequate (κ>0.4) except for four items. The four items of the original version also showed poor temporal stability although items were different from ours. Three of four items were non-traumatic stressors, in part supporting a previous study’s finding that more emotional events have higher temporal stability.39 Further, despite the longer interval of retest in the present study than in the original study (three weeks vs. one week), mean kappa was higher in our findings (0.65 vs. 0.59). It has to be considered that our test-retest sample consisted of younger college students, while the original study involved a clinical population with dual diagnoses.26
A Cronbach alpha of 0.724 was acceptable but lower than usually expected for a psychological instrument. This is probably due to the dichotomous response set of the scale itself. For example, the internal consistency of the LEC was 0.67 lower than that of this study.27 The Korean version of the LSC-R correlated well with individual items of the LEC, the only validated measure for PTE in the Korean language. Concurrent validity was demonstrated with correlations with theoretically associated common symptoms of traumatic reaction including PTSD, depression, and anxiety.2
The limitation of this study should be noted. First, the LEC used for concurrent validity has only 17 items and we were not able to test each item of the LSC-R. Because the LEC covers DSM-IV traumatic events, the remaining untested items are traumatic events that cannot be defined by the DSM and non-traumatic stressors. Second, the Korean version in this study did not undergo a back-translation process. However, the LSC-R contains behavior-specific items with factual content and thus, the space for error in translation will be narrower than those questionnaires inquiring about symptoms or psychological reactions. In addition, there is also research supporting the skipping of reverse translation because it is not related to the quality of translated scales.40 Third, test-retest reliability was tested with non-clinical population.
Despite these limitations, this study demonstrated acceptable reliability and good validity of the Korean version of the LSC-R, supporting its use in filtering out PTE among a Korean speaking clinical population. Future research is needed to test the reliability and validity of the scale for the general population. Our results also support the need to assess the multiple traumatic and stressful experiences that occur across the patient’s lifespan, especially in regard to those events of an interpersonal nature.
Figures and Tables
Table 1
General Characteristics of the Outpatients with Anxiety or Depressive Disorder (n=258)

Table 2
The Test-Retest Reliability* of the Life Stressor Checklist-Revised and Frequency of Traumatic Events

Table 3
Correlation between Items of the Life Stressor Checklist-Revised (LSCR) and the Life Events Checklist (LEC)

Table 4
Correlation among the Number of Traumatic Events on the LSCR and the Scores of Other Scales
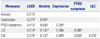
| Measures | LSCR | Anxiety | Depression | PTSD symptoms | LEC |
|---|---|---|---|---|---|
| Anxiety | 0.318† | ||||
| Depression | 0.274‡ | 0.581‡ | |||
| PTSD symptoms | 0.415‡ | 0.506‡ | 0.392‡ | ||
| LEC | 0.514‡ | 0.142* | 0.084 | 0.308‡ | |
| GSI | 0.376‡ | 0.727‡ | 0.405‡ | 0.529‡ | 0.275‡ |
LSCR, Life Stressor Checklist-Revised; PTSD, posttraumatic stress disorder; LEC, Life Event Checklist; GSI, Global Severity Index.
Correlation coefficient is Spearman’s rho. Anxiety is measured by Zung Self-Rating Anxiety Scale; Depression by Zung Self-Rating Depression Scale; Post-traumatic symptoms by Impact of Events Scale.
*p<0.05, †p<0.01, ‡p<0.001.
Table 5
Principal Component Analysis of the Life Stressor Checklist-Revised in outpatients (n=258)

ACKNOWLEDGEMENTS
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HM15C1058).
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorder. 3rd ed. Washington, DC: American Psychiatric Association Press;1987.
2. Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998; 55:626–632.

3. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995; 52:1048–1060.

4. American Psychiatric Association. Diagnotic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association Press;2013.
5. Santiago PN, Ursano RJ, Gray CL, Pynoos RS, Spiegel D, Lewis-Fernandez R, et al. A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: intentional and non-intentional traumatic events. PLoS One. 2013; 8:e59236.

6. Backholm K, Isomaa R, Birgegård A. The prevalence and impact of trauma history in eating disorder patients. Eur J Psychotraumatol. 2013; 11. 20. [Epub]. DOI: 10.3402/ejpt.v4i0.22482.

7. Brown RJ, Schrag A, Trimble MR. Dissociation, childhood interpersonal trauma, and family functioning in patients with somatization disorder. Am J Psychiatry. 2005; 162:899–905.

8. Kelleher I, Keeley H, Corcoran P, Ramsay H, Wasserman C, Carli V, et al. Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. Am J Psychiatry. 2013; 170:734–741.

9. Sar V, Akyüz G, Kundakçi T, Kiziltan E, Dogan O. Childhood trauma, dissociation, and psychiatric comorbidity in patients with conversion disorder. Am J Psychiatry. 2004; 161:2271–2276.

10. Shea MT, Zlotnick C, Weisberg RB. Commonality and specificity of personality disorder profiles in subjects with trauma histories. J Pers Disord. 1999; 13:199–210.

11. Vrshek-Schallhorn S, Wolitzky-Taylor K, Doane LD, Epstein A, Sumner JA, Mineka S, et al. Validating new summary indices for the Childhood Trauma Interview: associations with first onsets of major depressive disorder and anxiety disorders. Psychol Assess. 2014; 26:730–740.

12. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998; 14:245–258.

13. Anda RF, Brown DW, Dube SR, Bremner JD, Felitti VJ, Giles WH. Adverse childhood experiences and chronic obstructive pulmonary disease in adults. Am J Prev Med. 2008; 34:396–403.

14. Brown DW, Anda RF, Felitti VJ, Edwards VJ, Malarcher AM, Croft JB, et al. Adverse childhood experiences are associated with the risk of lung cancer: a prospective cohort study. BMC Public Health. 2010; 10:20.

15. Keyes KM, McLaughlin KA, Demmer RT, Cerdá M, Koenen KC, Uddin M, et al. Potentially traumatic events and the risk of six physical health conditions in a population-based sample. Depress Anxiety. 2013; 30:451–460.

16. Elhai JD, Gray MJ, Kashdan TB, Franklin CL. Which instruments are most commonly used to assess traumatic event exposure and posttraumatic effects?: a survey of traumatic stress professionals. J Trauma Stress. 2005; 18:541–545.

17. Goodman LA, Corcoran C, Turner K, Yuan N, Green BL. Assessing traumatic event exposure: general issues and preliminary findings for the Stressful Life Events Screening Questionnaire. J Trauma Stress. 1998; 11:521–542.

18. Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychol Assess. 2000; 12:210–224.

19. Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004; 11:330–341.

20. Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. J Trauma Stress. 1995; 8:75–90.

21. Wolfe J, Kimerling R, Brown PJ, Chrestman KR, Levin K. Psychometric review of the life stressor checklist-revised. In : Stamm BH, editor. Measurement of Stress, Trauma, and Adaptation. Lutherville, MD: Sidran Press;1996. p. 198–201.
22. Wolfe J, Kimerling R. Gender issues in the assessment of posttraumatic stress disorder. In : Wilson J, Keane TM, editors. Assessing psychologicla trauma and PTSD. New York: Guildford Press;1997.
23. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders-Clinician Version (SCID-CV). Washington, DC: American Psychiatric Association Press;1997.
24. Kimerling R, Calhoun KS, Forehand R, Armistead L, Morse E, Morse P, et al. Traumatic stress in HIV-infected women. AIDS Educ Prev. 1999; 11:321–330.
25. Himelhoch S, Weber E, Medoff D, Charlotte M, Clayton S, Wilson C, et al. Posttraumatic stress disorder and one-year outcome in methadone maintenance treatment. Am J Addict. 2012; 21:524–530.

26. McHugo GJ, Caspi Y, Kammerer N, Mazelis R, Jackson EW, Russell L, et al. The assessment of trauma history in women with co-occurring substance abuse and mental disorders and a history of interpersonal violence. J Behav Health Serv Res. 2005; 32:113–127.

27. Bae H, Kim D, Koh H, Kim Y, Park JS. Psychometric properties of the life events checklist-Korean version. Psychiatry Investig. 2008; 5:163–167.

28. Weiss DF, Marmer CR. The Impact of Event Scale-Revised. In : Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD: a practitioners handbook. New York: Guilford Press;1997. p. 399–411.
29. Eun HJ, Kwon TW, Lee SM, Kim TH, Choi MR, Cho SJ. A study on reliability and validity of the Korean version of impact of event scale-revised. J Korean Neuropsychiatr Assoc. 2005; 44:303–310.
31. Lee JH. Development of the Korean form of Zung’s self-rating depression scale. Yeungnam Univ J Med. 1995; 12:292–305.

33. Lee JH. Development of the Korean form of Zung’s self-rating anxiety scale. Yeungnam Univ J Med. 1996; 13:279–294.

34. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.

35. Scott-Storey K. Cumulative abuse: do things add up? An evaluation of the conceptualization, operationalization, and methodological approaches in the study of the phenomenon of cumulative abuse. Trauma Violence Abuse. 2011; 12:135–150.

36. Campbell R, Greeson MR, Bybee D, Raja S. The co-occurrence of childhood sexual abuse, adult sexual assault, intimate partner violence, and sexual harassment: a mediational model of posttraumatic stress disorder and physical health outcomes. J Consult Clin Psychol. 2008; 76:194–207.

37. Rosen LN, Martin L. Childhood maltreatment history as a risk factor for sexual harassment among U.S. Army soldiers. Violence Vict. 1998; 13:269–286.

38. Pietrzak RH, Feder A, Singh R, Schechter CB, Bromet EJ, Katz CL, et al. Trajectories of PTSD risk and resilience in World Trade Center responders: an 8-year prospective cohort study. Psychol Med. 2014; 44:205–219.

39. van Giezen AE, Arensman E, Spinhoven P, Wolters G. Consistency of memory for emotionally arousing events: a review of prospective and experimental studies. Clin Psychol Rev. 2005; 25:935–953.

40. Perneger TV, Leplège A, Etter JF. Cross-cultural adaptation of a psychometric instrument: two methods compared. J Clin Epidemiol. 1999; 52:1037–1046.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download